Centres Of Excellence
Our Centres of Excellence bring together multidisciplinary teams to deliver precise diagnosis, advanced treatments, and superior outcomes across a wide spectrum of medical specialties.

Related Links
Doctors For Treatment in Similar Locations
Treatments in India for Visitors
Best Hospital Near by for treatment
Related Links
Doctors For Treatment in Similar Locations
Treatments in India for Visitors
- Cardiac Care Treatment in Hyderabad for Bangladesh
- Cardiac Care Treatment in Chennai for Ethiopia
- Cardiac Care Treatment in Mumbai for Ethiopia
- Cardiac Care Treatment in Gurugram for Iraq
- Cardiac Care Treatment in Mumbai for Iraq
- Cardiac Care Treatment in Mumbai for Nigeria
- Cardiac Care Treatment in Bengaluru for Ethiopia
- Cardiac Care Treatment in Chennai for Iraq
- Cardiac Care Treatment in Hyderabad for UAE
- Cardiac Care Treatment in Mumbai for Bangladesh
- Cardiac Care Treatment in Bengaluru for Iraq
- Cardiac Care Treatment in Chennai for Nigeria
- Cardiac Care Treatment in Pune for Bangladesh
- Cardiac Care Treatment in Bengaluru for Bangladesh
- Cardiac Care Treatment in Hyderabad for Ethiopia
- Cardiac Care Treatment in Hyderabad for Iraq
- Cardiac Care Treatment in Pune for UAE
- Cardiac Care Treatment in New Delhi for UAE
- Cardiac Care Treatment in New Delhi for Bangladesh
- Cardiac Care Treatment in Gurugram for Nigeria
- Cardiac Care Treatment in Bengaluru for Nigeria
- Cardiac Care Treatment in Hyderabad for Nigeria
- Cardiac Care Treatment in India for Bangladesh
- Cardiac Care Treatment in Gurugram for Ethiopia
- Cardiac Care Treatment in Pune for Ethiopia
- Cardiac Care Treatment in New Delhi for Ethiopia
- Cardiac Care Treatment in Pune for Nigeria
- Cardiac Care Treatment in India for Ethiopia
- Cardiac Care Treatment in New Delhi for Iraq
- Cardiac Care Treatment in Gurugram for UAE
- Cardiac Care Treatment in India for UAE
- Cardiac Care Treatment in Chennai for UAE
- Cardiac Care Treatment in Bengaluru for UAE
- Cardiac Care Treatment in Mumbai for UAE
- Cardiac Care Treatment in Gurugram for Bangladesh
- Cardiac Care Treatment in India for Iraq
- Cardiac Care Treatment in India for Nigeria
Best Hospital Near by for treatment
Related Links
- Cardiac Care cost in Haryana
- Cardiac Care cost in Hyderabad
- Cardiac Care cost in Mumbai
- Cardiac Care cost in India
- Cardiac Care cost in Bengaluru
- Cardiac Care cost in New Delhi
- Cardiac Care Success Rate in New Delhi
- Cardiac Care Success Rate in India
- Cardiac Care cost in Chennai
- Cardiac Care Success Rate in Pune
- Cardiac Care Success Rate in Mumbai
- Cardiac Care Success Rate in Hyderabad
Related Treatments

structural heart
Treatment Price
$15000.00 USDStructural heart disease encompasses a range of conditions affecting the heart's non-coronary structures. Treatment goals include correcting anatomical defects, alleviating symptoms, and preventing progressive heart damage. Modern techniques often involve catheter-based interventions (e.g., TAVI, MitraClip, PFO/ASD closure) that offer quicker recovery times compared to traditional open-heart surgery, ensuring safety and efficacy.
Structural heart disease encompasses a range of conditions affecting the heart's non-coronary structures. Treatment goals include correcting anatomical defects, alleviating symptoms, and preventing progressive heart damage. Modern techniques often involve catheter-based interventions (e.g., TAVI, MitraClip, PFO/ASD closure) that offer quicker recovery times compared to traditional open-heart surgery, ensuring safety and efficacy.
Treatment Overview
<p>Structural heart disease encompasses a range of conditions affecting the heart's non-coronary structures. Treatment goals include correcting anatomical defects, alleviating symptoms, and preventing progressive heart damage. Modern techniques often involve catheter-based interventions (e.g., TAVI, MitraClip, PFO/ASD closure) that offer quicker recovery times compared to traditional open-heart surgery, ensuring safety and efficacy.</p>
Procedures
Structural heart procedures vary significantly based on the condition being treated. For valvular diseases, common procedures include: * **Transcatheter Aortic Valve Implantation (TAVI/TAVR):** A minimally invasive procedure to replace a diseased aortic valve. A catheter, usually inserted through an artery in the leg (femoral artery), delivers a new collapsible valve to the heart. The new valve expands and takes over the function of the old, diseased valve. * **MitraClip Procedure:** Used to repair a leaky mitral valve (mitral regurgitation). A catheter is guided through a vein in the groin to the heart. A small clip is then used to grasp the two leaflets of the mitral valve, improving their closure and reducing regurgitation. * **Percutaneous Septal Defect Closure (ASD/PFO Closure):** For congenital heart defects like Atrial Septal Defect (ASD) or Patent Foramen Ovale (PFO), a catheter delivers a small device (e.g., an occluder) to close the hole between the heart's upper chambers. This prevents abnormal blood flow and reduces the risk of stroke. For each procedure, real-time imaging (e.g., echocardiography, fluoroscopy) is used to guide the catheter and device placement, ensuring precision and safety. The specific steps depend on the access site and the device used.
Benefits
<h2>Benefits of Modern Structural Heart Treatment</h2><ul><li><h3>Improved Quality of Life</h3><p>Alleviates symptoms like shortness of breath, fatigue, and chest pain, allowing patients to resume daily activities with renewed energy.</p></li><li><h3>Minimally Invasive Options</h3><p>Many procedures, such as TAVI and MitraClip, are catheter-based, meaning smaller incisions, less pain, reduced hospital stays, and faster recovery compared to open-heart surgery.</p></li><li><h3>High Success Rates</h3><p>Advanced techniques and expert cardiologists contribute to excellent clinical outcomes and improved long-term prognosis.</p></li><li><h3>Prevention of Further Complications</h3><p>Correcting structural defects reduces the risk of serious issues like heart failure, stroke, and other cardiovascular events.</p></li><li><h3>Personalized Care</h3><p>Treatment plans are tailored to individual patient needs, ensuring the most effective and safest approach for their specific condition.</p></li></ul>
Recovery Information
<h2>Structural Heart Treatment Recovery Time and Tips</h2><ul><li><h3>Immediate Post-Procedure (1-3 days)</h3><p>For catheter-based interventions (TAVI, MitraClip, ASD/PFO closure), patients often spend 1-2 days in the ICU/recovery unit followed by a few days in a regular hospital room. Early mobilization is encouraged.</p></li><li><h3>Short-Term Recovery (1-4 weeks)</h3><p>Most patients can return to light activities within 1-2 weeks. Full recovery for minimally invasive procedures typically takes 2-4 weeks. For traditional open-heart surgery, this phase might extend to 4-6 weeks.</p></li><li><h3>Long-Term Recovery & Rehabilitation</h3><p>Cardiac rehabilitation is often recommended to strengthen the heart and improve overall cardiovascular health. This includes supervised exercise, dietary counseling, and lifestyle modifications. Regular follow-ups with your cardiologist are crucial to monitor progress and ensure long-term well-being.</p></li><li><h3>Recovery Tips:</h3><ul><li>Follow all medication instructions diligently.</li><li>Engage in gentle, progressive physical activity as advised by your doctor.</li><li>Maintain a heart-healthy diet.</li><li>Avoid heavy lifting or strenuous activities during the initial recovery period.</li><li>Attend all scheduled follow-up appointments.</li><li>Seek emotional support if needed; recovery can be a challenging process.</li></ul></li></ul>

robotic cardiac surgery
Treatment Price
$0.00 USDNo overview available
No overview available
Treatment Overview
No overview available
Procedures
No procedure details available
Benefits
No benefits information available
Recovery Information
No recovery information available

congenital heart surgery
Treatment Price
$8500.00 USDCongenital heart surgery encompasses a range of intricate procedures designed to repair congenital heart defects (CHDs), which can affect heart walls, valves, or blood vessels. The goal is to restore normal blood flow, prevent complications like heart failure or pulmonary hypertension, and ensure healthy development. Techniques vary from minimally invasive catheter-based interventions to complex open-heart surgeries, tailored to each patient's unique condition and age.
Congenital heart surgery encompasses a range of intricate procedures designed to repair congenital heart defects (CHDs), which can affect heart walls, valves, or blood vessels. The goal is to restore normal blood flow, prevent complications like heart failure or pulmonary hypertension, and ensure healthy development. Techniques vary from minimally invasive catheter-based interventions to complex open-heart surgeries, tailored to each patient's unique condition and age.
Treatment Overview
Congenital heart surgery encompasses a range of intricate procedures designed to repair congenital heart defects (CHDs), which can affect heart walls, valves, or blood vessels. The goal is to restore normal blood flow, prevent complications like heart failure or pulmonary hypertension, and ensure healthy development. Techniques vary from minimally invasive catheter-based interventions to complex open-heart surgeries, tailored to each patient's unique condition and age.
Procedures
Congenital heart surgery procedures vary greatly based on the specific defect. For open-heart surgery, an incision is made in the chest (often through the breastbone), and the patient is placed on a heart-lung bypass machine to maintain blood circulation and oxygenation while the surgeon repairs the heart. This can involve patching holes (e.g., VSD, ASD closure), widening narrowed vessels (e.g., coarctation repair), replacing or repairing valves, or rerouting blood vessels (e.g., Tetralogy of Fallot repair, arterial switch for TGA). Minimally invasive techniques or catheter-based interventions may involve smaller incisions or catheters inserted through blood vessels to access the heart. After repair, the heart-lung machine is removed, and the chest is closed. Post-procedure, patients are transferred to ICU for critical monitoring.
Benefits
<h3>Benefits of Congenital Heart Surgery</h3><ul><li><strong>Improved Heart Function:</strong> Correction of defects restores normal blood flow and pumping efficiency.</li><li><strong>Enhanced Quality of Life:</strong> Reduced symptoms like breathlessness, fatigue, and cyanosis, leading to increased activity levels.</li><li><strong>Prevention of Complications:</strong> Minimizes risks of heart failure, pulmonary hypertension, stroke, and developmental delays.</li><li><strong>Increased Life Expectancy:</strong> For many defects, surgery offers a chance for a normal lifespan.</li><li><strong>Better Growth and Development:</strong> Especially crucial for infants and children, ensuring they meet developmental milestones.</li><li><strong>Reduced Medication Dependency:</strong> Successful surgery can often decrease the need for ongoing heart medications.</li></ul>
Recovery Information
<h3>Congenital Heart Surgery Recovery Time and Tips</h3><ul><li><strong>Initial Hospital Stay:</strong> Typically 5-10 days, including time in the Intensive Care Unit (ICU) for close monitoring after surgery. More complex cases, especially in infants, may require longer stays.</li><li><strong>Post-Discharge Recovery:</strong> Full recovery at home can take several weeks to a few months (e.g., 4-8 weeks for children, longer for adults or complex cases). Activity restrictions, such as avoiding heavy lifting and strenuous exercise, are common.</li><li><strong>Pain Management:</strong> Mild to moderate pain is expected and managed with prescribed medication.</li><li><strong>Wound Care:</strong> Keeping the incision clean and dry is vital to prevent infection.</li><li><strong>Diet and Nutrition:</strong> A balanced diet supports healing. For infants, feeding may need careful monitoring.</li><li><strong>Follow-up Care:</strong> Regular appointments with a cardiologist are essential to monitor heart function and recovery progress.</li><li><strong>Emotional Support:</strong> Both patients and families may benefit from psychological support to cope with the stress of surgery and recovery.</li><li><strong>Physical Therapy:</strong> May be recommended to gradually rebuild strength and endurance.</li></ul>

angiography
Treatment Price
$1500.00 USDThe primary goal of angiography is to accurately diagnose vascular conditions affecting the heart, brain, kidneys, and limbs. It's crucial for planning interventions like angioplasty or stent placement. Techniques involve inserting a thin catheter, usually through the groin or wrist, guiding it to the target vessel, and releasing a dye visible under X-ray, providing real-time images of blood flow and vessel structure. DivinHeal connects you with highly experienced interventional cardiologists and radiologists for safe and precise angiography.
The primary goal of angiography is to accurately diagnose vascular conditions affecting the heart, brain, kidneys, and limbs. It's crucial for planning interventions like angioplasty or stent placement. Techniques involve inserting a thin catheter, usually through the groin or wrist, guiding it to the target vessel, and releasing a dye visible under X-ray, providing real-time images of blood flow and vessel structure. DivinHeal connects you with highly experienced interventional cardiologists and radiologists for safe and precise angiography.
Treatment Overview
<p>The primary goal of angiography is to accurately diagnose vascular conditions affecting the heart, brain, kidneys, and limbs. It's crucial for planning interventions like angioplasty or stent placement. Techniques involve inserting a thin catheter, usually through the groin or wrist, guiding it to the target vessel, and releasing a dye visible under X-ray, providing real-time images of blood flow and vessel structure. DivinHeal connects you with highly experienced interventional cardiologists and radiologists for safe and precise angiography.</p>
Procedures
<h3>How Angiography is Performed</h3><ul><li><strong>Preparation:</strong> Patients fast for 6-8 hours. Medications are reviewed, especially blood thinners. An IV line is established, and mild sedation is often given. The access site (usually groin or wrist) is sterilized and numbed with local anesthetic.</li><li><strong>Catheter Insertion:</strong> A small incision is made, and a guide wire is inserted into an artery or vein, followed by a sheath (hollow tube).</li><li><strong>Catheter Advancement:</strong> A thin catheter is threaded through the sheath and guided to the target vessel under real-time X-ray (fluoroscopy) guidance.</li><li><strong>Contrast Injection:</strong> An iodine-based contrast dye is injected through the catheter, making the blood vessels visible on the X-ray monitor. Patients may feel a warm sensation.</li><li><strong>Image Acquisition:</strong> Multiple X-ray images are taken from different angles to capture detailed views of blood flow and vessel structure.</li><li><strong>Intervention (Optional):</strong> If blockages are found, procedures like angioplasty or stent placement may be performed immediately.</li><li><strong>Catheter Removal & Closure:</strong> After imaging/intervention, the catheter and sheath are removed. Pressure is applied to the puncture site, or a closure device is used, followed by a dressing.</li></ul>
Benefits
<h2>Benefits of Angiography</h2><ul><li><strong>Accurate Diagnosis:</strong> Provides precise visualization of blood vessels, crucial for diagnosing conditions like blockages, aneurysms, and malformations.</li><li><strong>Minimally Invasive:</strong> Generally involves only a small puncture site, leading to less pain and quicker recovery compared to open surgery.</li><li><strong>Immediate Intervention:</strong> Allows for therapeutic procedures like angioplasty or stent placement to be performed during the same session if needed.</li><li><strong>Real-time Imaging:</strong> Offers dynamic views of blood flow, enabling physicians to make informed decisions.</li><li><strong>Reduced Risk of Major Surgery:</strong> By accurately identifying issues, it can often prevent or postpone more invasive surgical interventions.</li><li><strong>Improved Outcomes:</strong> Early and accurate diagnosis through angiography leads to timely treatment, significantly improving patient outcomes for cardiovascular and other vascular diseases.</li></ul>
Recovery Information
<h2>Angiography Recovery Time and Tips</h2><h3>Immediate Post-Procedure Care</h3><p>After your angiography, you'll typically spend several hours in a recovery room. The primary focus will be on monitoring the insertion site for bleeding or swelling and ensuring your vital signs are stable. You will be asked to lie flat for a few hours, especially if the groin was used, to prevent complications.</p><h3>Recovery at Home</h3><ul><li><strong>Rest:</strong> Plan for at least 24-48 hours of rest post-procedure. Avoid strenuous activities, heavy lifting, and intense exercise for about a week.</li><li><strong>Hydration:</strong> Drink plenty of fluids to help flush the contrast dye from your system.</li><li><strong>Wound Care:</strong> Keep the puncture site clean and dry. You'll receive specific instructions on when you can shower and how to identify signs of infection.</li><li><strong>Medication:</strong> Take any prescribed medications, such as blood thinners, exactly as directed by your doctor.</li><li><strong>Monitoring:</strong> Watch for any signs of complications like persistent bleeding, severe pain, numbness, coolness, or discoloration in the limb where the catheter was inserted.</li></ul><h3>When to Seek Medical Attention</h3><p>Contact your doctor immediately if you experience:</p><ul><li>Sudden swelling or bruising at the puncture site.</li><li>Bleeding that doesn't stop with direct pressure.</li><li>Fever or chills.</li><li>New or worsening chest pain or shortness of breath.</li><li>Numbness, tingling, or weakness in the affected limb.</li></ul><p>Most patients can return to light activities within a few days and full activities within a week. DivinHeal’s care coordinators will provide detailed <a href="#" target="_blank">angiography recovery time and tips</a>, ensuring you have all the support needed for a smooth and comfortable recuperation.</p>

heart failure surgery
Treatment Price
$6000.00 USDOverview of Heart Failure Surgery Treatment
Restoring Cardiac Function and Quality of Life
Heart failure surgery treatment aims to address the underlying structural or functional issues causing the heart to fail in its pumping ability. Depending on the specific diagnosis, techniques can range from revascularization procedures like CABG to complex valve corrections, or the implantation of mechanical support devices (VADs) to aid a weakened heart. For end-stage heart failure, a heart transplant may be considered. Our goal is to enhance the heart's efficiency, reduce symptoms, and significantly improve a patient's longevity and quality of life.
Overview of Heart Failure Surgery Treatment
Restoring Cardiac Function and Quality of Life
Heart failure surgery treatment aims to address the underlying structural or functional issues causing the heart to fail in its pumping ability. Depending on the specific diagnosis, techniques can range from revascularization procedures like CABG to complex valve corrections, or the implantation of mechanical support devices (VADs) to aid a weakened heart. For end-stage heart failure, a heart transplant may be considered. Our goal is to enhance the heart's efficiency, reduce symptoms, and significantly improve a patient's longevity and quality of life.
Treatment Overview
<h2>Overview of Heart Failure Surgery Treatment</h2><h3>Restoring Cardiac Function and Quality of Life</h3><p>Heart failure surgery treatment aims to address the underlying structural or functional issues causing the heart to fail in its pumping ability. Depending on the specific diagnosis, techniques can range from revascularization procedures like CABG to complex valve corrections, or the implantation of mechanical support devices (VADs) to aid a weakened heart. For end-stage heart failure, a heart transplant may be considered. Our goal is to enhance the heart's efficiency, reduce symptoms, and significantly improve a patient's longevity and quality of life.</p>
Procedures
The specific steps of heart failure surgery treatment vary significantly based on the chosen procedure. For example, during a Coronary Artery Bypass Grafting (CABG), the surgeon makes an incision in the chest, opens the sternum, and uses a heart-lung machine. Grafts (blood vessels from other parts of the body, like the leg or chest wall) are then attached to bypass the blocked coronary arteries. For heart valve repair or replacement, the damaged valve is either reshaped and repaired using rings or patches, or it is removed and replaced with a mechanical or biological prosthesis. Ventricular Assist Device (VAD) implantation involves surgically attaching the VAD to the heart's ventricles and aorta, with a driveline exiting the body to connect to an external battery and controller. Heart transplantation is a complex procedure where the diseased heart is removed and replaced with a healthy donor heart. All these procedures require meticulous surgical skill, advanced cardiac monitoring, and a dedicated team of anesthesiologists, perfusionists, and nurses. Post-surgery, patients are monitored closely in the ICU to manage pain, fluid balance, and cardiac function.
Benefits
<h2>Benefits of Heart Failure Surgery Treatment</h2><h3>A New Lease on Life</h3><ul><li><strong>Improved Cardiac Function:</strong> Surgical interventions can significantly enhance the heart's ability to pump blood effectively, reducing symptoms and improving overall health.</li><li><strong>Symptom Relief:</strong> Patients often experience a dramatic reduction in debilitating symptoms like shortness of breath, fatigue, and swelling, leading to a better quality of life.</li><li><strong>Increased Longevity:</strong> Addressing the underlying cause of heart failure through surgery can extend life expectancy and prevent further cardiac complications.</li><li><strong>Enhanced Quality of Life:</strong> With improved heart function, patients can often return to many daily activities, hobbies, and enjoy a more active, fulfilling life.</li><li><strong>Reduced Hospitalizations:</strong> Successful surgery can decrease the frequency of hospital admissions related to heart failure exacerbations.</li><li><strong>Advanced Technological Care:</strong> Access to state-of-the-art surgical techniques and devices, including minimally invasive options where applicable, through DivinHeal's network.</li></ul>
Recovery Information
<h2>Recovery and Life After Heart Failure Surgery Treatment</h2><h3>Your Path to a Stronger Heart</h3><ul><li><strong>Immediate Post-Operative Period:</strong> Patients typically spend a few days in the Intensive Care Unit (ICU) for close monitoring, followed by a stay in a regular hospital room. Pain management and early mobilization are crucial.</li><li><strong>Hospital Stay Duration:</strong> The average hospital stay for heart failure surgery is usually 7-10 days, depending on the complexity of the procedure and individual recovery progress.</li><li><strong>Initial Home Recovery (First 4-6 Weeks):</strong> During this period, patients are advised to rest, avoid heavy lifting, and gradually increase activity levels as guided by their medical team. Wound care is essential.</li><li><strong>Cardiac Rehabilitation:</strong> A vital component of recovery, cardiac rehab programs involve supervised exercise, education on heart-healthy living, and emotional support. This typically begins a few weeks post-surgery and can last several months.</li><li><strong>Long-Term Lifestyle Adjustments:</strong> Adopting a heart-healthy diet, regular moderate exercise, stress management, and strict adherence to medication regimens are crucial for long-term success and preventing recurrence.</li><li><strong>Emotional Support:</strong> It's normal to experience emotional challenges during recovery. DivinHeal's network can connect patients with counseling and support groups to aid mental well-being.</li></ul><p>DivinHeal's dedicated care coordinators provide continuous support throughout your recovery, ensuring you have access to the best post-operative care and rehabilitation resources.</p>

interventional cardiology
Treatment Price
$4500.00 USDInterventional cardiology focuses on using advanced catheterization techniques to effectively manage complex heart conditions. The primary goal is to open blocked arteries, repair dysfunctional valves, or close congenital heart defects, thereby preventing heart attacks, strokes, and improving patient quality of life. DivinHeal connects you with world-class cardiac specialists and state-of-the-art facilities for optimal outcomes.
Interventional cardiology focuses on using advanced catheterization techniques to effectively manage complex heart conditions. The primary goal is to open blocked arteries, repair dysfunctional valves, or close congenital heart defects, thereby preventing heart attacks, strokes, and improving patient quality of life. DivinHeal connects you with world-class cardiac specialists and state-of-the-art facilities for optimal outcomes.
Treatment Overview
Interventional cardiology focuses on using advanced catheterization techniques to effectively manage complex heart conditions. The primary goal is to open blocked arteries, repair dysfunctional valves, or close congenital heart defects, thereby preventing heart attacks, strokes, and improving patient quality of life. DivinHeal connects you with world-class cardiac specialists and state-of-the-art facilities for optimal outcomes.
Procedures
A typical interventional cardiology procedure, such as coronary angioplasty and stenting, begins with the patient receiving local anesthesia at the access site (usually the groin or wrist). A thin, flexible guide wire is then inserted into an artery and carefully threaded up to the heart. A catheter with a balloon at its tip is advanced over the guide wire to the narrowed section of the coronary artery. The balloon is inflated to compress the plaque against the artery walls, widening the artery. In most cases, a stent (a small mesh tube) is then deployed to keep the artery open. The balloon and catheter are removed, leaving the stent in place. The access site is then closed, and pressure is applied to prevent bleeding.
Benefits
<h2>Benefits of Interventional Cardiology Treatment</h2><ul><li><strong>Minimally Invasive:</strong> Most procedures involve small incisions, leading to less pain and scarring.</li><li><strong>Faster Recovery:</strong> Patients often experience shorter hospital stays and quicker return to daily activities compared to open-heart surgery. See <a href="#">interventional cardiology recovery time and tips</a> for more.</li><li><strong>High Success Rates:</strong> Advanced techniques and skilled cardiologists lead to excellent outcomes in restoring heart function. Refer to <a href="#">interventional cardiology success rate</a> for details.</li><li><strong>Improved Quality of Life:</strong> Alleviates symptoms like chest pain, shortness of breath, and fatigue, significantly enhancing patient well-being.</li><li><strong>Prevention of Future Cardiac Events:</strong> Effectively treats blockages and defects, reducing the risk of heart attacks and strokes.</li></ul>
Recovery Information
<h2>Interventional Cardiology Recovery Time and Tips</h2><p>Recovery after interventional cardiology varies based on the specific procedure and individual patient factors, but it is generally much quicker than traditional surgery. For common procedures like angioplasty and stenting, patients may be discharged within 1-2 days. Full recovery and return to normal activities typically take 1-2 weeks. <a href="#">Interventional cardiology recovery time and tips</a> include:</p><ul><li><strong>Initial Rest:</strong> Rest for 24-48 hours after discharge, especially at the access site (groin or wrist).</li><li><strong>Medication Adherence:</strong> Strictly follow prescribed medications, particularly antiplatelet drugs, to prevent clot formation.</li><li><strong>Lifestyle Modifications:</strong> Adopt a heart-healthy diet, regular light exercise (as advised by your doctor), quit smoking, and manage stress.</li><li><strong>Cardiac Rehabilitation:</strong> Participate in supervised exercise and education programs to strengthen your heart and improve overall health.</li><li><strong>Follow-up Appointments:</strong> Regular check-ups with your cardiologist are crucial to monitor progress and address any concerns.</li><li><strong>Avoid Heavy Lifting:</strong> For a few weeks, avoid strenuous activities or heavy lifting to protect the access site.</li></ul>

cardiac surgery
Treatment Price
$5500.00 USDCardiac surgery involves a range of complex procedures designed to correct structural heart problems, improve blood flow, and repair damaged heart tissue. The primary goals of cardiac surgery are to alleviate debilitating symptoms, prevent life-threatening complications, and enhance the overall health and longevity of patients. Techniques vary from traditional open-heart surgery, requiring a sternotomy, to minimally invasive approaches and even robotic-assisted procedures, offering reduced recovery times and smaller scars. DivinHeal provides access to leading cardiac surgeons and state-of-the-art technology for every type of cardiac surgery treatment.
Cardiac surgery involves a range of complex procedures designed to correct structural heart problems, improve blood flow, and repair damaged heart tissue. The primary goals of cardiac surgery are to alleviate debilitating symptoms, prevent life-threatening complications, and enhance the overall health and longevity of patients. Techniques vary from traditional open-heart surgery, requiring a sternotomy, to minimally invasive approaches and even robotic-assisted procedures, offering reduced recovery times and smaller scars. DivinHeal provides access to leading cardiac surgeons and state-of-the-art technology for every type of cardiac surgery treatment.
Treatment Overview
Cardiac surgery involves a range of complex procedures designed to correct structural heart problems, improve blood flow, and repair damaged heart tissue. The primary goals of cardiac surgery are to alleviate debilitating symptoms, prevent life-threatening complications, and enhance the overall health and longevity of patients. Techniques vary from traditional open-heart surgery, requiring a sternotomy, to minimally invasive approaches and even robotic-assisted procedures, offering reduced recovery times and smaller scars. DivinHeal provides access to leading cardiac surgeons and state-of-the-art technology for every type of cardiac surgery treatment.
Procedures
Cardiac surgery procedures vary widely, but a typical open-heart surgery, such as a Coronary Artery Bypass Graft (CABG), generally involves these steps: 1. **Anesthesia:** The patient is given general anesthesia to ensure they are unconscious and pain-free throughout the procedure. 2. **Incision:** A long incision is made down the center of the chest, and the sternum (breastbone) is carefully divided to expose the heart. 3. **Cardiopulmonary Bypass:** The heart is stopped, and a heart-lung machine takes over the functions of circulating and oxygenating the blood. This allows the surgeon to operate on a still, bloodless heart. 4. **Repair/Replacement:** The specific repair is performed, such as grafting new blood vessels onto the coronary arteries, repairing or replacing heart valves, or correcting congenital defects. 5. **Weaning from Bypass:** Once the repair is complete, the heart is restarted, and the patient is gradually weaned off the heart-lung machine. 6. **Closure:** The sternum is rejoined with wires, and the chest incision is closed with sutures or staples. Drains may be inserted to remove fluid.
Benefits
The benefits of cardiac surgery treatment are profound, offering a new lease on life for many patients:<ul><li><strong>Significant Symptom Relief:</strong> Alleviates chest pain (angina), shortness of breath, and fatigue, allowing for a more active lifestyle.</li><li><strong>Improved Heart Function:</strong> Restores normal blood flow, repairs damaged valves, or corrects structural defects, enhancing the heart's pumping efficiency.</li><li><strong>Increased Longevity:</strong> Reduces the risk of heart attacks, strokes, and heart failure, potentially extending life expectancy.</li><li><strong>Enhanced Quality of Life:</strong> Enables patients to return to their daily activities, hobbies, and enjoy a better overall well-being.</li><li><strong>Prevention of Future Complications:</strong> Addresses underlying issues that could lead to more severe health problems if left untreated.</li></ul>
Recovery Information
Cardiac surgery recovery time varies depending on the specific procedure, patient's overall health, and adherence to post-operative instructions. Typically, hospital stay ranges from 5 to 10 days, followed by several weeks or months of home recovery. Key aspects include:<ul><li><strong>Initial Hospital Recovery:</strong> Patients spend a day or two in the ICU, then transition to a regular ward. Early mobilization is encouraged.</li><li><strong>Home Recovery:</strong> Gradual increase in activity, avoiding heavy lifting, and managing pain. Incision care is crucial to prevent infection.</li><li><strong>Cardiac Rehabilitation:</strong> A structured program involving supervised exercise, nutrition counseling, and psychological support is often recommended to strengthen the heart and aid full recovery.</li><li><strong>Lifestyle Modifications:</strong> Adopting a heart-healthy diet, regular exercise, smoking cessation, and stress management are vital for long-term health.</li></ul>DivinHeal provides comprehensive guidance on cardiac surgery recovery and tips for optimal outcomes.

heart treatment
Treatment Price
$6000.00 USDHeart treatment aims to restore cardiac function, alleviate symptoms, improve quality of life, and extend longevity for individuals suffering from heart conditions. Techniques range from advanced medication regimens and minimally invasive procedures like angioplasty and stenting, to complex open-heart surgeries such as Coronary Artery Bypass Grafting (CABG) and valve replacement. DivinHeal ensures access to cutting-edge diagnostics and therapies, guided by experienced cardiologists and cardiac surgeons.
Heart treatment aims to restore cardiac function, alleviate symptoms, improve quality of life, and extend longevity for individuals suffering from heart conditions. Techniques range from advanced medication regimens and minimally invasive procedures like angioplasty and stenting, to complex open-heart surgeries such as Coronary Artery Bypass Grafting (CABG) and valve replacement. DivinHeal ensures access to cutting-edge diagnostics and therapies, guided by experienced cardiologists and cardiac surgeons.
Treatment Overview
Heart treatment aims to restore cardiac function, alleviate symptoms, improve quality of life, and extend longevity for individuals suffering from heart conditions. Techniques range from advanced medication regimens and minimally invasive procedures like angioplasty and stenting, to complex open-heart surgeries such as Coronary Artery Bypass Grafting (CABG) and valve replacement. DivinHeal ensures access to cutting-edge diagnostics and therapies, guided by experienced cardiologists and cardiac surgeons.
Procedures
Heart treatment procedures vary widely. For instance, an angioplasty involves inserting a catheter into a blood vessel, guiding it to the narrowed coronary artery, inflating a balloon to open the blockage, and often placing a stent to keep the artery open. A Coronary Artery Bypass Graft (CABG) surgery involves taking healthy blood vessels (grafts) from other parts of the body and attaching them to the coronary arteries, bypassing the blocked sections and restoring blood flow to the heart muscle. Valve replacement surgery entails replacing a diseased heart valve with a mechanical or biological valve. All procedures are performed under strict sterile conditions by highly skilled cardiac teams.
Benefits
<h2>Benefits of Modern Heart Treatment</h2><ul><li><strong>Improved Quality of Life:</strong> Alleviates symptoms like chest pain, shortness of breath, and fatigue, enabling a more active and fulfilling life.</li><li><strong>Extended Lifespan:</strong> Effective treatment of conditions like CAD, heart failure, and arrhythmias significantly reduces the risk of serious cardiac events and mortality.</li><li><strong>Reduced Risk of Future Complications:</strong> Procedures like angioplasty and bypass surgery restore blood flow, preventing further heart damage.</li><li><strong>Enhanced Physical Capacity:</strong> Patients often regain stamina and strength, allowing them to engage in daily activities and exercise more comfortably.</li><li><strong>Peace of Mind:</strong> Knowing you've received the best possible care for your heart provides immense reassurance for you and your family.</li><li><strong>Access to Advanced Technology:</strong> Benefiting from state-of-the-art diagnostic tools and minimally invasive surgical techniques available in top Indian hospitals.</li></ul>
Recovery Information
<h2>Heart Treatment Recovery Time and Tips</h2><p>Recovery time for heart treatment varies significantly depending on the specific procedure. For minimally invasive procedures like angioplasty, recovery is relatively quick, often allowing discharge within 1-2 days and return to normal activities within a week. For major open-heart surgeries like CABG or valve replacement, hospital stay is typically 5-7 days, with a full recovery taking anywhere from 6 to 12 weeks.</p><h3>Key Recovery Tips:</h3><ul><li><strong>Cardiac Rehabilitation:</strong> Essential for regaining strength, improving heart function, and adopting heart-healthy lifestyle habits. DivinHeal can guide you to appropriate rehab programs.</li><li><strong>Medication Adherence:</strong> Strictly follow your doctor's prescriptions for optimal healing and to prevent complications.</li><li><strong>Gradual Activity Increase:</strong> Avoid strenuous activities initially and gradually increase your physical activity as advised by your medical team.</li><li><strong>Wound Care:</strong> Keep surgical incisions clean and dry to prevent infection.</li><li><strong>Healthy Lifestyle:</strong> Adopt a balanced diet, quit smoking, limit alcohol, and manage stress.</li><li><strong>Emotional Support:</strong> Seek support from family, friends, or support groups, as emotional well-being is crucial during recovery.</li><li><strong>Regular Follow-ups:</strong> Adhere to all scheduled follow-up appointments with your cardiologist.</li></ul>

Cardiac Ablation for Arrhythmias
Treatment Price
$8500.00 USDOverview of Cardiac Ablation for Arrhythmias Treatment
The primary goal of Cardiac Ablation for Arrhythmias treatment is to eliminate or reduce the frequency of abnormal heartbeats, which can cause symptoms like palpitations, dizziness, fatigue, and shortness of breath. Utilizing advanced mapping technology, electrophysiologists identify the precise origin of the arrhythmia. Then, using catheters inserted through blood vessels, energy (radiofrequency heat or cryoablation cold) is delivered to create tiny scars, blocking the faulty electrical signals. DivinHeal connects patients with top-tier hospitals offering state-of-the-art facilities and experienced electrophysiology teams for this life-changing procedure.
Overview of Cardiac Ablation for Arrhythmias Treatment
The primary goal of Cardiac Ablation for Arrhythmias treatment is to eliminate or reduce the frequency of abnormal heartbeats, which can cause symptoms like palpitations, dizziness, fatigue, and shortness of breath. Utilizing advanced mapping technology, electrophysiologists identify the precise origin of the arrhythmia. Then, using catheters inserted through blood vessels, energy (radiofrequency heat or cryoablation cold) is delivered to create tiny scars, blocking the faulty electrical signals. DivinHeal connects patients with top-tier hospitals offering state-of-the-art facilities and experienced electrophysiology teams for this life-changing procedure.
Treatment Overview
<h2>Overview of Cardiac Ablation for Arrhythmias Treatment</h2><p>The primary goal of Cardiac Ablation for Arrhythmias treatment is to eliminate or reduce the frequency of abnormal heartbeats, which can cause symptoms like palpitations, dizziness, fatigue, and shortness of breath. Utilizing advanced mapping technology, electrophysiologists identify the precise origin of the arrhythmia. Then, using catheters inserted through blood vessels, energy (radiofrequency heat or cryoablation cold) is delivered to create tiny scars, blocking the faulty electrical signals. DivinHeal connects patients with top-tier hospitals offering state-of-the-art facilities and experienced electrophysiology teams for this life-changing procedure.</p>
Procedures
Cardiac Ablation for Arrhythmias typically begins with local anesthesia and sedation. Catheters are inserted into a vein, usually in the groin, and guided to the heart using X-ray imaging and 3D mapping systems. An electrophysiology study is performed to map the heart's electrical signals and pinpoint the precise source of the arrhythmia. Once identified, the ablation catheter delivers radiofrequency energy (heat) or cryoablation (cold) to create small scars in the problematic tissue, blocking the abnormal electrical pathways. The procedure duration varies but can take several hours. After confirming the elimination of the arrhythmia, the catheters are removed, and pressure is applied to the insertion site.
Benefits
<h2>Benefits of Cardiac Ablation for Arrhythmias</h2><p>Opting for Cardiac Ablation for Arrhythmias treatment offers numerous significant advantages, leading to a profound improvement in patients' lives. These include:</p><ul><li><h3>Restoration of Normal Heart Rhythm</h3><p>The primary benefit is the elimination or significant reduction of arrhythmias, restoring a stable and healthy heart rhythm.</p></li><li><h3>Improved Quality of Life</h3><p>Patients often experience relief from debilitating symptoms like palpitations, dizziness, fatigue, and shortness of breath, allowing them to resume normal activities.</p></li><li><h3>Reduced Reliance on Medications</h3><p>Many patients can reduce or discontinue long-term antiarrhythmic medications, avoiding their potential side effects.</p></li><li><h3>Lowered Risk of Stroke</h3><p>For conditions like Atrial Fibrillation, successful ablation significantly reduces the risk of stroke associated with blood clot formation in the heart.</p></li><li><h3>Minimally Invasive Procedure</h3><p>Cardiac Ablation is performed via catheters, avoiding open-heart surgery and resulting in faster recovery times and less discomfort.</p></li><li><h3>High Success Rate</h3><p>Modern Cardiac Ablation for Arrhythmias boasts impressive success rates, especially for specific types of arrhythmias, offering a long-term or permanent solution.</p></li></ul>
Recovery Information
<h2>Cardiac Ablation for Arrhythmias Recovery Time and Tips</h2><p>Recovery after Cardiac Ablation for Arrhythmias treatment is generally swift, given its minimally invasive nature. Most patients stay in the hospital for 1-2 days following the procedure. During this time, the medical team monitors your heart rhythm and ensures there are no immediate complications.</p><ul><li><h3>Immediate Post-Procedure (1-3 days)</h3><p>You may experience mild chest discomfort or soreness at the catheter insertion site. Rest is crucial, and heavy lifting or strenuous activity should be avoided. Your doctor will provide specific instructions regarding medication and activity levels.</p></li><li><h3>Short-Term Recovery (1-2 weeks)</h3><p>Most patients can return to light activities and work within a week. Avoid intense exercise and activities that put pressure on the groin area. It's normal to experience occasional palpitations or skipped beats during this period as the heart heals and remodels. This is part of the Cardiac Ablation for Arrhythmias recovery process.</p></li><li><h3>Long-Term Recovery & Follow-up (1-3 months)</h3><p>Full healing of the ablation sites can take several weeks to months. Regular follow-up appointments with your electrophysiologist are essential to monitor your heart rhythm and assess the procedure's success. Lifestyle modifications, such as managing stress, maintaining a healthy diet, and regular light exercise, are vital for a successful Cardiac Ablation for Arrhythmias long-term outlook.</p></li></ul>

atrial fibrillation ablation
Treatment Price
$7500.00 USDAtrial Fibrillation (AFib) ablation is a targeted interventional procedure designed to restore a normal heart rhythm (sinus rhythm) in patients suffering from AFib, a common type of arrhythmia. By strategically ablating (scarring) specific areas within the heart that generate or transmit abnormal electrical impulses, electrophysiologists can disrupt the faulty pathways responsible for AFib. This procedure is a cornerstone in managing AFib, especially when medications are ineffective or poorly tolerated, aiming to reduce symptoms, prevent AFib recurrence, and mitigate risks like stroke and heart failure. DivinHeal connects you to world-class cardiologists and state-of-the-art facilities for this life-changing treatment, focusing on your hope for a healthier future, safety, and access to quality, affordable care.
Atrial Fibrillation (AFib) ablation is a targeted interventional procedure designed to restore a normal heart rhythm (sinus rhythm) in patients suffering from AFib, a common type of arrhythmia. By strategically ablating (scarring) specific areas within the heart that generate or transmit abnormal electrical impulses, electrophysiologists can disrupt the faulty pathways responsible for AFib. This procedure is a cornerstone in managing AFib, especially when medications are ineffective or poorly tolerated, aiming to reduce symptoms, prevent AFib recurrence, and mitigate risks like stroke and heart failure. DivinHeal connects you to world-class cardiologists and state-of-the-art facilities for this life-changing treatment, focusing on your hope for a healthier future, safety, and access to quality, affordable care.
Treatment Overview
Atrial Fibrillation (AFib) ablation is a targeted interventional procedure designed to restore a normal heart rhythm (sinus rhythm) in patients suffering from AFib, a common type of arrhythmia. By strategically ablating (scarring) specific areas within the heart that generate or transmit abnormal electrical impulses, electrophysiologists can disrupt the faulty pathways responsible for AFib. This procedure is a cornerstone in managing AFib, especially when medications are ineffective or poorly tolerated, aiming to reduce symptoms, prevent AFib recurrence, and mitigate risks like stroke and heart failure. DivinHeal connects you to world-class cardiologists and state-of-the-art facilities for this life-changing treatment, focusing on your hope for a healthier future, safety, and access to quality, affordable care.
Procedures
Atrial fibrillation ablation is performed in a specialized electrophysiology (EP) lab. After administering local anesthesia and light sedation, thin, flexible catheters are inserted into blood vessels, typically in the groin, and meticulously guided to the heart using advanced imaging techniques such as fluoroscopy and 3D electro-anatomical mapping systems. The electrophysiologist identifies the specific areas within the atria responsible for generating or propagating the irregular electrical signals that cause AFib. Energy (either radiofrequency heat or cryoablation cold) is then precisely delivered through the catheter tip to create small, controlled scars. These scars effectively block these abnormal electrical pathways, electrically isolating the problematic areas, most commonly around the pulmonary veins. The entire procedure usually lasts 2-4 hours, with continuous monitoring of the patient's heart rhythm and vital signs for utmost safety.
Benefits
<h3>Key Benefits of Atrial Fibrillation Ablation Treatment</h3><ul><li><strong>Restoration of Normal Heart Rhythm:</strong> Significantly increases the chance of maintaining a normal sinus rhythm, improving overall heart function and stability.</li><li><strong>Symptom Relief:</strong> Effectively reduces or eliminates debilitating AFib symptoms such as palpitations, fatigue, shortness of breath, and dizziness, enhancing daily comfort.</li><li><strong>Reduced Medication Dependency:</strong> Many patients can reduce or discontinue antiarrhythmic medications post-ablation, minimizing side effects and long-term drug costs.</li><li><strong>Lowered Stroke Risk:</strong> While anticoagulation often remains necessary, successful ablation can contribute to a reduced overall risk of AFib-related stroke.</li><li><strong>Improved Quality of Life:</strong> Patients often report enhanced energy levels, exercise tolerance, and a better overall quality of life, allowing them to resume activities they love.</li><li><strong>Prevention of AFib Progression:</strong> Can prevent the progression of paroxysmal AFib to more persistent forms, preserving heart health over time.</li><li><strong>Minimized Risk of Heart Failure:</strong> By restoring normal rhythm, ablation can help prevent AFib-induced heart weakening (tachycardia-induced cardiomyopathy), safeguarding long-term cardiac function.</li></ul><p>Choosing atrial fibrillation ablation offers a hopeful pathway to a healthier, more active life with greater cardiac stability.</p>
Recovery Information
<h3>Atrial Fibrillation Ablation Recovery Time and Tips</h3><p>The immediate recovery after atrial fibrillation ablation typically involves a 1-3 day hospital stay for monitoring and initial healing. Patients are usually advised to limit strenuous activities for the first week. Full recovery and return to normal activities generally take about 4-6 weeks. It's common to experience some chest discomfort, occasional palpitations, or fatigue during this period as the heart heals and adapts to its new rhythm. Medications, especially antiarrhythmics and anticoagulants, will likely continue for several weeks or months post-procedure, guided by your cardiologist.</p><h3>Essential Atrial Fibrillation Ablation Recovery Tips:</h3><ul><li><strong>Follow Medication Schedule:</strong> Adhere strictly to your cardiologist's prescribed medications, especially blood thinners, to prevent complications like blood clots.</li><li><strong>Avoid Strenuous Activity:</strong> Refrain from heavy lifting, intense exercise, and prolonged standing for 4-6 weeks to allow the groin puncture site to heal and minimize bleeding risk.</li><li><strong>Monitor Symptoms:</strong> Report any new or worsening symptoms (e.g., severe chest pain, prolonged bleeding, fever, signs of infection) to your doctor immediately.</li><li><strong>Stay Hydrated:</strong> Drink plenty of fluids as recommended to aid recovery.</li><li><strong>Adopt a Heart-Healthy Lifestyle:</strong> Embrace a balanced diet, manage stress, maintain a healthy weight, and avoid excessive caffeine and alcohol as advised to support long-term heart health.</li><li><strong>Attend Follow-up Appointments:</strong> Regular check-ups with your electrophysiologist are crucial to monitor your heart rhythm, assess healing, and adjust medications as needed.</li><li><strong>Seek Emotional Support:</strong> It's normal to experience anxiety or fluctuations in mood; seeking support from family, friends, or a counselor can be beneficial during recovery.</li></ul><p>DivinHeal's dedicated care team provides detailed recovery guidelines and is available to assist with any post-procedure concerns, ensuring a smooth and safe healing process, empowering you with quality care and reassurance.</p>

electrophysiology cardiology
Treatment Price
$6000.00 USDCardiac electrophysiology aims to correct irregular heartbeats, improve quality of life, and prevent serious complications like stroke or sudden cardiac arrest. Techniques range from minimally invasive catheter ablations to device implantations like pacemakers and ICDs, tailored to each patient's specific arrhythmia.
Cardiac electrophysiology aims to correct irregular heartbeats, improve quality of life, and prevent serious complications like stroke or sudden cardiac arrest. Techniques range from minimally invasive catheter ablations to device implantations like pacemakers and ICDs, tailored to each patient's specific arrhythmia.
Treatment Overview
Cardiac electrophysiology aims to correct irregular heartbeats, improve quality of life, and prevent serious complications like stroke or sudden cardiac arrest. Techniques range from minimally invasive catheter ablations to device implantations like pacemakers and ICDs, tailored to each patient's specific arrhythmia.
Procedures
Electrophysiology cardiology procedures often begin with an Electrophysiology Study (EPS) to precisely map the heart's electrical pathways and identify the source of arrhythmias. For catheter ablation, thin, flexible catheters are guided through blood vessels to the heart. Radiofrequency (heat) or cryoenergy (cold) is then applied to ablate (destroy) the small areas of heart tissue responsible for the irregular beats. For pacemaker/ICD implantation, a small incision is made, typically beneath the collarbone, and the device is placed under the skin. Leads are then threaded through veins into the heart chambers, connecting to the device to monitor and regulate heart rhythm.
Benefits
The benefits of successful electrophysiology cardiology treatment include improved heart rhythm, significant relief from debilitating symptoms like palpitations, dizziness, and fatigue, a reduced risk of serious complications such as stroke and sudden cardiac arrest, and a dramatically enhanced quality of life. For many, these advanced procedures offer a lasting solution, restoring normal heart function and enabling a return to active lifestyles.
Recovery Information
Electrophysiology cardiology recovery time and tips vary based on the specific procedure. For catheter ablation, patients typically return to light activities within a week and full activity within 2-4 weeks. Pacemaker or ICD implantation recovery is similar, with specific care instructions for arm movement (e.g., avoiding lifting the arm above the shoulder for 4-6 weeks) to allow the device leads to secure properly. Comprehensive post-procedure guidance and follow-up are crucial for optimal electrophysiology cardiology recovery.

icd device
Treatment Price
$8500.00 USDICD device treatment involves surgically implanting an advanced electronic device that continuously monitors the heart's electrical activity. Its primary goal is to detect and correct dangerously fast heart rhythms (ventricular tachycardia or ventricular fibrillation) by delivering a controlled electrical impulse or shock, thereby restoring a normal heart rhythm and safeguarding against sudden cardiac death.
ICD device treatment involves surgically implanting an advanced electronic device that continuously monitors the heart's electrical activity. Its primary goal is to detect and correct dangerously fast heart rhythms (ventricular tachycardia or ventricular fibrillation) by delivering a controlled electrical impulse or shock, thereby restoring a normal heart rhythm and safeguarding against sudden cardiac death.
Treatment Overview
ICD device treatment involves surgically implanting an advanced electronic device that continuously monitors the heart's electrical activity. Its primary goal is to detect and correct dangerously fast heart rhythms (ventricular tachycardia or ventricular fibrillation) by delivering a controlled electrical impulse or shock, thereby restoring a normal heart rhythm and safeguarding against sudden cardiac death.
Procedures
1. **Preparation:** The patient is positioned on the operating table, and local anesthesia is administered to numb the incision area, often combined with light sedation or general anesthesia.2. **Incision:** A small incision (typically 2-4 inches) is made in the upper chest, usually below the collarbone.3. **Lead Implantation:** Thin, insulated wires (leads) are guided through a vein into the heart chambers (right atrium and/or right ventricle) using fluoroscopy (X-ray imaging). The tips of the leads are anchored to the heart wall. For S-ICD, leads are placed under the skin, outside the heart.4. **Device Connection:** The other ends of the leads are connected to the ICD pulse generator.5. **Pocket Creation:** A small pocket is created under the skin or muscle in the chest to house the ICD device.6. **Device Implantation:** The ICD pulse generator is placed into the prepared pocket.7. **Testing:** The device is tested to ensure it can accurately sense heart rhythms and deliver appropriate therapy. This may involve inducing a brief, controlled arrhythmia to verify the ICD's response.8. **Closure:** Once optimal function is confirmed, the incision is closed with sutures and covered with a sterile dressing.
Benefits
<h2>Key Benefits of ICD Device Implantation</h2><ul><li><strong>Prevention of Sudden Cardiac Death:</strong> The primary benefit is the life-saving ability to detect and terminate life-threatening ventricular arrhythmias, significantly reducing the risk of sudden cardiac arrest.</li><li><strong>Improved Quality of Life:</strong> For patients living with the fear of a cardiac event, an ICD provides peace of mind, allowing them to lead more active and fulfilling lives.</li><li><strong>Continuous Monitoring:</strong> ICDs offer constant, 24/7 monitoring of heart rhythm, providing immediate intervention when needed.</li><li><strong>Personalized Therapy:</strong> Modern ICDs can be programmed to deliver specific therapies (pacing or shock) tailored to the individual's condition.</li><li><strong>Diagnostic Data:</strong> The device records heart rhythm events, providing valuable data for cardiologists to optimize treatment plans.</li><li><strong>Enhanced Safety:</strong> For those with conditions predisposing them to dangerous arrhythmias, an ICD acts as a crucial safety net.</li></ul>
Recovery Information
<h2>ICD Device Recovery Time and Tips</h2><h3>Immediate Post-Procedure Recovery (Hospital Stay)</h3><p>After ICD implantation, patients typically stay in the hospital for 1-3 days for monitoring. You may experience some pain, bruising, or swelling at the incision site, which can be managed with medication. Your doctor will provide instructions on arm movement restrictions to allow the leads to settle in the heart.</p><h3>Home Recovery (First 4-6 Weeks)</h3><ul><li><strong>Activity Restrictions:</strong> Avoid lifting the arm on the side of the implant above shoulder height, heavy lifting, or strenuous activities for 4-6 weeks.</li><li><strong>Wound Care:</strong> Keep the incision site clean and dry. Watch for signs of infection (redness, pus, fever).</li><li><strong>Driving:</strong> You may have temporary driving restrictions, especially if you have recently experienced an arrhythmia that required a shock.</li><li><strong>Work:</strong> Most individuals can return to light work within a week or two, depending on their occupation.</li></ul><h3>Long-Term Recovery and Living with an ICD</h3><ul><li><strong>Follow-Up Appointments:</strong> Regular follow-up appointments are essential to check device function and battery life.</li><li><strong>Lifestyle Adjustments:</strong> While most daily activities can resume, discuss any concerns about sports, travel, or magnetic fields with your doctor.</li><li><strong>Emotional Support:</strong> Some patients may experience anxiety or depression related to living with an ICD. Counseling or support groups can be beneficial.</li><li><strong>Medicines:</strong> Continue all prescribed medications as directed by your cardiologist.</li><li><strong>Emergency Information:</strong> Carry your ICD identification card and inform healthcare providers about your device.</li></ul>

pacemaker
Treatment Price
$3000.00 USDPacemaker treatment aims to restore a normal heart rate and rhythm, alleviating symptoms caused by electrical conduction disorders of the heart. The procedure involves surgically implanting a pulse generator and leads into the heart, ensuring consistent and effective heart function. DivinHeal connects patients with leading cardiac centers and top cardiologists globally, emphasizing precise diagnosis and personalized therapy options for pacemaker implantation and follow-up care.
Pacemaker treatment aims to restore a normal heart rate and rhythm, alleviating symptoms caused by electrical conduction disorders of the heart. The procedure involves surgically implanting a pulse generator and leads into the heart, ensuring consistent and effective heart function. DivinHeal connects patients with leading cardiac centers and top cardiologists globally, emphasizing precise diagnosis and personalized therapy options for pacemaker implantation and follow-up care.
Treatment Overview
<p>Pacemaker treatment aims to restore a normal heart rate and rhythm, alleviating symptoms caused by electrical conduction disorders of the heart. The procedure involves surgically implanting a pulse generator and leads into the heart, ensuring consistent and effective heart function. DivinHeal connects patients with leading cardiac centers and top cardiologists globally, emphasizing precise diagnosis and personalized therapy options for pacemaker implantation and follow-up care.</p>
Procedures
Pacemaker implantation is typically performed under local anesthesia with sedation. An incision, usually 2-3 inches long, is made in the skin near the shoulder or collarbone. The cardiologist then identifies a major vein, often the subclavian vein, through which one or more insulated leads are guided using fluoroscopy (X-ray imaging) into the appropriate chambers of the heart. The tips of the leads are anchored to the heart muscle. Once the leads are in place and tested to ensure proper signal transmission, they are connected to the pulse generator. The pulse generator is then placed in a small pocket created under the skin, usually below the collarbone. Finally, the incision is closed with sutures.
Benefits
<h2>Benefits of Pacemaker Implantation</h2><ul><li><h3>Restored Normal Heart Rate</h3><p>The primary benefit is regulating a slow or irregular heart rate, ensuring consistent blood flow throughout the body.</p></li><li><h3>Alleviation of Symptoms</h3><p>Patients typically experience a significant reduction or complete elimination of symptoms such as dizziness, fatigue, shortness of breath, and fainting spells.</p></li><li><h3>Improved Quality of Life</h3><p>With symptoms relieved, patients can resume normal activities, regain energy, and enjoy a much-improved quality of life.</p></li><li><h3>Prevention of Complications</h3><p>A pacemaker can prevent serious complications associated with persistent bradycardia, including falls, injury, and more severe cardiac events.</p></li><li><h3>Enhanced Longevity</h3><p>For many, a pacemaker is a life-saving device that significantly extends lifespan by maintaining vital heart function.</p></li><li><h3>High Success Rate</h3><p>Modern pacemaker implantation boasts a very high pacemaker success rate, with immediate and lasting positive outcomes for most patients.</p></li></ul>
Recovery Information
<h2>Pacemaker Recovery Time and Tips</h2><ul><li><h3>Immediate Post-Procedure Care</h3><p>After your pacemaker surgery, you'll be monitored in the hospital for 1-3 days. You may experience some soreness, bruising, or swelling at the incision site, which is normal. Pain medication will be provided as needed.</p></li><li><h3>First Few Weeks (3-6 Weeks)</h3><p>During the initial pacemaker recovery time, it's crucial to avoid strenuous activities and heavy lifting (typically over 5-10 pounds) with the arm on the side of the implant. Keep the incision site clean and dry. You'll have follow-up appointments to check the incision and ensure the device is functioning correctly.</p></li><li><h3>Long-Term Recovery & Lifestyle</h3><p>Most patients fully recover and return to their normal routines within a few weeks. However, it's important to be aware of electromagnetic interference (EMI) sources and follow your doctor's guidelines regarding cell phone use, certain electrical devices, and medical imaging (like MRIs, unless your pacemaker is MRI-safe). Regular follow-up appointments (often annually) with your cardiologist are essential to monitor your pacemaker's function and battery life (which typically lasts 5-15 years).</p></li><li><h3>Emotional and Psychological Support</h3><p>Adjusting to a pacemaker can sometimes involve emotional challenges. DivinHeal provides resources and support to help patients adapt, focusing on mental well-being as much as physical recovery.</p></li></ul>

ventricular assist device
Treatment Price
$35000.00 USDVentricular Assist Device Treatment Overview
Ventricular Assist Device (VAD) treatment is a life-saving intervention designed to improve the quality of life and extend survival for patients suffering from severe, end-stage heart failure. This advanced cardiac procedure involves surgically implanting a sophisticated mechanical pump that helps the heart circulate blood throughout the body. By reducing the workload on a failing heart, VADs alleviate debilitating symptoms like extreme fatigue and shortness of breath, enhancing organ function and restoring a semblance of normal activity. DivinHeal connects you with world-class cardiac surgeons and facilities, ensuring optimal outcomes with compassionate care.
Ventricular Assist Device Treatment Overview
Ventricular Assist Device (VAD) treatment is a life-saving intervention designed to improve the quality of life and extend survival for patients suffering from severe, end-stage heart failure. This advanced cardiac procedure involves surgically implanting a sophisticated mechanical pump that helps the heart circulate blood throughout the body. By reducing the workload on a failing heart, VADs alleviate debilitating symptoms like extreme fatigue and shortness of breath, enhancing organ function and restoring a semblance of normal activity. DivinHeal connects you with world-class cardiac surgeons and facilities, ensuring optimal outcomes with compassionate care.
Treatment Overview
<h2>Ventricular Assist Device Treatment Overview</h2><p>Ventricular Assist Device (VAD) treatment is a life-saving intervention designed to improve the quality of life and extend survival for patients suffering from severe, end-stage heart failure. This advanced cardiac procedure involves surgically implanting a sophisticated mechanical pump that helps the heart circulate blood throughout the body. By reducing the workload on a failing heart, VADs alleviate debilitating symptoms like extreme fatigue and shortness of breath, enhancing organ function and restoring a semblance of normal activity. DivinHeal connects you with world-class cardiac surgeons and facilities, ensuring optimal outcomes with compassionate care.</p>
Procedures
The Ventricular Assist Device (VAD) implantation is a complex open-heart surgery. After general anesthesia, an incision is made in the chest to access the heart. The VAD is typically implanted below the heart, with inflow cannulas connected to the left (or right) ventricle and outflow cannulas connected to the aorta (or pulmonary artery). The device's pump then takes over the function of the failing ventricle, circulating blood. A driveline exits the skin, connecting the internal pump to an external controller and battery pack. The chest is then closed.
Benefits
<h2>Benefits of Ventricular Assist Device Treatment</h2><ul><li><h3>Improved Heart Function</h3><p>VADs directly assist the heart in pumping blood, leading to better circulation and reduced strain on the failing heart.</p></li><li><h3>Reduced Symptoms</h3><p>Patients experience significant relief from debilitating symptoms of heart failure, such as shortness of breath, fatigue, and swelling.</p></li><li><h3>Enhanced Quality of Life</h3><p>With improved energy levels and reduced symptoms, patients can often return to many daily activities, improving their overall well-being.</p></li><li><h3>Extended Survival</h3><p>For patients with advanced heart failure, VADs can significantly prolong life, often for many years.</p></li><li><h3>Bridge to Transplant</h3><p>For eligible patients, VADs can sustain them until a suitable heart donor becomes available.</p></li><li><h3>Destination Therapy</h3><p>For patients not eligible for transplant, VADs offer a long-term solution to manage heart failure and improve prognosis.</p></li></ul>
Recovery Information
<h2>Ventricular Assist Device Recovery Time and Tips</h2><p>Recovery from Ventricular Assist Device (VAD) implantation is a gradual process requiring dedication and comprehensive support. The initial hospital stay typically ranges from 2 to 4 weeks, during which patients receive intensive care and begin rehabilitation.</p><h3>Key Aspects of VAD Recovery:</h3><ul><li><h3>Hospital Stay</h3><p>Post-surgery, patients spend time in the ICU for close monitoring before moving to a cardiac ward. During this period, wound care, pain management, and early mobilization are critical.</p></li><li><h3>Device Management Training</h3><p>Patients and their caregivers receive extensive training on how to manage the VAD, including battery changes, alarm recognition, and proper care of the driveline exit site to prevent infection.</p></li><li><h3>Physical Rehabilitation</h3><p>A tailored physical therapy program is vital for regaining strength, endurance, and mobility. This often begins in the hospital and continues with outpatient cardiac rehabilitation.</p></li><li><h3>Medication Adherence</h3><p>Strict adherence to prescribed medications, including anticoagulants to prevent blood clots, is crucial for long-term success and to prevent complications.</p></li><li><h3>Nutritional Guidance</h3><p>A healthy diet supports healing and overall well-being. Nutritionists provide personalized plans to meet specific dietary needs.</p></li><li><h3>Psychological Support</h3><p>Adjusting to life with a VAD can be challenging. Emotional counseling and support groups are often recommended to help patients and families cope with the changes.</p></li><li><h3>Long-Term Follow-up</h3><p>Regular follow-up appointments with the VAD team are essential to monitor device function, assess heart health, and manage any potential complications. DivinHeal facilitates seamless communication with your care team for your ventricular assist device long-term management.</p></li></ul>

mitral valve surgery
Treatment Price
$8000.00 USDOverview of Mitral Valve Surgery Treatment
Mitral valve surgery aims to correct issues with the heart's mitral valve, which controls blood flow between the left atrium and left ventricle. Whether through repair (valvuloplasty) or replacement (using mechanical or biological valves), the goal is to improve the heart's pumping efficiency, relieve symptoms, and significantly enhance a patient's quality of life and longevity. DivinHeal connects you with top cardiovascular surgeons and state-of-the-art facilities for optimal outcomes in mitral valve surgery treatment.
Overview of Mitral Valve Surgery Treatment
Mitral valve surgery aims to correct issues with the heart's mitral valve, which controls blood flow between the left atrium and left ventricle. Whether through repair (valvuloplasty) or replacement (using mechanical or biological valves), the goal is to improve the heart's pumping efficiency, relieve symptoms, and significantly enhance a patient's quality of life and longevity. DivinHeal connects you with top cardiovascular surgeons and state-of-the-art facilities for optimal outcomes in mitral valve surgery treatment.
Treatment Overview
<h2>Overview of Mitral Valve Surgery Treatment</h2><p>Mitral valve surgery aims to correct issues with the heart's mitral valve, which controls blood flow between the left atrium and left ventricle. Whether through repair (valvuloplasty) or replacement (using mechanical or biological valves), the goal is to improve the heart's pumping efficiency, relieve symptoms, and significantly enhance a patient's quality of life and longevity. DivinHeal connects you with top cardiovascular surgeons and state-of-the-art facilities for optimal outcomes in mitral valve surgery treatment.</p>
Procedures
Mitral valve surgery involves several key steps. For traditional open-heart surgery, a median sternotomy (an incision through the breastbone) is performed. The patient is then connected to a heart-lung machine, which takes over the functions of the heart and lungs, allowing the surgeon to work on a still heart. If repair is possible, the surgeon will use techniques such as annuloplasty (implanting a ring to reshape the valve opening), leaflet repair (removing or reshaping valve tissue), or chordal repair (repairing or replacing the "heart strings"). If the valve is too damaged, it is carefully excised, and a prosthetic valve (mechanical or biological) is sewn into place. Once the repair or replacement is complete, the heart is restarted, and the patient is weaned off the heart-lung machine. The sternum is then closed with wires, and the incision is sutured. Minimally invasive approaches use smaller incisions, often between the ribs, with specialized instruments and sometimes robotic assistance, avoiding the sternotomy.
Benefits
<h2>Benefits of Mitral Valve Surgery Treatment</h2><ul><li><h3>Improved Heart Function</h3><p>Successfully treated mitral valve ensures efficient blood flow, reducing strain on the heart and improving its overall pumping capability.</p></li><li><h3>Relief from Symptoms</h3><p>Patients typically experience significant reduction or elimination of symptoms like shortness of breath, fatigue, chest pain, and palpitations, leading to a greatly improved quality of life.</p></li><li><h3>Prevention of Heart Failure</h3><p>By correcting the valve dysfunction, the surgery helps prevent the progression of heart disease to severe conditions like congestive heart failure.</p></li><li><h3>Increased Longevity</h3><p>For patients with severe mitral valve disease, surgery can significantly extend lifespan and reduce the risk of sudden cardiac events.</p></li><li><h3>Enhanced Quality of Life</h3><p>Many patients report increased energy levels, improved exercise tolerance, and the ability to return to normal daily activities and hobbies.</p></li><li><h3>Minimally Invasive Options</h3><p>For eligible candidates, minimally invasive techniques offer benefits such as smaller incisions, less pain, reduced blood loss, and faster recovery times for mitral valve surgery.</p></li></ul>
Recovery Information
<h2>Recovery and Life After Mitral Valve Surgery</h2><p>Recovery from mitral valve surgery is a gradual process that varies for each individual, influenced by the type of surgery (open-heart vs. minimally invasive), age, and overall health. Here's what to expect regarding mitral valve surgery recovery time and tips:</p><ul><li><h3>Immediate Post-Operative Period (Hospital Stay)</h3><p>Typically 5-7 days for open-heart surgery, with the first 1-2 days in the ICU. Patients receive pain management, respiratory support, and gradual mobilization under medical supervision.</p></li><li><h3>First Few Weeks at Home (2-6 Weeks)</h3><p>Activity restrictions are crucial, especially for sternal precautions (avoiding heavy lifting, pushing, or pulling). Patients gradually increase walking and light activities. Fatigue is common, and proper wound care is essential.</p></li><li><h3>Cardiac Rehabilitation</h3><p>Many patients benefit from a structured cardiac rehab program, which includes supervised exercise, education on heart-healthy living, and emotional support. DivinHeal can guide you to appropriate rehabilitation programs.</p></li><li><h3>Full Recovery (2-3 Months to 6 Months)</h3><p>Full recovery can take 2-3 months for minimally invasive procedures and up to 6 months for open-heart surgery. Patients typically return to work and most normal activities during this period.</p></li><li><h3>Long-Term Wellness</h3><p>Adherence to medication (especially anticoagulants for mechanical valves), a heart-healthy diet, regular exercise, and avoiding smoking are crucial for long-term success. Regular follow-ups with a cardiologist are essential.</p></li><li><h3>Emotional Support</h3><p>It's normal to experience emotional fluctuations during recovery. DivinHeal offers resources for counseling and support groups to help navigate this journey.</p></li></ul>

aortic valve surgery
Treatment Price
$9000.00 USDAortic Valve Surgery: Restoring Heart Health
Aortic valve surgery aims to correct issues with the heart's aortic valve, which controls blood flow from the left ventricle to the aorta. The primary goals are to relieve symptoms, prevent further heart damage, and improve longevity.
Procedures range from traditional open-heart surgery (Aortic Valve Replacement, AVR) to less invasive options like Transcatheter Aortic Valve Implantation (TAVI/TAVR) or minimally invasive aortic valve surgery. These techniques either repair the existing valve or replace it with a prosthetic (mechanical or biological) valve, ensuring optimal cardiac function and patient safety.
Aortic Valve Surgery: Restoring Heart Health
Aortic valve surgery aims to correct issues with the heart's aortic valve, which controls blood flow from the left ventricle to the aorta. The primary goals are to relieve symptoms, prevent further heart damage, and improve longevity.
Procedures range from traditional open-heart surgery (Aortic Valve Replacement, AVR) to less invasive options like Transcatheter Aortic Valve Implantation (TAVI/TAVR) or minimally invasive aortic valve surgery. These techniques either repair the existing valve or replace it with a prosthetic (mechanical or biological) valve, ensuring optimal cardiac function and patient safety.
Treatment Overview
<h2>Aortic Valve Surgery: Restoring Heart Health</h2><p>Aortic valve surgery aims to correct issues with the heart's aortic valve, which controls blood flow from the left ventricle to the aorta. The primary goals are to relieve symptoms, prevent further heart damage, and improve longevity.</p><p>Procedures range from traditional open-heart surgery (Aortic Valve Replacement, AVR) to less invasive options like Transcatheter Aortic Valve Implantation (TAVI/TAVR) or minimally invasive aortic valve surgery. These techniques either repair the existing valve or replace it with a prosthetic (mechanical or biological) valve, ensuring optimal cardiac function and patient safety.</p>
Procedures
Aortic valve surgery involves either repairing or replacing a diseased aortic valve. 1. **Open-Heart Aortic Valve Replacement (AVR):** * **Anesthesia:** General anesthesia is administered. * **Incision:** A sternotomy (an incision down the middle of the chest, through the breastbone) is made to access the heart. * **Bypass Machine:** The heart-lung bypass machine takes over the function of the heart and lungs, allowing the surgeon to operate on a still, bloodless heart. * **Valve Removal:** The diseased aortic valve is carefully excised. * **Valve Implantation:** A new prosthetic valve (mechanical or biological) is sewn into place. * **Closure:** The heart is restarted, the patient is weaned off the bypass machine, and the incision is closed layer by layer, with the breastbone wired together. 2. **Transcatheter Aortic Valve Implantation (TAVI/TAVR):** * **Access:** Typically performed via a small incision in the groin (femoral artery), or less commonly, through a small incision in the chest (transapical, transcaval). * **Catheter Guidance:** A catheter with a collapsed replacement valve is guided through the blood vessels to the heart. * **Valve Deployment:** The new valve is precisely positioned within the diseased native aortic valve and expanded, pushing the old valve leaflets aside. * **Withdrawal:** The catheter is removed, and the access site is closed. This procedure is performed on a beating heart, often under conscious sedation or general anesthesia, without the need for a heart-lung bypass machine. 3. **Minimally Invasive Aortic Valve Surgery:** * Uses smaller incisions (mini-sternotomy or right mini-thoracotomy) compared to traditional open-heart surgery. * Still often requires a heart-lung bypass machine but can result in less pain, shorter hospital stays, and faster recovery for selected patients.
Benefits
<h2>Key Benefits of Aortic Valve Surgery</h2><ul><li><h3>Improved Cardiac Function:</h3><p>Restores efficient blood flow, reducing strain on the heart and improving its pumping ability.</p></li><li><h3>Symptom Relief:</h3><p>Alleviates debilitating symptoms such as shortness of breath, chest pain, dizziness, and fatigue.</p></li><li><h3>Increased Longevity:</h3><p>Significantly improves life expectancy for patients with severe aortic valve disease.</p></li><li><h3>Enhanced Quality of Life:</h3><p>Allows patients to resume normal activities and enjoy a more active, healthier lifestyle.</p></li><li><h3>Reduced Risk of Heart Failure:</h3><p>Prevents or slows the progression of heart failure and other serious cardiac complications.</p></li><li><h3>Access to Advanced Techniques:</h3><p>Modern approaches like TAVR offer less invasive options with faster recovery for eligible patients.</p></li></ul>
Recovery Information
<h2>Aortic Valve Surgery Recovery Time and Tips</h2><p>Recovery from aortic valve surgery varies depending on the type of procedure (open-heart vs. TAVR), individual health, and adherence to post-operative instructions.</p><ul><li><h3>Hospital Stay:</h3><p>Typically 5-7 days for open-heart surgery, with the first 1-2 days in an intensive care unit (ICU). TAVR patients may have a shorter stay, sometimes 2-3 days.</p></li><li><h3>Initial Home Recovery (First 2-4 weeks):</h3><p>Patients will experience fatigue, and some discomfort at the incision site. Activities like lifting heavy objects, driving, and strenuous exercise are restricted. Gradually increasing light activity is encouraged.</p></li><li><h3>Full Recovery (2-6 months):</h3><p>For open-heart surgery, full sternal healing can take 6-8 weeks, and complete recovery often extends to 3-6 months. TAVR recovery is generally faster, with many patients feeling significantly better within a few weeks.</p></li><li><h3>Cardiac Rehabilitation:</h3><p>A crucial part of recovery, involving supervised exercise, education on heart-healthy living, and emotional support. DivinHeal helps coordinate access to these programs.</p></li><li><h3>Medication Management:</h3><p>Adherence to prescribed medications, including anti-coagulants (for mechanical valves) and blood pressure medications, is vital.</p></li><li><h3>Lifestyle Adjustments:</h3><p>Adopting a heart-healthy diet, regular light exercise, smoking cessation, and stress management are essential for long-term success. Regular follow-up with your cardiologist is paramount.</p></li></ul>

heart valve surgery
Treatment Price
$8500.00 USDHeart valve surgery aims to correct structural issues with the heart's valves, ensuring efficient blood circulation. Techniques range from traditional open-heart surgery to minimally invasive procedures and transcatheter approaches, tailored to the patient's specific condition and overall health. DivinHeal connects you to world-class cardiac centers offering comprehensive diagnostic and therapeutic options.
Heart valve surgery aims to correct structural issues with the heart's valves, ensuring efficient blood circulation. Techniques range from traditional open-heart surgery to minimally invasive procedures and transcatheter approaches, tailored to the patient's specific condition and overall health. DivinHeal connects you to world-class cardiac centers offering comprehensive diagnostic and therapeutic options.
Treatment Overview
Heart valve surgery aims to correct structural issues with the heart's valves, ensuring efficient blood circulation. Techniques range from traditional open-heart surgery to minimally invasive procedures and transcatheter approaches, tailored to the patient's specific condition and overall health. DivinHeal connects you to world-class cardiac centers offering comprehensive diagnostic and therapeutic options.
Procedures
Heart valve surgery, whether repair or replacement, is typically performed under general anesthesia. For traditional open-heart surgery, the surgeon makes an incision in the chest and may connect the patient to a heart-lung bypass machine, which temporarily takes over the heart's function. The damaged valve is then either repaired using techniques like annuloplasty or leaflet reconstruction, or it is removed and replaced with a mechanical or bioprosthetic valve. After the procedure, the patient is weaned off the bypass machine, and the chest incision is closed. Minimally invasive approaches involve smaller incisions and specialized instruments, while transcatheter procedures (like TAVR) involve inserting a catheter through an artery, usually in the groin, to deliver and deploy a new valve without major incisions.
Benefits
<ul><li>Improved heart function and blood circulation.</li><li>Relief from symptoms like shortness of breath, fatigue, and chest pain.</li><li>Reduced risk of heart failure, stroke, and sudden cardiac death.</li><li>Enhanced quality of life and increased longevity.</li><li>Potential for a return to normal activities and improved exercise tolerance.</li><li>For valve repair, preservation of natural valve tissue and potentially avoiding lifelong anticoagulation.</li></ul>
Recovery Information
Recovery from heart valve surgery varies depending on the type of procedure (open-heart vs. minimally invasive) and individual patient factors. Generally, hospital stay ranges from 5-10 days. Full recovery can take 6-12 weeks for open-heart surgery, involving a gradual return to normal activities. Patients are encouraged to participate in cardiac rehabilitation, which includes supervised exercise, education on heart-healthy living, and emotional support. Post-operative care involves regular follow-ups, medication management, and lifestyle modifications for optimal long-term health. DivinHeal provides comprehensive guidance for your recovery journey.

valve replacement
Treatment Price
$7000.00 USDValve Replacement Treatment Overview
Restoring Heart Health Through Advanced Valve Procedures
Valve replacement treatment is a critical intervention for patients suffering from valvular heart disease, where one or more heart valves fail to open or close properly. This condition can lead to symptoms like shortness of breath, chest pain, and fatigue, significantly impacting quality of life.
DivinHeal partners with leading cardiac centers globally, offering state-of-the-art diagnostic and therapeutic options. Our approach focuses on personalized care, utilizing advanced techniques such as traditional open-heart surgery for complex cases, and minimally invasive options like Transcatheter Aortic Valve Implantation (TAVI) for those unsuitable for open surgery, ensuring optimal outcomes with reduced recovery times.
We emphasize safety, affordability, and quality, facilitating access to world-class cardiac surgeons and cutting-edge facilities, particularly in India, where exceptional care meets cost-effectiveness.
Valve Replacement Treatment Overview
Restoring Heart Health Through Advanced Valve Procedures
Valve replacement treatment is a critical intervention for patients suffering from valvular heart disease, where one or more heart valves fail to open or close properly. This condition can lead to symptoms like shortness of breath, chest pain, and fatigue, significantly impacting quality of life.
DivinHeal partners with leading cardiac centers globally, offering state-of-the-art diagnostic and therapeutic options. Our approach focuses on personalized care, utilizing advanced techniques such as traditional open-heart surgery for complex cases, and minimally invasive options like Transcatheter Aortic Valve Implantation (TAVI) for those unsuitable for open surgery, ensuring optimal outcomes with reduced recovery times.
We emphasize safety, affordability, and quality, facilitating access to world-class cardiac surgeons and cutting-edge facilities, particularly in India, where exceptional care meets cost-effectiveness.
Treatment Overview
<h2>Valve Replacement Treatment Overview</h2> <h3>Restoring Heart Health Through Advanced Valve Procedures</h3> <p>Valve replacement treatment is a critical intervention for patients suffering from valvular heart disease, where one or more heart valves fail to open or close properly. This condition can lead to symptoms like shortness of breath, chest pain, and fatigue, significantly impacting quality of life.</p> <p>DivinHeal partners with leading cardiac centers globally, offering state-of-the-art diagnostic and therapeutic options. Our approach focuses on personalized care, utilizing advanced techniques such as traditional open-heart surgery for complex cases, and minimally invasive options like Transcatheter Aortic Valve Implantation (TAVI) for those unsuitable for open surgery, ensuring optimal outcomes with reduced recovery times.</p> <p>We emphasize safety, affordability, and quality, facilitating access to world-class cardiac surgeons and cutting-edge facilities, particularly in India, where exceptional care meets cost-effectiveness.</p>
Procedures
A valve replacement procedure typically involves the following steps: 1. **Anesthesia**: The patient is given general anesthesia to ensure they are unconscious and pain-free throughout the surgery. 2. **Incision**: * **Open-Heart Surgery**: A sternotomy (an incision down the middle of the chest, splitting the breastbone) is made to access the heart. * **Minimally Invasive Surgery**: Smaller incisions are made, often through the side of the chest, or a small incision in the groin for transcatheter procedures. 3. **Cardiopulmonary Bypass**: For open-heart surgery, the heart is stopped, and the patient is connected to a heart-lung machine (cardiopulmonary bypass) which takes over the functions of the heart and lungs, circulating oxygenated blood throughout the body. (This step is often avoided or minimally used in TAVI/TMVR). 4. **Valve Removal**: The diseased or damaged heart valve is carefully removed. 5. **New Valve Implantation**: The new prosthetic valve (mechanical or biological) is meticulously sewn into place (for open/minimally invasive surgery) or deployed via a catheter (for TAVI/TMVR). 6. **Weaning from Bypass (Open-Heart)**: Once the new valve is secured and functioning, the heart is restarted, and the patient is gradually weaned off the heart-lung machine. 7. **Closure**: The incisions are closed, and chest tubes may be inserted to drain fluid. The sternum is wired together, and the skin incision is sutured. For transcatheter procedures, the access site (e.g., groin artery) is closed. 8. **Post-Operative Care**: The patient is transferred to the ICU for close monitoring and recovery.
Benefits
<h2>Benefits of Valve Replacement Treatment</h2> <h3>Restoring Health, Enhancing Life</h3> <ul> <li><h3>Improved Cardiac Function:</h3><p>By correcting a malfunctioning heart valve, blood flow through the heart is optimized, leading to a more efficient cardiovascular system.</p></li> <li><h3>Alleviation of Symptoms:</h3><p>Patients often experience significant relief from symptoms such as shortness of breath, chest pain, fatigue, and dizziness, allowing for a return to a more active lifestyle.</p></li> <li><h3>Increased Life Expectancy:</h3><p>For many patients with severe valvular disease, valve replacement is a life-saving procedure that can significantly extend lifespan.</p></li> <li><h3>Enhanced Quality of Life:</h3><p>Beyond extending life, the procedure dramatically improves daily well-being, enabling patients to engage in activities they previously couldn't.</p></li> <li><h3>Reduced Risk of Complications:</h3><p>Replacing a damaged valve can prevent serious complications such as heart failure, stroke, and sudden cardiac death.</p></li> <li><h3>Advanced Options:</h3><p>Access to modern techniques like TAVI/TAVR offers less invasive options for high-risk patients, promoting faster recovery and fewer complications.</p></li> </ul>
Recovery Information
<h2>Recovery and Life After Valve Replacement</h2> <h3>A Path to Renewed Health and Vitality</h3> <p>The recovery process following valve replacement varies significantly depending on the type of procedure performed (open-heart vs. minimally invasive/transcatheter) and the individual's overall health. DivinHeal provides comprehensive guidance and support throughout your recovery journey.</p> <ul> <li><h3>Immediate Post-Operative Period (Hospital Stay):</h3><p>After surgery, you will spend time in the Intensive Care Unit (ICU) for close monitoring, typically for 1-2 days. The total hospital stay for open-heart surgery is usually 5-7 days, while for TAVI, it might be as short as 2-4 days. Pain management, wound care, and early mobilization are key priorities during this phase.</p></li> <li><h3>First Few Weeks (At Home):</h3><p>Upon discharge, you'll need significant rest. For open-heart surgery, sternal precautions (avoiding heavy lifting or pushing) are crucial for 6-8 weeks. Fatigue is common. Gradually increasing activity levels under medical guidance is important. For TAVI, recovery is generally quicker, with many patients feeling much better within a couple of weeks.</p></li> <li><h3>Cardiac Rehabilitation:</h3><p>Many patients are recommended to participate in a structured cardiac rehabilitation program. This involves supervised exercise, education on heart-healthy living, and emotional support, significantly aiding recovery and long-term well-being. DivinHeal can help connect you with rehabilitation services.</p></li> <li><h3>Long-Term Wellness:</h3><p>Regular follow-up appointments with your cardiologist are essential to monitor your new valve and overall heart health. Lifelong medication management (e.g., blood thinners for mechanical valves) and lifestyle modifications such as a heart-healthy diet, regular exercise, and stress management are vital for sustaining the benefits of your valve replacement.</p></li> <li><h3>Emotional Support:</h3><p>It's normal to experience a range of emotions during recovery. DivinHeal emphasizes the importance of emotional well-being and can guide you to support groups or counseling services if needed.</p></li> </ul> <p>With proper care and adherence to medical advice, valve replacement can lead to a significant improvement in symptoms and a return to a fulfilling, active life. DivinHeal is here to support every step of this transformative journey.</p>

off pump bypass
Treatment Price
$7500.00 USDOverview of Off-Pump Bypass Surgery
Goals and Techniques of Beating-Heart Bypass
Off-pump bypass surgery aims to revascularize the heart, improving blood supply to the cardiac muscle by bypassing narrowed or blocked coronary arteries. Unlike traditional bypass surgery, this procedure is performed while the heart continues to beat, eliminating the need for a heart-lung machine. This technique can reduce the risk of certain complications, particularly for patients with specific health considerations. Surgeons use specialized instruments to stabilize small sections of the heart where the grafts are attached, ensuring precision and safety throughout the operation.
Overview of Off-Pump Bypass Surgery
Goals and Techniques of Beating-Heart Bypass
Off-pump bypass surgery aims to revascularize the heart, improving blood supply to the cardiac muscle by bypassing narrowed or blocked coronary arteries. Unlike traditional bypass surgery, this procedure is performed while the heart continues to beat, eliminating the need for a heart-lung machine. This technique can reduce the risk of certain complications, particularly for patients with specific health considerations. Surgeons use specialized instruments to stabilize small sections of the heart where the grafts are attached, ensuring precision and safety throughout the operation.
Treatment Overview
<h2>Overview of Off-Pump Bypass Surgery</h2><h3>Goals and Techniques of Beating-Heart Bypass</h3><p>Off-pump bypass surgery aims to revascularize the heart, improving blood supply to the cardiac muscle by bypassing narrowed or blocked coronary arteries. Unlike traditional bypass surgery, this procedure is performed while the heart continues to beat, eliminating the need for a heart-lung machine. This technique can reduce the risk of certain complications, particularly for patients with specific health considerations. Surgeons use specialized instruments to stabilize small sections of the heart where the grafts are attached, ensuring precision and safety throughout the operation.</p>
Procedures
Off-pump bypass surgery begins with general anesthesia. A sternotomy (incision down the center of the chest) is typically made to access the heart, though minimally invasive approaches can also be used. The surgeon then harvests healthy blood vessels, usually the internal mammary artery from the chest wall and saphenous veins from the leg, to be used as grafts. Using specialized stabilizing devices, the surgeon immobilizes a small section of the beating heart where the bypass will be performed. The harvested graft is then meticulously sutured onto the coronary artery beyond the blockage, creating a new pathway for blood flow. This process is repeated for each blocked artery. Once all grafts are in place and blood flow is confirmed, the chest incision is closed.
Benefits
<h2>Benefits of Off-Pump Bypass Surgery</h2><h3>Advantages of Beating-Heart Bypass for Patient Outcomes</h3><ul><li><strong>Reduced Risk of Complications:</strong> Avoiding the heart-lung machine can lower the risk of stroke, acute kidney injury, and neurocognitive dysfunction, especially in elderly patients or those with pre-existing conditions.</li><li><strong>Faster Recovery:</strong> Many patients experience a shorter hospital stay, quicker return to normal activities, and reduced need for blood transfusions.</li><li><strong>Less Systemic Inflammation:</strong> The absence of the cardiopulmonary bypass machine can lead to less overall inflammation in the body.</li><li><strong>Improved Outcomes for Specific Patients:</strong> Particularly beneficial for individuals with compromised lung function, kidney issues, or carotid artery disease.</li><li><strong>Lower Cost:</strong> Often associated with a more cost-effective treatment pathway due to potentially shorter ICU stays and fewer complications.</li></ul>
Recovery Information
<h2>Off-Pump Bypass Recovery Time and Tips</h2><h3>A Smooth Path to Cardiac Wellness</h3><ul><li><strong>Hospital Stay:</strong> Typically 5-7 days, including 1-2 days in the Cardiac Intensive Care Unit (ICU) for close monitoring, followed by transfer to a regular ward.</li><li><strong>Initial Recovery (Weeks 1-2):</strong> Focus on pain management, wound care, and gradual increase in mobility. Patients are encouraged to walk short distances. Deep breathing exercises are crucial to prevent lung complications.</li><li><strong>Intermediate Recovery (Weeks 3-6):</strong> Most patients can manage daily activities like dressing, light cooking, and short walks. Driving is generally not permitted during this period. Cardiac rehabilitation sessions begin, focusing on supervised exercise and lifestyle education.</li><li><strong>Full Recovery (Months 2-3 and Beyond):</strong> Significant improvement in strength and stamina. Most can return to work and resume light recreational activities. Full chest bone healing can take up to 6-12 months, requiring continued caution with heavy lifting.</li><li><strong>Lifestyle Modifications:</strong> Adopting a heart-healthy diet, regular exercise, stress management, and strictly adhering to medication schedules are vital for long-term success. DivinHeal provides guidance for sustained wellness.</li></ul>

cabg surgery
Treatment Price
$5500.00 USDCABG Surgery: Overview and Goals
The primary goal of CABG surgery is to relieve symptoms of coronary artery disease, such as angina (chest pain), shortness of breath, and fatigue, and to reduce the risk of future heart attacks or other serious cardiac events. By restoring adequate blood flow to the heart, CABG can significantly improve a patient's quality of life and prognosis. The procedure involves carefully grafting healthy vessels—often from the leg (saphenous vein) or chest (internal mammary artery)—onto the coronary arteries, bypassing the occluded segments. Modern techniques include traditional on-pump surgery, off-pump (beating heart) surgery, and minimally invasive approaches.
CABG Surgery: Overview and Goals
The primary goal of CABG surgery is to relieve symptoms of coronary artery disease, such as angina (chest pain), shortness of breath, and fatigue, and to reduce the risk of future heart attacks or other serious cardiac events. By restoring adequate blood flow to the heart, CABG can significantly improve a patient's quality of life and prognosis. The procedure involves carefully grafting healthy vessels—often from the leg (saphenous vein) or chest (internal mammary artery)—onto the coronary arteries, bypassing the occluded segments. Modern techniques include traditional on-pump surgery, off-pump (beating heart) surgery, and minimally invasive approaches.
Treatment Overview
<h3>CABG Surgery: Overview and Goals</h3><p>The primary goal of CABG surgery is to relieve symptoms of coronary artery disease, such as angina (chest pain), shortness of breath, and fatigue, and to reduce the risk of future heart attacks or other serious cardiac events. By restoring adequate blood flow to the heart, CABG can significantly improve a patient's quality of life and prognosis. The procedure involves carefully grafting healthy vessels—often from the leg (saphenous vein) or chest (internal mammary artery)—onto the coronary arteries, bypassing the occluded segments. Modern techniques include traditional on-pump surgery, off-pump (beating heart) surgery, and minimally invasive approaches.</p>
Procedures
CABG surgery typically begins with general anesthesia. The surgeon makes an incision down the center of the chest and opens the breastbone (sternotomy) to access the heart. In most cases, the heart is temporarily stopped, and a heart-lung machine takes over the functions of the heart and lungs to maintain blood circulation. The surgeon then harvests healthy blood vessels, usually from the leg (saphenous vein) or the chest wall (internal mammary artery), to use as grafts. These grafts are then meticulously sewn onto the blocked coronary arteries, bypassing the narrowed or blocked segments. Once all grafts are in place, the heart is restarted, and the heart-lung machine is gradually disconnected. The breastbone is rejoined with wires, and the incision is closed.
Benefits
<h3>Benefits of CABG Surgery</h3><ul><li><b>Relief from Angina:</b> Effectively eliminates or significantly reduces chest pain, improving daily comfort and activity levels.</li><li><b>Improved Quality of Life:</b> Patients experience increased energy, better exercise tolerance, and reduced reliance on medications.</li><li><b>Increased Life Expectancy:</b> For many patients with severe coronary artery disease, CABG can extend lifespan by reducing the risk of heart attacks and improving overall heart health.</li><li><b>Reduced Risk of Heart Attack:</b> By restoring blood flow, the surgery helps protect heart muscle from damage due to ischemia.</li><li><b>Improved Heart Function:</b> Enhanced blood supply can lead to better pumping action of the heart.</li><li><b>Long-Term Efficacy:</b> Grafted vessels, especially arterial grafts, often remain open and functional for many years.</li></ul>
Recovery Information
<h3>CABG Surgery Recovery Time and Tips</h3><ul><li><b>Hospital Stay:</b> Typically 5-7 days, including 1-2 days in the Intensive Care Unit (ICU) followed by a few days in a regular hospital ward.</li><li><b>Initial Recovery (First 2-4 Weeks):</b> Patients will experience pain or discomfort at the incision site, fatigue, and possibly mood changes. Gradual increase in activity is encouraged, but heavy lifting and strenuous activities are restricted.</li><li><b>Full Recovery:</b> Most patients can return to light activities and work within 4-6 weeks, with full recovery taking 6-12 weeks. Complete healing of the breastbone can take several months.</li><li><b>Cardiac Rehabilitation:</b> A crucial part of recovery, cardiac rehab programs involve monitored exercise, education on heart-healthy living, and emotional support. DivinHeal emphasizes participation in these programs.</li><li><b>Lifestyle Modifications:</b> Adopting a heart-healthy diet, regular exercise, smoking cessation, and managing stress are vital for long-term success and preventing further heart disease.</li><li><b>Follow-up Care:</b> Regular check-ups with your cardiologist are essential to monitor progress, manage medications, and ensure the continued health of your heart.</li></ul>

bypass surgery
Treatment Price
$5500.00 USDBypass surgery aims to significantly improve blood flow to the heart, reduce symptoms like angina (chest pain), and decrease the risk of heart attack and other severe cardiac events. The procedure involves harvesting a healthy blood vessel, typically from the leg or chest, and surgically connecting it to bypass the obstructed coronary artery, thereby creating a new path for blood to reach the heart muscle. Techniques vary, including on-pump (with heart-lung machine) and off-pump ('beating heart') bypass.
Bypass surgery aims to significantly improve blood flow to the heart, reduce symptoms like angina (chest pain), and decrease the risk of heart attack and other severe cardiac events. The procedure involves harvesting a healthy blood vessel, typically from the leg or chest, and surgically connecting it to bypass the obstructed coronary artery, thereby creating a new path for blood to reach the heart muscle. Techniques vary, including on-pump (with heart-lung machine) and off-pump ('beating heart') bypass.
Treatment Overview
Bypass surgery aims to significantly improve blood flow to the heart, reduce symptoms like angina (chest pain), and decrease the risk of heart attack and other severe cardiac events. The procedure involves harvesting a healthy blood vessel, typically from the leg or chest, and surgically connecting it to bypass the obstructed coronary artery, thereby creating a new path for blood to reach the heart muscle. Techniques vary, including on-pump (with heart-lung machine) and off-pump ('beating heart') bypass.
Procedures
Bypass surgery, or CABG, begins with the administration of general anesthesia. An incision is made in the chest to access the heart. For on-pump surgery, the heart-lung machine is connected to temporarily take over heart and lung function, allowing the heart to be stopped. For off-pump, the heart remains beating. Grafts (usually saphenous vein from the leg or internal mammary artery from the chest) are harvested. The surgeon then meticulously sews one end of the graft to the aorta and the other end to the coronary artery beyond the blockage, creating a new pathway for blood flow. Multiple bypasses may be performed depending on the number of blocked arteries. Once complete, the chest incision is closed, often with wires to hold the breastbone together.
Benefits
<h2>Benefits of Bypass Surgery</h2><ul><li><strong>Significant Symptom Relief:</strong> Effectively alleviates severe chest pain (angina) and shortness of breath caused by reduced blood flow to the heart.</li><li><strong>Improved Heart Function:</strong> Restores adequate blood supply to the heart muscle, preventing further damage and enhancing overall cardiac performance.</li><li><strong>Increased Life Expectancy:</strong> For appropriate candidates, bypass surgery can significantly improve long-term survival rates and reduce the risk of heart attack.</li><li><strong>Enhanced Quality of Life:</strong> Patients can often return to a more active lifestyle, free from debilitating symptoms, leading to a better quality of life.</li><li><strong>Reduced Need for Medications:</strong> While some medications may still be necessary, the severity and number of required drugs might decrease post-surgery.</li></ul>
Recovery Information
<h2>Recovery and Life After Bypass Surgery</h2><h3>Immediate Post-Operative Period</h3><p>Following bypass surgery, patients typically spend 1-2 days in the intensive care unit (ICU) for close monitoring. This is followed by 4-5 days in a regular hospital ward. During this time, pain management, wound care, and early mobilization are crucial. Physiotherapists will guide gentle exercises to help patients regain strength and lung function.</p><h3>At-Home Recovery (3-6 Weeks)</h3><p>The initial recovery at home usually takes about 3 to 6 weeks. Patients should avoid heavy lifting, strenuous activities, and driving during this period. Rest is vital, but light activities like walking are encouraged. Incision sites need careful monitoring for signs of infection.</p><h3>Long-Term Recovery and Rehabilitation</h3><p>Full recovery can take several months, often 2-3 months or more. A structured cardiac rehabilitation program is highly recommended. This typically includes supervised exercise, nutritional counseling, stress management, and education on heart-healthy lifestyle changes. Adhering to medication schedules and regular follow-ups with a cardiologist are essential for long-term success and preventing future cardiac issues. DivinHeal assists in coordinating these crucial recovery phases, ensuring you have the support you need.</p>

carotid angioplasty
Treatment Price
$4000.00 USDTreatment Overview
Carotid angioplasty with stenting aims to restore proper blood flow to the brain by widening narrowed carotid arteries, often caused by atherosclerosis. It involves inserting a balloon-tipped catheter to expand the artery, followed by placing a stent to keep it open, significantly reducing stroke risk. This advanced <strong>carotid angioplasty treatment</strong> is crucial for stroke prevention.
Procedures
1. **Preparation:** The patient receives local anesthesia and sometimes mild sedation. The groin area, the usual access point, is prepped and sterilized. 2. **Catheter Insertion:** A thin, flexible catheter is inserted into an artery (typically the femoral artery in the groin) and carefully guided to the carotid artery in the neck using real-time X-ray imaging (fluoroscopy). 3. **Filter Placement:** A tiny, umbrella-like filter device is often deployed beyond the narrowed section of the carotid artery to catch any plaque debris that might be dislodged during the procedure, preventing it from traveling to the brain and causing a stroke. 4. **Balloon Angioplasty:** A balloon-tipped catheter is advanced to the narrowed segment. The balloon is then inflated, gently pushing the plaque against the artery walls and widening the vessel. 5. **Stent Placement:** After the artery is opened, a self-expanding or balloon-expandable metal mesh tube, called a stent, is deployed at the site of the narrowing. The stent acts as a scaffold to keep the artery open and maintain proper blood flow. 6. **Catheter Removal:** Once the stent is securely in place, the balloon catheter and the filter device are retrieved. Pressure is applied to the access site to achieve hemostasis (stop bleeding).
Benefits
<h2>Key Benefits of Carotid Angioplasty</h2><ul><li><h3>Stroke Prevention</h3><p>Significantly reduces the risk of future strokes or transient ischemic attacks (TIAs) by restoring proper blood flow to the brain, directly addressing the primary concern of carotid artery stenosis.</p></li><li><h3>Minimally Invasive</h3><p>Compared to traditional open surgery (carotid endarterectomy), <strong>carotid angioplasty treatment</strong> involves smaller incisions, less pain, and a shorter hospital stay, contributing to a better patient experience.</p></li><li><h3>Faster Recovery</h3><p>Patients typically experience a quicker return to normal activities, often within a week, thanks to the less invasive nature of the procedure and fewer post-operative complications, leading to a shorter <strong>carotid angioplasty recovery time</strong>.</p></li><li><h3>Improved Brain Function</h3><p>By alleviating arterial narrowing, it can improve blood supply to the brain, potentially enhancing cognitive function and reducing neurological symptoms associated with insufficient blood flow.</p></li><li><h3>High Success Rate</h3><p>Modern <strong>carotid angioplasty with stenting</strong> boasts a high success rate in opening stenosed arteries and preventing recurrent blockages, especially when performed by experienced vascular specialists in advanced medical centers, contributing to long-term stroke prevention.</p></li></ul>
Recovery Information
<h2>Carotid Angioplasty Recovery Time and Tips</h2><h3>Immediate Post-Procedure Care</h3><p>After <strong>carotid angioplasty treatment</strong>, you will typically spend 1-2 days in the hospital for monitoring. The access site (usually in the groin) will be closely observed for bleeding. You'll be advised to lie flat for several hours and avoid strenuous activity to allow the entry site to heal, ensuring a smooth start to your <strong>carotid angioplasty recovery time</strong>.</p><h3>Short-Term Recovery (First Week)</h3><ul><li><strong>Activity:</strong> Avoid heavy lifting, vigorous exercise, and sudden neck movements for at least a week. Light walking is usually encouraged.</li><li><strong>Medication:</strong> It's crucial to diligently take prescribed antiplatelet medications (e.g., aspirin, clopidogrel) to prevent blood clots from forming on the stent, a key aspect of preventing recurrence.</li><li><strong>Wound Care:</strong> Keep the access site clean and dry. Report any signs of infection, swelling, or excessive pain to your healthcare provider.</li></ul><h3>Long-Term Recovery and Lifestyle Adjustments</h3><p>Full recovery and integration into normal life usually occur within 1-2 weeks. However, long-term success hinges on lifestyle modifications and adherence to medical advice for sustained stroke prevention.</p><ul><li><strong>Follow-Up:</strong> Regular follow-up appointments, including duplex ultrasound scans, are essential to monitor the stent and carotid artery health and ensure the long-term <strong>carotid angioplasty success rate</strong>.</li><li><strong>Lifestyle Changes:</strong> Adopt a heart-healthy diet, engage in regular moderate exercise, quit smoking, and manage conditions like high blood pressure, diabetes, and high cholesterol to prevent further plaque buildup.</li><li><strong>Emotional Support:</strong> Some patients may experience anxiety post-procedure. DivinHeal provides access to counseling resources to support emotional well-being throughout recovery.</li></ul><p>Adhering to these guidelines is key to maximizing the long-term benefits of your <strong>carotid angioplasty</strong> and ensuring sustained stroke prevention and a successful <strong>carotid angioplasty recovery</strong>.</p>

mitraclip
Treatment Price
$10000.00 USDThe MitraClip procedure aims to reduce severe mitral regurgitation in patients for whom open-heart surgery is deemed too risky. Using a catheter-based approach, a small clip is guided to the heart and precisely attached to the mitral valve leaflets, creating a double-orifice valve that lessens the backflow of blood. This improves the heart's pumping efficiency, alleviates symptoms like shortness of breath and fatigue, and enhances quality of life. DivinHeal connects you with leading interventional cardiologists specializing in this advanced technique, ensuring access to cutting-edge care.
The MitraClip procedure aims to reduce severe mitral regurgitation in patients for whom open-heart surgery is deemed too risky. Using a catheter-based approach, a small clip is guided to the heart and precisely attached to the mitral valve leaflets, creating a double-orifice valve that lessens the backflow of blood. This improves the heart's pumping efficiency, alleviates symptoms like shortness of breath and fatigue, and enhances quality of life. DivinHeal connects you with leading interventional cardiologists specializing in this advanced technique, ensuring access to cutting-edge care.
Treatment Overview
The MitraClip procedure aims to reduce severe mitral regurgitation in patients for whom open-heart surgery is deemed too risky. Using a catheter-based approach, a small clip is guided to the heart and precisely attached to the mitral valve leaflets, creating a double-orifice valve that lessens the backflow of blood. This improves the heart's pumping efficiency, alleviates symptoms like shortness of breath and fatigue, and enhances quality of life. DivinHeal connects you with leading interventional cardiologists specializing in this advanced technique, ensuring access to cutting-edge care.
Procedures
The MitraClip procedure is a sophisticated, minimally invasive, catheter-based intervention performed in a cardiac catheterization laboratory under general anesthesia. The step-by-step process typically involves: 1. **Vascular Access:** A small incision is made in the groin, and a catheter is inserted into the femoral vein. 2. **Transseptal Puncture:** The catheter is carefully guided through the venous system to the heart, where a small puncture is made in the interatrial septum to access the left atrium. 3. **MitraClip Delivery:** A specialized steerable guide catheter delivers the MitraClip device to the mitral valve. Using advanced imaging, particularly transesophageal echocardiography (TEE), the clip arms are precisely positioned over the diseased valve leaflets. 4. **Leaflet Grasping and Assessment:** The clip is gently closed to grasp the two leaflets of the mitral valve, bringing them together. The cardiologist then assesses the reduction in mitral regurgitation and the impact on blood flow using real-time TEE. If needed, the clip can be repositioned, retrieved, or additional clips can be implanted to achieve optimal results. 5. **Deployment and Withdrawal:** Once the desired reduction in regurgitation is achieved, the MitraClip is permanently deployed, and the delivery system and catheters are carefully withdrawn. The incision site in the groin is then closed, usually with sutures or a closure device.
Benefits
<h2>Benefits of MitraClip Treatment</h2><ul><li><h3>Minimally Invasive Procedure</h3><p>The MitraClip procedure is catheter-based, requiring only a small incision in the groin. This avoids the need for open-heart surgery, leading to less pain, reduced trauma, and a significantly faster recovery compared to traditional surgical options.</p></li><li><h3>Significant Symptom Improvement</h3><p>Patients often experience rapid and substantial relief from debilitating symptoms of mitral regurgitation, such as shortness of breath, fatigue, and fluid retention. This directly translates to an improved quality of life and enhanced capacity for daily activities and exercise.</p></li><li><h3>Reduced Hospital Stay</h3><p>The typical hospital stay after a MitraClip procedure is remarkably short, usually just 2 to 3 days. This quick discharge allows patients to return to the comfort of their homes sooner and accelerate their overall recovery process.</p></li><li><h3>High Success Rate for Targeted Patients</h3><p>For appropriately selected patients, the MitraClip procedure boasts a high success rate in effectively reducing mitral regurgitation, improving cardiac function, and significantly lowering the rates of heart failure-related hospitalizations.</p></li><li><h3>Viable for High-Risk Individuals</h3><p>It provides a crucial and life-extending treatment option for individuals who are considered too frail, elderly, or have too many co-existing medical conditions to safely undergo conventional open-heart surgery, offering them a chance at better heart health.</p></li><li><h3>Preservation of Native Valve</h3><p>Unlike valve replacement, the MitraClip repairs the native mitral valve, preserving its original structure while improving its function. This can lead to better long-term outcomes for certain patients.</p></li></ul>
Recovery Information
<h2>MitraClip Treatment Recovery Time and Tips</h2><h3>Immediate Post-Procedure Recovery</h3><p>After a MitraClip procedure, patients are typically monitored in a specialized cardiac recovery unit for 24-48 hours. Most individuals can expect to be discharged from the hospital within 2 to 3 days, a significant advantage over open-heart surgery. During this initial period, rest is crucial, and activities are limited to light ambulation within the hospital under medical supervision.</p><h3>Short-Term Recovery (First Few Weeks)</h3><ul><li><strong>Activity Restrictions:</strong> For the first 2-4 weeks, it's important to avoid heavy lifting (usually over 5-10 pounds), strenuous exercise, and any activities that put undue pressure on the groin incision site. Your cardiologist will provide specific, personalized guidelines.</li><li><strong>Wound Care:</strong> Keep the groin incision site clean and dry. Monitor for any signs of infection such as redness, swelling, increased pain, or discharge, and report them immediately to your medical team.</li><li><strong>Medications:</strong> Adhere strictly to your prescribed medication regimen, which may include blood thinners, antiplatelet drugs, and other heart medications. These are vital for preventing complications and supporting heart health.</li><li><strong>Follow-up Appointments:</strong> Regular follow-up appointments with your cardiologist, including repeat echocardiograms, are essential to monitor your heart's function, assess the effectiveness of the clip, and ensure a smooth recovery.</li></ul><h3>Long-Term Wellness and Lifestyle</h3><ul><li><strong>Cardiac Rehabilitation:</strong> Your doctor may recommend a cardiac rehabilitation program to help you gradually regain strength, improve cardiovascular fitness, and adopt a sustainable heart-healthy lifestyle.</li><li><strong>Healthy Lifestyle:</strong> Embrace a balanced diet, engage in regular light to moderate exercise as advised by your healthcare provider, avoid smoking, and diligently manage other chronic conditions like high blood pressure or diabetes.</li><li><strong>Emotional Support:</strong> It's natural to experience a range of emotions during recovery. Connecting with support groups or seeking professional counseling can be beneficial. DivinHeal can guide you to resources for comprehensive physical and emotional well-being.</li></ul><p>Most patients experience significant improvement in symptoms and can progressively return to their normal daily activities within a few weeks to a couple of months, depending on their overall health, the severity of their pre-existing heart condition, and adherence to recovery guidelines.</p>

tavi
Treatment Price
$15000.00 USDTAVI involves implanting a new aortic valve via a catheter, typically inserted through a small incision in the leg. This procedure restores proper blood flow, alleviating symptoms of aortic stenosis and significantly improving quality of life with a shorter recovery period.
TAVI involves implanting a new aortic valve via a catheter, typically inserted through a small incision in the leg. This procedure restores proper blood flow, alleviating symptoms of aortic stenosis and significantly improving quality of life with a shorter recovery period.
Treatment Overview
TAVI involves implanting a new aortic valve via a catheter, typically inserted through a small incision in the leg. This procedure restores proper blood flow, alleviating symptoms of aortic stenosis and significantly improving quality of life with a shorter recovery period.
Procedures
TAVI is performed in a catheterization laboratory or hybrid operating room. The procedure typically involves administering local anesthesia and conscious sedation, or sometimes general anesthesia. A small incision is made, usually in the groin, to access the femoral artery. A catheter, containing the folded new aortic valve, is then guided through the artery, up to the heart, and positioned within the diseased native aortic valve. Once correctly placed, the new valve is expanded, either by an inflatable balloon or by self-expansion, pushing aside the old valve leaflets. The catheter is then carefully withdrawn, and the incision site is closed. The new valve begins to function immediately, restoring normal blood flow.
Benefits
<h2>Benefits of TAVI</h2><h3>Key Advantages of Transcatheter Aortic Valve Implantation</h3><ul><li><strong>Minimally Invasive:</strong> Unlike open-heart surgery, TAVI requires only a small incision, leading to less pain and reduced scarring.</li><li><strong>Faster Recovery:</strong> Patients typically experience a significantly shorter hospital stay and quicker return to normal activities compared to traditional surgery. This translates to a more manageable <a href="#tavi-recovery-time">TAVI recovery time</a>.</li><li><strong>Reduced Risks:</strong> For high-risk surgical candidates, TAVI offers a lower risk of complications associated with major surgery, such as bleeding and infection.</li><li><strong>Improved Quality of Life:</strong> By restoring proper blood flow, TAVI effectively alleviates symptoms of aortic stenosis, such as shortness of breath and chest pain, enhancing the patient's overall well-being and life expectancy.</li><li><strong>High <a href="#tavi-success-rate">TAVI Success Rate</a>:</strong> Modern TAVI procedures boast a very high success rate, offering excellent long-term outcomes for eligible patients.</li><li><strong>Option for Inoperable Patients:</strong> TAVI provides a life-saving treatment option for patients who are deemed too frail or high-risk for conventional aortic valve replacement surgery.</li></ul>
Recovery Information
<h2>TAVI Recovery Time and Tips</h2><h3>Expected Recovery After Transcatheter Aortic Valve Implantation</h3><p>One of the significant advantages of TAVI is its relatively shorter <a href="#tavi-recovery-time">TAVI recovery time</a> compared to open-heart surgery. Most patients can expect a hospital stay of 2-5 days. During this time, medical staff will monitor your condition, manage pain, and assist with early mobilization. Many patients are able to walk within a day or two of the procedure.</p><h3>Long-Term Recovery and Lifestyle</h3><p>Full recovery, allowing for a return to normal activities, typically takes about 2-4 weeks. It is crucial to follow all post-procedure instructions, which include:</p><ul><li><strong>Medication Adherence:</strong> Regularly take prescribed medications, especially blood thinners, to prevent complications.</li><li><strong>Activity Restrictions:</strong> Avoid heavy lifting or strenuous activities for a few weeks as advised by your doctor.</li><li><strong>Wound Care:</strong> Keep the incision site clean and dry to prevent infection.</li><li><strong>Cardiac Rehabilitation:</strong> Participate in a supervised cardiac rehabilitation program to regain strength and improve heart health.</li><li><strong>Follow-Up Appointments:</strong> Attend all scheduled check-ups with your cardiologist to monitor your new valve and overall heart function.</li></ul><p>DivinHeal provides continuous support throughout your recovery, offering guidance and resources to ensure a smooth transition back to a healthy and active life. We ensure you have all the essential <a href="#tavi-recovery-tips">TAVI recovery tips</a> needed for optimal healing and sustained well-being.</p>

pci cardiology
Treatment Price
$3500.00 USDOverview of PCI Cardiology Treatment
PCI Cardiology aims to alleviate symptoms of coronary artery disease, such as angina (chest pain), and to prevent serious cardiac events like heart attacks. This procedure involves inserting a catheter into an artery (usually in the wrist or groin), guiding it to the heart, and using a balloon to widen the narrowed artery. Often, a stent (a small mesh tube) is then deployed to keep the artery open, ensuring sustained blood flow.
Overview of PCI Cardiology Treatment
PCI Cardiology aims to alleviate symptoms of coronary artery disease, such as angina (chest pain), and to prevent serious cardiac events like heart attacks. This procedure involves inserting a catheter into an artery (usually in the wrist or groin), guiding it to the heart, and using a balloon to widen the narrowed artery. Often, a stent (a small mesh tube) is then deployed to keep the artery open, ensuring sustained blood flow.
Treatment Overview
<h2>Overview of PCI Cardiology Treatment</h2><p>PCI Cardiology aims to alleviate symptoms of coronary artery disease, such as angina (chest pain), and to prevent serious cardiac events like heart attacks. This procedure involves inserting a catheter into an artery (usually in the wrist or groin), guiding it to the heart, and using a balloon to widen the narrowed artery. Often, a stent (a small mesh tube) is then deployed to keep the artery open, ensuring sustained blood flow.</p>
Procedures
PCI Cardiology begins with the insertion of a catheter into a blood vessel, typically in the groin (femoral artery) or wrist (radial artery). Guided by X-ray imaging, the catheter is advanced to the coronary arteries. A guidewire is then passed through the blockage, followed by a balloon-tipped catheter. The balloon is inflated to compress plaque against the artery walls, widening the artery. Finally, a stent (often drug-eluting) is deployed to maintain the artery's patency, and the balloon and catheter are withdrawn.
Benefits
<h2>Benefits of PCI Cardiology Treatment</h2><ul><li><h3>Improved Blood Flow</h3><p>Successfully opens blocked arteries, restoring vital blood supply to the heart.</p></li><li><h3>Relief from Angina</h3><p>Significantly reduces or eliminates chest pain and discomfort.</p></li><li><h3>Prevention of Heart Attacks</h3><p>Reduces the risk of future myocardial infarctions and related complications.</p></li><li><h3>Minimally Invasive</h3><p>Involves smaller incisions and generally less discomfort compared to open-heart surgery.</p></li><li><h3>Faster Recovery Time</h3><p>Patients typically experience a quicker return to daily activities.</p></li><li><h3>Enhanced Quality of Life</h3><p>Allows patients to live more active and symptom-free lives.</p></li></ul>
Recovery Information
<h2>Recovery and Life After PCI Cardiology</h2><h3>Immediate Recovery (1-3 Days)</h3><ul><li><b>Hospital Stay:</b> Patients typically stay in the hospital for 1-2 days for observation, monitoring, and initial recovery.</li><li><b>Activity Restriction:</b> Limited activity is recommended immediately after the procedure, especially avoiding heavy lifting or strenuous exercise.</li><li><b>Medication:</b> Adherence to prescribed antiplatelet medications (e.g., aspirin, clopidogrel) is crucial to prevent blood clots on the stent.</li></ul><h3>Long-Term Recovery and Lifestyle</h3><ul><li><b>Return to Activities:</b> Most patients can resume light activities within a few days and return to normal activities within a week after PCI Cardiology. Your cardiologist will provide specific guidance.</li><li><b>Cardiac Rehabilitation:</b> Participation in a cardiac rehabilitation program is highly recommended to improve heart health, strength, and overall well-being.</li><li><b>Lifestyle Modifications:</b> Adopting a heart-healthy lifestyle is paramount for long-term success. This includes a balanced diet, regular exercise, maintaining a healthy weight, smoking cessation, and managing conditions like high blood pressure and diabetes.</li><li><b>Follow-up Care:</b> Regular follow-up appointments with your cardiologist are essential to monitor your heart health and stent function.</li></ul>

heart stent
Treatment Price
$3500.00 USDThe primary goal of heart stent treatment is to alleviate symptoms of coronary artery disease (CAD), such as chest pain (angina), and to prevent serious cardiac events like heart attacks. By physically expanding the narrowed artery and providing structural support, a heart stent ensures sustained blood flow, improving heart function and patient quality of life. This procedure uses advanced interventional cardiology techniques, focusing on precision and patient well-being.
The primary goal of heart stent treatment is to alleviate symptoms of coronary artery disease (CAD), such as chest pain (angina), and to prevent serious cardiac events like heart attacks. By physically expanding the narrowed artery and providing structural support, a heart stent ensures sustained blood flow, improving heart function and patient quality of life. This procedure uses advanced interventional cardiology techniques, focusing on precision and patient well-being.
Treatment Overview
<p>The primary goal of heart stent treatment is to alleviate symptoms of coronary artery disease (CAD), such as chest pain (angina), and to prevent serious cardiac events like heart attacks. By physically expanding the narrowed artery and providing structural support, a heart stent ensures sustained blood flow, improving heart function and patient quality of life. This procedure uses advanced interventional cardiology techniques, focusing on precision and patient well-being.</p>
Procedures
A heart stent procedure, technically known as percutaneous coronary intervention (PCI) with stenting, begins with the patient receiving local anesthesia and sometimes mild sedation. A thin, flexible guide wire is inserted into an artery, typically in the wrist (radial approach) or groin (femoral approach). Under X-ray guidance (fluoroscopy), a catheter is threaded over the guide wire to the blocked coronary artery. A contrast dye is injected to visualize the blockages. A balloon-tipped catheter is then advanced to the narrowed segment and inflated, compressing the plaque against the artery walls. After the artery is widened, a stent (either bare-metal or drug-eluting) mounted on another balloon is positioned at the site of the blockage and expanded. The balloon is then deflated and withdrawn, leaving the stent permanently in place to hold the artery open and ensure uninterrupted blood flow. Finally, the catheter and guide wire are removed, and pressure is applied to the access site to prevent bleeding.
Benefits
<ul><li><strong>Improved Blood Flow:</strong> Immediately restores blood flow to the heart muscle, relieving angina.</li><li><strong>Reduced Heart Attack Risk:</strong> Significantly lowers the risk of future heart attacks and other cardiovascular events.</li><li><strong>Minimally Invasive:</strong> Generally performed through a small puncture, leading to less pain and faster recovery compared to open-heart surgery.</li><li><strong>Quick Recovery:</strong> Patients often return to normal activities within a few days.</li><li><strong>Enhanced Quality of Life:</strong> Alleviates symptoms, allowing patients to enjoy a more active and fulfilling life.</li><li><strong>High Success Rate:</strong> Modern stent technology offers excellent long-term outcomes for eligible patients.</li></ul>
Recovery Information
<p>Recovery after heart stent placement is typically swift. Most patients are discharged within 1 to 2 days after the procedure. Initial recovery involves monitoring the access site (usually wrist or groin) for bleeding or bruising. Patients are advised to avoid strenuous activities and heavy lifting for about a week. Adherence to prescribed antiplatelet medications (such as aspirin and clopidogrel) is crucial to prevent stent thrombosis. Long-term recovery emphasizes lifestyle modifications, including a heart-healthy diet, regular exercise, smoking cessation, and stress management, alongside regular follow-up appointments with a cardiologist to monitor progress and ensure optimal cardiac health.</p>

coronary angioplasty
Treatment Price
$4500.00 USDCoronary angioplasty, also known as percutaneous coronary intervention (PCI), is a vital treatment for coronary artery disease (CAD). It aims to relieve angina symptoms, reduce the risk of heart attack, and improve overall cardiac function by widening arteries narrowed by plaque buildup (atherosclerosis). The procedure typically uses a balloon-tipped catheter to compress plaque, often followed by the insertion of a small mesh tube called a stent to maintain vessel patency and ensure long-term patency.
Coronary angioplasty, also known as percutaneous coronary intervention (PCI), is a vital treatment for coronary artery disease (CAD). It aims to relieve angina symptoms, reduce the risk of heart attack, and improve overall cardiac function by widening arteries narrowed by plaque buildup (atherosclerosis). The procedure typically uses a balloon-tipped catheter to compress plaque, often followed by the insertion of a small mesh tube called a stent to maintain vessel patency and ensure long-term patency.
Treatment Overview
Coronary angioplasty, also known as percutaneous coronary intervention (PCI), is a vital treatment for coronary artery disease (CAD). It aims to relieve angina symptoms, reduce the risk of heart attack, and improve overall cardiac function by widening arteries narrowed by plaque buildup (atherosclerosis). The procedure typically uses a balloon-tipped catheter to compress plaque, often followed by the insertion of a small mesh tube called a stent to maintain vessel patency and ensure long-term patency.
Procedures
Coronary angioplasty is performed in a cardiac catheterization lab by an interventional cardiologist. The patient typically receives a local anesthetic at the access site (usually wrist or groin) and a mild sedative to help them relax. A small incision (puncture) is made, and a sheath (a thin plastic tube) is inserted into the artery. A guide wire is then carefully threaded through the sheath, past the aorta, and into the blocked coronary artery under X-ray guidance. Over this guide wire, a catheter with a tiny deflated balloon at its tip is advanced to the narrowed segment. The balloon is then inflated for several seconds, compressing the plaque against the artery walls and widening the vessel. This process may be repeated. In most cases, a coronary stent (a small, expandable mesh tube) is then deployed at the site of the blockage. The stent is expanded by a balloon and remains permanently in the artery to keep it open. Once the stent is in place, the balloon catheter and guide wire are removed. The sheath is withdrawn from the access site, and pressure is applied to prevent bleeding, or a closure device may be used. The entire procedure typically takes 30 minutes to a few hours, depending on the complexity and number of blockages.
Benefits
<h2>Benefits of Coronary Angioplasty Treatment</h2><p>Choosing <a href="/coronary-angioplasty-treatment">coronary angioplasty treatment</a> offers numerous significant advantages, making it a preferred option for many patients suffering from coronary artery disease:</p><ul><li><h3>Minimally Invasive:</h3><p>Unlike open-heart bypass surgery (CABG), angioplasty involves only a small puncture, leading to less pain, smaller scars, and a reduced risk of infection, contributing to a quicker <a href="/coronary-angioplasty-recovery-time-and-tips">recovery time</a>.</p></li><li><h3>Rapid Symptom Relief:</h3><p>Patients often experience immediate alleviation of chest pain (angina) and shortness of breath as blood flow to the heart is restored, significantly improving their quality of life.</p></li><li><h3>Shorter Recovery Time:</h3><p>The hospital stay is typically 1-3 days, and patients can often return to normal activities much faster than with traditional surgery, contributing to an easier <a href="/coronary-angioplasty-recovery-time-and-tips">coronary angioplasty recovery time</a>.</p></li><li><h3>Improved Heart Function:</h3><p>By opening blocked arteries, angioplasty helps prevent further damage to the heart muscle, improving overall cardiac function and reducing the risk of future heart attacks.</p></li><li><h3>High Success Rate:</h3><p>Modern techniques and advanced stent technology contribute to a very high <a href="/coronary-angioplasty-success-rate">coronary angioplasty success rate</a>, effectively restoring blood flow and providing long-term benefits for most patients.</p></li><li><h3>Enhanced Quality of Life:</h3><p>Patients can resume a more active and fulfilling life without the debilitating symptoms of coronary artery disease, engaging in activities they previously avoided.</p></li></ul>
Recovery Information
<h2>Coronary Angioplasty Recovery Time and Tips</h2><p>Understanding the <a href="/coronary-angioplasty-recovery-time-and-tips">coronary angioplasty recovery time and tips</a> is crucial for optimal outcomes. While angioplasty is less invasive than open-heart surgery, proper post-procedure care is essential for a smooth and successful recovery.</p><h3>Immediate Post-Procedure (Hospital Stay):</h3><ul><li><strong>Monitoring:</strong> You'll be closely monitored in a recovery unit for several hours to 1-2 days, depending on your condition and the access site (wrist or groin).</li><li><strong>Bed Rest:</strong> If the access site was the groin, you'll need to lie flat for several hours to prevent bleeding.</li><li><strong>Pain Management:</strong> Mild discomfort or bruising at the access site is common and can be managed with medication.</li><li><strong>Medications:</strong> You'll be prescribed antiplatelet medications (like aspirin and clopidogrel) to prevent blood clots from forming on the stent. Adherence to these is critical.</li></ul><h3>At-Home Recovery (First Few Weeks):</h3><ul><li><strong>Activity Restrictions:</strong> Avoid heavy lifting, strenuous exercise, and prolonged standing for at least a week. Your cardiologist will provide specific guidelines on resuming activities.</li><li><strong>Wound Care:</strong> Keep the access site clean and dry. Report any signs of infection (redness, swelling, discharge, fever) immediately to your doctor.</li><li><strong>Lifestyle Modifications:</strong> This is a crucial time to adopt heart-healthy habits, including a balanced diet, regular light exercise (as approved by your doctor), smoking cessation, and stress management.</li><li><strong>Cardiac Rehabilitation:</strong> Your doctor may recommend a cardiac rehab program to help you gradually regain strength and learn how to maintain heart health through structured exercise and education.</li></ul><h3>Long-Term Wellness:</h3><ul><li><strong>Medication Adherence:</strong> Continue all prescribed medications, especially antiplatelets, as directed by your cardiologist for the specified duration (often 6-12 months or longer for drug-eluting stents).</li><li><strong>Regular Follow-ups:</strong> Schedule and attend all follow-up appointments with your cardiologist to monitor your heart health, stent function, and overall recovery.</li><li><strong>Embrace a Healthy Lifestyle:</strong> Long-term success depends heavily on maintaining a heart-healthy diet, regular physical activity, managing blood pressure and cholesterol, and avoiding tobacco.</li></ul><p>With DivinHeal, you receive comprehensive guidance for your <a href="/coronary-angioplasty-recovery-time-and-tips">coronary angioplasty recovery</a>, including access to rehabilitation programs and support for long-term lifestyle changes, ensuring your journey to a healthier heart is fully supported.</p>

angioplasty
Treatment Price
$3000.00 USDAngioplasty: Restoring Heart Health
Angioplasty aims to restore optimal blood flow to the heart muscle, relieving chest pain (angina), shortness of breath, and reducing the risk of heart attack. Performed by interventional cardiologists, it involves a catheter-guided approach to mechanically open blocked arteries, primarily coronary arteries, ensuring vital oxygen and nutrients reach the heart. This procedure is a cornerstone in modern cardiovascular care, offering significant improvement in quality of life for many patients.
Angioplasty: Restoring Heart Health
Angioplasty aims to restore optimal blood flow to the heart muscle, relieving chest pain (angina), shortness of breath, and reducing the risk of heart attack. Performed by interventional cardiologists, it involves a catheter-guided approach to mechanically open blocked arteries, primarily coronary arteries, ensuring vital oxygen and nutrients reach the heart. This procedure is a cornerstone in modern cardiovascular care, offering significant improvement in quality of life for many patients.
Treatment Overview
<h2>Angioplasty: Restoring Heart Health</h2><p>Angioplasty aims to restore optimal blood flow to the heart muscle, relieving chest pain (angina), shortness of breath, and reducing the risk of heart attack. Performed by interventional cardiologists, it involves a catheter-guided approach to mechanically open blocked arteries, primarily coronary arteries, ensuring vital oxygen and nutrients reach the heart. This procedure is a cornerstone in modern cardiovascular care, offering significant improvement in quality of life for many patients.</p>
Procedures
Angioplasty typically begins with the patient receiving local anesthesia at the catheter insertion site (usually the groin or wrist). A small incision or puncture is made, and a thin guide wire is inserted into the artery, carefully maneuvered under X-ray guidance to the blocked coronary artery. A catheter with a deflated balloon at its tip is then threaded over the guide wire to the narrowed section. Once in position, the balloon is inflated for several seconds, compressing the plaque against the artery walls and widening the vessel. This process may be repeated. Following balloon inflation, a stent (a tiny mesh tube) is almost always deployed. The stent, mounted on a balloon, is expanded into place and then the balloon is deflated and removed, leaving the stent to keep the artery open. Finally, the catheter and guidewire are removed, and pressure is applied to the insertion site to stop any bleeding. The entire procedure usually takes 1 to 2 hours.
Benefits
<h2>Benefits of Angioplasty Treatment</h2><ul><li><h3>Minimally Invasive</h3><p>Unlike open-heart surgery, angioplasty involves only a small puncture, leading to less pain and scarring.</p></li><li><h3>Rapid Symptom Relief</h3><p>Quickly restores blood flow, alleviating chest pain, shortness of breath, and improving exercise tolerance.</p></li><li><h3>Faster Recovery Time</h3><p>Most patients are discharged within 1-2 days and can resume normal activities much sooner than with surgery.</p></li><li><h3>Improved Quality of Life</h3><p>Enhances cardiac function, reduces the risk of future cardiac events, and significantly improves overall well-being.</p></li><li><h3>High Success Rate</h3><p>Modern angioplasty with stent placement boasts excellent success rates in opening blocked arteries and maintaining long-term patency.</p></li></ul>
Recovery Information
<h2>Angioplasty Recovery Time and Tips</h2><h3>Immediate Post-Procedure Care</h3><p>After your <code>angioplasty treatment</code>, you'll typically spend 1-2 days in the hospital for monitoring. You may experience some bruising or soreness at the catheter insertion site (wrist or groin). Nurses will guide you on mobility and initial care.</p><h3>Returning Home and Daily Activities</h3><p>Most patients can return to light activities within a few days. Strenuous exercise, heavy lifting, and driving should be avoided for 1-2 weeks, as advised by your cardiologist. Full <code>angioplasty recovery time</code> often takes 2-4 weeks.</p><h3>Long-term Wellness & Lifestyle Modifications</h3><p>Successful <code>angioplasty recovery</code> involves crucial lifestyle changes: regular exercise, a heart-healthy diet, smoking cessation, and stress management. Adherence to prescribed medications (antiplatelet drugs, statins) is vital to prevent future blockages. DivinHeal provides resources and connects you with specialists for comprehensive post-procedural support, ensuring a smooth and sustainable recovery.</p>
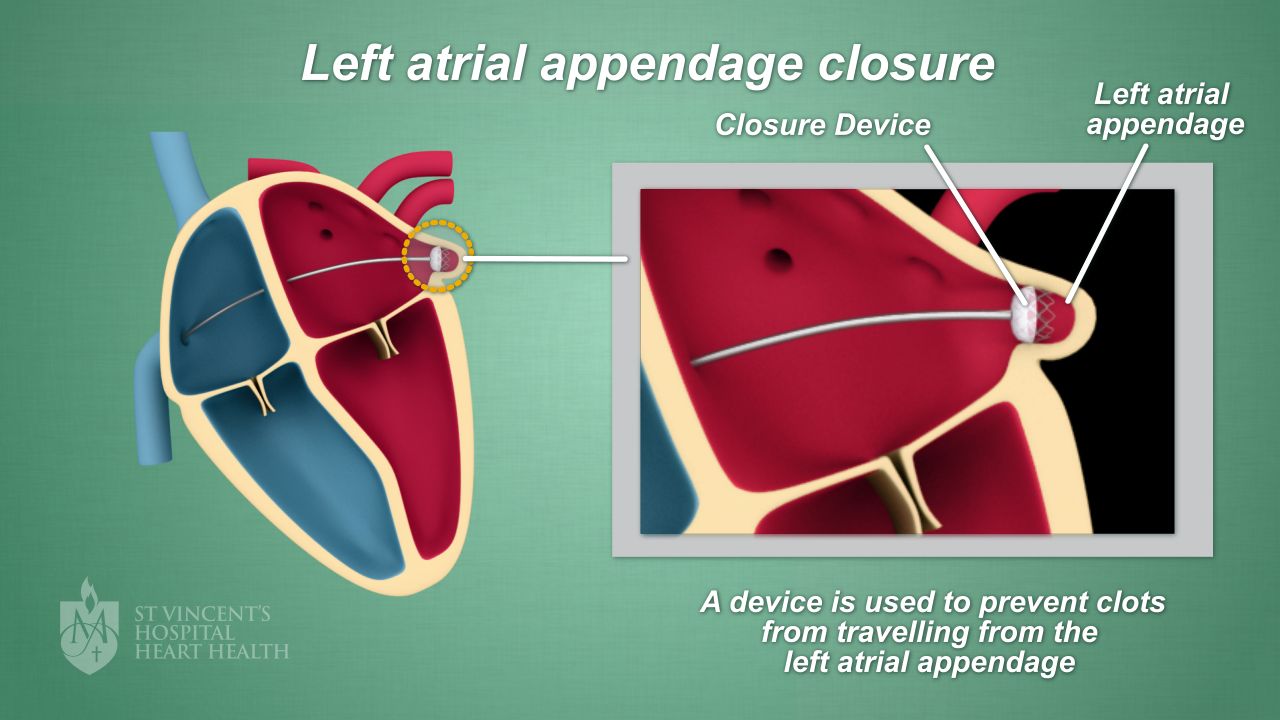
Left Atrial Appendage Closure (LAAC)
Treatment Price
$12000.00 USDLAAC treatment primarily aims to prevent stroke in individuals with non-valvular atrial fibrillation who have a high risk of stroke but also a high risk of bleeding from standard anticoagulant therapy. The procedure typically involves implanting a permanent device (like Watchman™ or Amulet™) into the left atrial appendage via a catheter, effectively sealing it off from the rest of the left atrium. This prevents blood clots from forming in the LAA and migrating to the brain, offering a crucial alternative to lifelong blood thinners.
LAAC treatment primarily aims to prevent stroke in individuals with non-valvular atrial fibrillation who have a high risk of stroke but also a high risk of bleeding from standard anticoagulant therapy. The procedure typically involves implanting a permanent device (like Watchman™ or Amulet™) into the left atrial appendage via a catheter, effectively sealing it off from the rest of the left atrium. This prevents blood clots from forming in the LAA and migrating to the brain, offering a crucial alternative to lifelong blood thinners.
Treatment Overview
LAAC treatment primarily aims to prevent stroke in individuals with non-valvular atrial fibrillation who have a high risk of stroke but also a high risk of bleeding from standard anticoagulant therapy. The procedure typically involves implanting a permanent device (like Watchman™ or Amulet™) into the left atrial appendage via a catheter, effectively sealing it off from the rest of the left atrium. This prevents blood clots from forming in the LAA and migrating to the brain, offering a crucial alternative to lifelong blood thinners.
Procedures
The Left Atrial Appendage Closure (LAAC) procedure is performed in a cardiac catheterization lab under general anesthesia. A small incision is made, typically in the groin, to access the femoral vein. A guidewire and sheath are advanced through the vein, into the right atrium of the heart. A transseptal puncture is then performed to cross the septum into the left atrium. Through this access, a specialized delivery catheter is advanced into the left atrial appendage (LAA). Using imaging guidance, such as transesophageal echocardiography (TEE) and fluoroscopy, the LAAC device (e.g., Watchman, Amulet) is carefully deployed into the opening of the LAA. Once properly positioned and confirmed to effectively seal the LAA, the device is released, and the catheter is withdrawn. The incision site is then closed.
Benefits
<h2>Benefits of Left Atrial Appendage Closure (LAAC) Treatment</h2><ul><li><h3>Effective Stroke Risk Reduction</h3><p>LAAC significantly reduces the risk of ischemic stroke in patients with atrial fibrillation, particularly for those who cannot tolerate or are contraindicated for long-term oral anticoagulation.</p></li><li><h3>Alternative to Long-Term Blood Thinners</h3><p>For patients at high bleeding risk, LAAC provides a crucial alternative to daily blood thinner medication, eliminating the associated risks of hemorrhage.</p></li><li><h3>Improved Quality of Life</h3><p>Patients can often stop or reduce their blood thinner medication after a successful LAAC procedure and a period of healing, leading to less worry about bleeding events and an improved quality of life.</p></li><li><h3>Minimally Invasive Procedure</h3><p>LAAC is performed via a transcatheter approach, meaning no open-heart surgery, resulting in smaller incisions, less pain, shorter hospital stays, and quicker recovery compared to traditional surgical methods.</p></li><li><h3>High Success Rate</h3><p>Modern LAAC devices and techniques boast high procedural success rates, offering a durable solution for stroke prevention.</p></li><li><h3>Global Access to Advanced Care via DivinHeal</h3><p>DivinHeal connects you to hospitals and interventional cardiologists utilizing the latest LAAC technologies, ensuring global standards of care, often at a fraction of the cost found in Western countries.</p></li></ul>
Recovery Information
<h2>Left Atrial Appendage Closure (LAAC) Recovery Time and Tips</h2><ul><li><h3>Immediate Post-Procedure Care</h3><p>After your LAAC procedure, you'll typically stay in the hospital for 1 to 3 days for observation. You may experience some mild discomfort at the catheter insertion site (usually the groin). Your medical team will monitor your heart rhythm and vital signs closely.</p></li><li><h3>Medication Regimen</h3><p>Patients usually follow a specific medication regimen for a period after LAAC. This often includes a combination of a blood thinner and an antiplatelet medication for a few weeks to months, allowing the tissue to grow over the implanted device. Your cardiologist will determine the exact duration based on your specific case.</p></li><li><h3>Activity Restrictions</h3><p>For the first week or two, you'll need to limit strenuous activities, heavy lifting, and intense exercise. Most patients can return to light daily activities within a few days to a week. Full recovery and return to normal activities typically occur within 4-6 weeks.</p></li><li><h3>Follow-up Appointments</h3><p>Regular follow-up appointments, including transesophageal echocardiograms (TEE) at 45 days and 6-12 months, are crucial to ensure the device is properly sealed and integrated with your heart tissue. Your DivinHeal care coordinator will assist in scheduling these follow-ups.</p></li><li><h3>Long-Term Wellness</h3><p>Maintaining a heart-healthy lifestyle, including a balanced diet, regular moderate exercise (as advised by your doctor), managing blood pressure and cholesterol, and avoiding smoking, is essential for long-term cardiac health after LAAC. DivinHeal supports your holistic recovery journey.</p></li></ul>
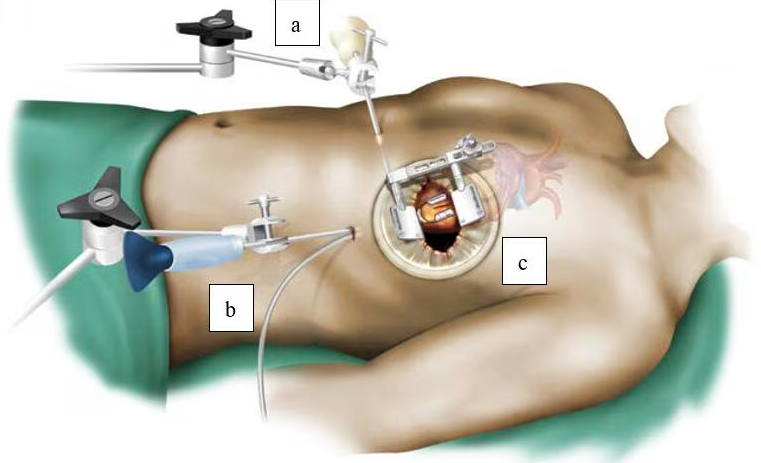
Minimally Invasive Coronary Artery Bypass Surgery (MICS CABG)
Treatment Price
$7000.00 USDMICS CABG: A Safer Approach to Heart Bypass
MICS CABG aims to restore normal blood flow to the heart muscle by bypassing blocked coronary arteries using grafts (usually arteries from the chest wall or veins from the leg). The primary goal is to alleviate symptoms like chest pain (angina), reduce the risk of heart attack, and improve overall heart function and quality of life. This technique is preferred for its reduced invasiveness, quicker return to daily activities, and excellent long-term outcomes for suitable patients.
MICS CABG: A Safer Approach to Heart Bypass
MICS CABG aims to restore normal blood flow to the heart muscle by bypassing blocked coronary arteries using grafts (usually arteries from the chest wall or veins from the leg). The primary goal is to alleviate symptoms like chest pain (angina), reduce the risk of heart attack, and improve overall heart function and quality of life. This technique is preferred for its reduced invasiveness, quicker return to daily activities, and excellent long-term outcomes for suitable patients.
Treatment Overview
<h2>MICS CABG: A Safer Approach to Heart Bypass</h2><p>MICS CABG aims to restore normal blood flow to the heart muscle by bypassing blocked coronary arteries using grafts (usually arteries from the chest wall or veins from the leg). The primary goal is to alleviate symptoms like chest pain (angina), reduce the risk of heart attack, and improve overall heart function and quality of life. This technique is preferred for its reduced invasiveness, quicker return to daily activities, and excellent long-term outcomes for suitable patients.</p>
Procedures
Minimally Invasive Coronary Artery Bypass Surgery (MICS CABG) is performed under general anesthesia. The surgeon makes a small incision (typically 2-3 inches) on the left side of the chest, usually between the ribs, without cutting the breastbone. Specialized instruments and a high-definition camera are inserted through these small incisions. The internal mammary artery, or another suitable graft vessel, is carefully harvested. The surgeon then meticulously bypasses the blocked coronary arteries by connecting the graft vessel to the coronary artery beyond the blockage, restoring blood flow. This can often be done while the heart is still beating (off-pump), reducing the need for a heart-lung machine in selected cases. Once the bypasses are complete, the incisions are closed, and drainage tubes may be placed temporarily.
Benefits
<h2>Benefits of MICS CABG</h2><ul> <li><h3>Faster Recovery and Shorter Hospital Stay</h3><p>Patients typically experience a quicker return to normal activities and a shorter duration in the hospital compared to traditional open-heart surgery, often leading to reduced overall treatment costs.</p></li> <li><h3>Reduced Pain and Scarring</h3><p>The smaller incisions lead to significantly less post-operative pain and improved cosmetic outcomes, enhancing patient comfort.</p></li> <li><h3>Lower Risk of Complications</h3><p>By avoiding sternotomy, MICS CABG reduces the risk of sternal wound infections, bleeding, and other complications associated with open-chest procedures.</p></li> <li><h3>Preservation of Chest Wall Integrity</h3><p>This approach is particularly beneficial for patients with osteopenia/osteoporosis or those who require strong upper body function post-surgery, as the breastbone remains intact.</p></li> <li><h3>High Success Rate and Durable Outcomes</h3><p>MICS CABG boasts excellent long-term patency rates for the grafts, providing effective and lasting relief from coronary artery disease symptoms and improving quality of life.</p></li></ul>
Recovery Information
<h2>MICS CABG Recovery Time and Tips</h2><p>Recovery from Minimally Invasive Coronary Artery Bypass Surgery (MICS CABG) is generally faster and less challenging than traditional CABG. While individual recovery varies, here's what patients can typically expect:</p><ul> <li><h3>Immediate Post-operative Period (1-2 weeks)</h3><p>After a few days in the ICU, you'll move to a regular ward. Pain will be managed with medication. You'll be encouraged to start light walking and breathing exercises. Hospital stay is typically 4-7 days.</p></li> <li><h3>Early Home Recovery (2-4 weeks)</h3><p>Most patients can return home within a week. You should avoid heavy lifting and strenuous activities. Gentle walks and adherence to medication schedules are crucial. Incision care is important to prevent infection.</p></li> <li><h3>Full Recovery and Rehabilitation (4-8 weeks)</h3><p>By this time, many patients can resume light daily activities and return to work (if non-strenuous). Cardiac rehabilitation plays a vital role in strengthening the heart, improving fitness, and adopting a heart-healthy lifestyle. DivinHeal can assist in coordinating post-operative rehabilitation programs.</p></li> <li><h3>Long-term Wellness</h3><p>Adopting a healthy diet, regular exercise, stress management, and diligent follow-up with your cardiologist are essential for long-term heart health after MICS CABG. DivinHeal provides resources and support for sustained wellness.</p></li></ul>
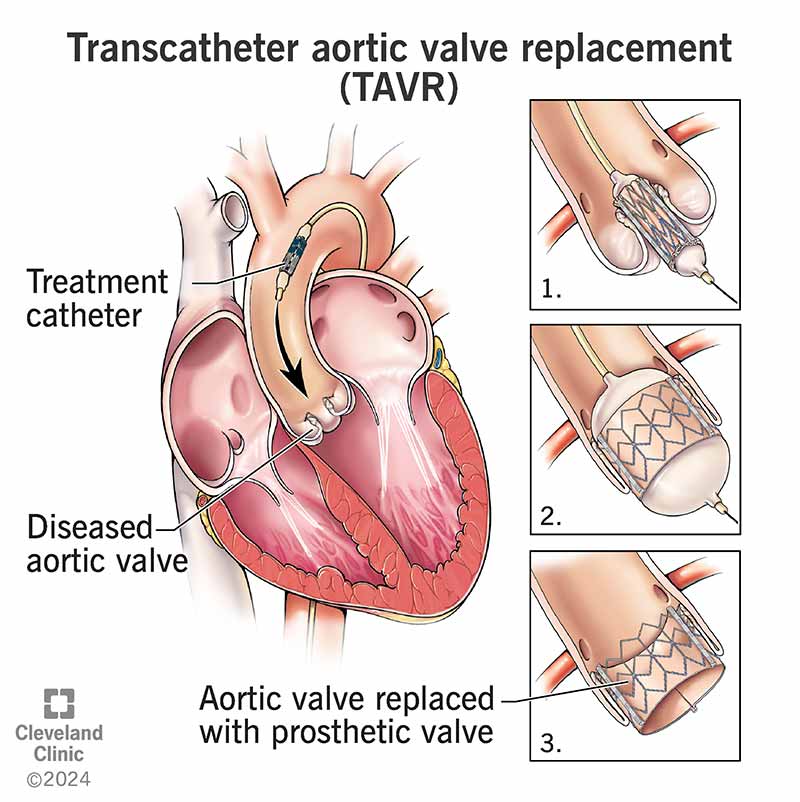
TAVR (Transcatheter Aortic Valve Replacement)
Treatment Price
$20000.00 USDTAVR: A Minimally Invasive Solution for Aortic Stenosis
TAVR is a revolutionary treatment aimed at improving heart function and quality of life for patients with severe aortic stenosis. This advanced procedure replaces a diseased aortic valve with a new, artificial one without the need for open-heart surgery. It significantly reduces recovery time and associated risks compared to conventional methods, ensuring patients can return to their daily lives sooner. DivinHeal connects you with leading cardiac centers globally, specializing in cutting-edge TAVR procedures and comprehensive post-procedure care.
TAVR: A Minimally Invasive Solution for Aortic Stenosis
TAVR is a revolutionary treatment aimed at improving heart function and quality of life for patients with severe aortic stenosis. This advanced procedure replaces a diseased aortic valve with a new, artificial one without the need for open-heart surgery. It significantly reduces recovery time and associated risks compared to conventional methods, ensuring patients can return to their daily lives sooner. DivinHeal connects you with leading cardiac centers globally, specializing in cutting-edge TAVR procedures and comprehensive post-procedure care.
Treatment Overview
<h2>TAVR: A Minimally Invasive Solution for Aortic Stenosis</h2><p>TAVR is a revolutionary treatment aimed at improving heart function and quality of life for patients with severe aortic stenosis. This advanced procedure replaces a diseased aortic valve with a new, artificial one without the need for open-heart surgery. It significantly reduces recovery time and associated risks compared to conventional methods, ensuring patients can return to their daily lives sooner. DivinHeal connects you with leading cardiac centers globally, specializing in cutting-edge TAVR procedures and comprehensive post-procedure care.</p>
Procedures
Transcatheter Aortic Valve Replacement (TAVR) involves several key steps. First, the patient undergoes thorough pre-procedure imaging, including CT scans, to precisely measure the aortic valve and surrounding structures and plan the best access route. On the day of the procedure, the patient receives anesthesia (local with sedation or general). A small incision is made, typically in the groin, to access the femoral artery. A catheter, a thin, flexible tube, is then inserted into the artery and carefully guided through the blood vessels up to the heart. The replacement valve, which is specially designed to be collapsible, is compressed onto the tip of this catheter. Once the catheter reaches the diseased aortic valve, the new valve is precisely positioned. Using fluoroscopic imaging and often echocardiography guidance, the interventional cardiologist ensures correct placement. The new valve is then expanded (either balloon-expandable or self-expanding designs), pushing the old, calcified valve leaflets aside and securing itself in place. The catheter is then withdrawn, and the access site is closed. The new valve immediately begins to function, restoring proper blood flow from the heart.
Benefits
<h2>Benefits of TAVR</h2><ul><li><h3>Minimally Invasive</h3><p>TAVR avoids open-heart surgery, meaning smaller incisions, less trauma, and no need for a heart-lung machine in most cases.</p></li><li><h3>Faster Recovery</h3><p>Patients typically experience a quicker recovery time and shorter hospital stays compared to traditional surgical aortic valve replacement (SAVR), often returning home within a few days.</p></li><li><h3>Reduced Pain & Scarring</h3><p>The minimally invasive nature results in less post-operative pain and smaller, less noticeable scars.</p></li><li><h3>Improved Quality of Life</h3><p>Effective treatment for aortic stenosis alleviates symptoms like shortness of breath and chest pain, leading to improved heart function and a better quality of life.</p></li><li><h3>Option for High-Risk Patients</h3><p>TAVR provides a vital treatment option for elderly patients or those with multiple co-morbidities who are considered high-risk for conventional open-heart surgery.</p></li><li><h3>High Success Rate</h3><p>With experienced cardiac teams and advanced technology, TAVR boasts a high success rate in restoring proper aortic valve function.</p></li></ul>
Recovery Information
<h2>TAVR Recovery Time and Tips</h2><ul><li><h3>Immediate Post-Procedure</h3><p>After TAVR, patients are typically monitored closely in the intensive care unit (ICU) for a day, then transferred to a regular hospital room. Most patients can walk within 24-48 hours.</p></li><li><h3>Hospital Stay</h3><p>The average hospital stay for TAVR is significantly shorter than open-heart surgery, usually ranging from 2 to 5 days, depending on the patient's overall health and any existing conditions.</p></li><li><h3>Home Recovery (1-2 Weeks)</h3><p>Upon discharge, patients are advised to avoid heavy lifting or strenuous activities for the first week or two. Most individuals can resume light daily activities within this period. Follow-up appointments and medication adherence are crucial.</p></li><li><h3>Full Recovery & Long-Term Wellness</h3><p>While many patients feel significantly better very quickly, a full recovery and adaptation to an improved quality of life can take several weeks. DivinHeal’s care coordination extends to guiding you on cardiac rehabilitation programs, healthy lifestyle modifications, and ongoing monitoring with your local physician to ensure long-term heart health.</p></li><li><h3>Important Tips for Recovery</h3><ul><li><strong>Medication Adherence:</strong> Take all prescribed medications, especially blood thinners, as directed.</li><li><strong>Monitor Symptoms:</strong> Report any unusual symptoms like chest pain, fever, or swelling immediately.</li><li><strong>Gradual Activity:</strong> Slowly increase your activity level as advised by your doctor.</li><li><strong>Healthy Lifestyle:</strong> Adopt a heart-healthy diet, maintain a healthy weight, and avoid smoking.</li><li><strong>Emotional Support:</strong> Seek support from family, friends, or counseling services as needed during your recovery.</li></ul></li></ul>

Minimally Invasive CABG / MIDCAB
Treatment Price
$7000.00 USDOverview of Minimally Invasive CABG (MIDCAB)
MIDCAB aims to restore blood flow to the heart muscle by bypassing narrowed or blocked coronary arteries using grafts, typically from the internal mammary artery. The procedure is performed through a small incision, usually on the left side of the chest, without requiring a sternotomy (splitting the breastbone) or often, cardiopulmonary bypass (heart-lung machine). This approach significantly reduces surgical trauma, minimizes blood loss, and accelerates the patient's return to normal activities, making it a preferred option for suitable candidates.
Overview of Minimally Invasive CABG (MIDCAB)
MIDCAB aims to restore blood flow to the heart muscle by bypassing narrowed or blocked coronary arteries using grafts, typically from the internal mammary artery. The procedure is performed through a small incision, usually on the left side of the chest, without requiring a sternotomy (splitting the breastbone) or often, cardiopulmonary bypass (heart-lung machine). This approach significantly reduces surgical trauma, minimizes blood loss, and accelerates the patient's return to normal activities, making it a preferred option for suitable candidates.
Treatment Overview
<h2>Overview of Minimally Invasive CABG (MIDCAB)</h2><p>MIDCAB aims to restore blood flow to the heart muscle by bypassing narrowed or blocked coronary arteries using grafts, typically from the internal mammary artery. The procedure is performed through a small incision, usually on the left side of the chest, without requiring a sternotomy (splitting the breastbone) or often, cardiopulmonary bypass (heart-lung machine). This approach significantly reduces surgical trauma, minimizes blood loss, and accelerates the patient's return to normal activities, making it a preferred option for suitable candidates.</p>
Procedures
Minimally Invasive Coronary Artery Bypass Grafting (MIDCAB) is typically performed under general anesthesia. The surgeon makes a small incision (usually 3-5 inches) on the left side of the chest, often between the ribs, accessing the heart without splitting the breastbone. The internal mammary artery (IMA) is carefully harvested from inside the chest wall. This artery, being naturally resistant to atherosclerosis, is then connected to the coronary artery beyond the blockage, creating a new pathway for blood flow. The procedure is usually performed on a beating heart (off-pump), meaning a heart-lung machine is often not required, further reducing surgical impact. Once the bypass is complete and blood flow is confirmed, the incision is closed with sutures or staples. Patients are then transferred to the intensive care unit for initial recovery and monitoring.
Benefits
<h2>Benefits of Minimally Invasive CABG (MIDCAB)</h2><ul><li><h3>Reduced Pain and Discomfort</h3><p>Smaller incisions mean less post-operative pain and a reduced need for strong pain medication compared to traditional open-heart surgery.</p></li><li><h3>Faster Recovery Time</h3><p>Patients typically experience a shorter hospital stay (3-5 days) and can return to normal activities and work much quicker, often within 2-4 weeks.</p></li><li><h3>Lower Risk of Complications</h3><p>Avoiding a full sternotomy and often cardiopulmonary bypass leads to a decreased risk of infection, blood loss, stroke, and other bypass machine-related complications.</p></li><li><h3>Improved Cosmetic Outcome</h3><p>The smaller incision results in a less noticeable scar, enhancing patient satisfaction.</p></li><li><h3>High Success Rate</h3><p>MIDCAB offers excellent long-term outcomes for suitable candidates, effectively restoring blood flow and improving quality of life, similar to traditional CABG.</p></li><li><h3>Preservation of Sternum Integrity</h3><p>Since the breastbone is not split, there is no sternal healing period, which is crucial for patients with certain medical conditions or those needing quicker mobilization.</p></li></ul>
Recovery Information
<h2>Minimally Invasive CABG (MIDCAB) Recovery Timeline & Tips</h2><ul><li><h3>Immediate Post-Operative Period (Hospital Stay)</h3><p>After MIDCAB, you will spend 1-2 days in the ICU for close monitoring, then move to a regular ward for another 2-3 days. During this time, nurses will assist with early mobilization, pain management, and wound care. You will be encouraged to start walking short distances.</p></li><li><h3>First 2-4 Weeks Post-Discharge (Home Recovery)</h3><p>At home, focus on gradual increase in activity. Avoid heavy lifting (over 5-10 lbs) and strenuous activities. Follow wound care instructions diligently. You can typically resume light daily activities, driving (once cleared by your surgeon), and light walking. Cardiac rehabilitation usually begins during this phase, helping you regain strength and stamina.</p></li><li><h3>2-3 Months Post-Surgery (Continued Rehabilitation)</h3><p>By this stage, most patients feel significantly better and stronger. Cardiac rehab will intensify, including supervised exercises and lifestyle counseling. You can gradually return to work and most recreational activities, always listening to your body and surgeon's advice.</p></li><li><h3>Long-Term Wellness</h3><p>Full recovery and adaptation to a heart-healthy lifestyle are ongoing. Regular follow-up appointments with your cardiologist are crucial. Adhere to medication schedules, maintain a balanced diet, engage in regular physical activity, and avoid smoking to ensure the long-term success of your MIDCAB and overall cardiovascular health.</p></li></ul>

Heart Valve Repair (Mitral/Tricuspid)
Treatment Price
$8500.00 USDOverview of Heart Valve Repair
Heart Valve Repair (Mitral/Tricuspid) is a life-changing cardiac surgical procedure aimed at correcting issues with the heart's mitral or tricuspid valves, which regulate blood flow between the heart chambers. Instead of replacing the damaged valve with an artificial one, repair techniques preserve the patient's native valve, often leading to better long-term outcomes and fewer complications like the need for lifelong anticoagulation.
At DivinHeal, we connect you with world-class cardiac surgeons and state-of-the-art facilities specializing in various Heart Valve Repair (Mitral/Tricuspid) treatment options, including annuloplasty, leaflet repair, and chordal repair. Our focus is on providing optimal care with superior Heart Valve Repair (Mitral/Tricuspid) success rates, ensuring patient safety and peace of mind.
Overview of Heart Valve Repair
Heart Valve Repair (Mitral/Tricuspid) is a life-changing cardiac surgical procedure aimed at correcting issues with the heart's mitral or tricuspid valves, which regulate blood flow between the heart chambers. Instead of replacing the damaged valve with an artificial one, repair techniques preserve the patient's native valve, often leading to better long-term outcomes and fewer complications like the need for lifelong anticoagulation.
At DivinHeal, we connect you with world-class cardiac surgeons and state-of-the-art facilities specializing in various Heart Valve Repair (Mitral/Tricuspid) treatment options, including annuloplasty, leaflet repair, and chordal repair. Our focus is on providing optimal care with superior Heart Valve Repair (Mitral/Tricuspid) success rates, ensuring patient safety and peace of mind.
Treatment Overview
<h2>Overview of Heart Valve Repair</h2><p>Heart Valve Repair (Mitral/Tricuspid) is a life-changing cardiac surgical procedure aimed at correcting issues with the heart's mitral or tricuspid valves, which regulate blood flow between the heart chambers. Instead of replacing the damaged valve with an artificial one, repair techniques preserve the patient's native valve, often leading to better long-term outcomes and fewer complications like the need for lifelong anticoagulation.</p><p>At DivinHeal, we connect you with world-class cardiac surgeons and state-of-the-art facilities specializing in various <strong>Heart Valve Repair (Mitral/Tricuspid) treatment</strong> options, including annuloplasty, leaflet repair, and chordal repair. Our focus is on providing optimal care with superior <strong>Heart Valve Repair (Mitral/Tricuspid) success rate</strong>s, ensuring patient safety and peace of mind.</p>
Procedures
Heart Valve Repair (Mitral/Tricuspid) typically involves general anesthesia. For open-heart surgery, a sternotomy (incision through the breastbone) is made. The patient is placed on a heart-lung bypass machine. The surgeon then accesses the affected valve. For mitral or tricuspid regurgitation, techniques like annuloplasty (repairing the valve's ring using a prosthetic band), leaflet repair (removing excess tissue, shortening or lengthening chords), or chordal replacement may be used. For stenosis, the valve may be widened. Once repaired, the heart is taken off bypass, and the chest is closed. Minimally invasive approaches use smaller incisions between the ribs, sometimes with robotic assistance, avoiding a full sternotomy and potentially reducing recovery time.
Benefits
<h2>Benefits of Heart Valve Repair (Mitral/Tricuspid)</h2><ul><li><h3>Preservation of Native Valve:</h3><p>Repairing the patient's own valve avoids the complexities associated with artificial valves, such as potential rejection or increased risk of infection.</p></li><li><h3>Avoidance of Lifelong Anticoagulation (Often):</h3><p>Many patients who undergo successful valve repair do not require lifelong blood thinners, reducing the risk of bleeding complications associated with mechanical valve replacements.</p></li><li><h3>Improved Cardiac Function:</h3><p>Restores proper blood flow, reducing strain on the heart and improving its pumping efficiency.</p></li><li><h3>Symptom Relief:</h3><p>Alleviates symptoms like shortness of breath, fatigue, and swelling, significantly enhancing quality of life.</p></li><li><h3>Better Long-Term Outcomes:</h3><p>Studies often show better long-term survival rates and reduced risk of complications compared to valve replacement, particularly for mitral valve repair.</p></li><li><h3>Faster Recovery (with Minimally Invasive Approaches):</h3><p>Minimally invasive or robotic techniques can lead to less pain, smaller scars, and a quicker return to normal activities during the <strong>Heart Valve Repair (Mitral/Tricuspid) recovery time</strong>.</p></li><li><h3>High Success Rate:</h3><p>Modern surgical techniques and experienced surgeons yield a very high <strong>Heart Valve Repair (Mitral/Tricuspid) success rate</strong>.</p></li></ul>
Recovery Information
<h2>Heart Valve Repair (Mitral/Tricuspid) Recovery Time and Tips</h2><p>Recovery after Heart Valve Repair varies depending on the surgical approach (open-heart vs. minimally invasive), the patient's overall health, and adherence to post-operative instructions. However, understanding the general timeline and adopting key recovery tips can significantly improve outcomes and comfort.</p><h3>Expected Recovery Timeline:</h3><ul><li><strong>Hospital Stay:</strong> Typically 5-7 days, including 1-2 days in the ICU for close monitoring.</li><li><strong>Initial Home Recovery (First 2-4 weeks):</strong> Focus on rest, gradual increase in activity, and wound care. Pain management is crucial.</li><li><strong>Mid-Term Recovery (1-3 months):</strong> Gradual return to light daily activities. Cardiac rehabilitation often begins during this phase, helping to regain strength and stamina.</li><li><strong>Full Recovery (3-6 months):</strong> Most patients can return to work and resume most normal activities. Strenuous exercise should be cleared by the cardiologist.</li></ul><h3>Recovery Tips:</h3><ul><li><strong>Follow Medical Advice Diligently:</strong> Adhere to all medication schedules, wound care instructions, and activity restrictions from your cardiac team.</li><li><strong>Cardiac Rehabilitation:</strong> Actively participate in prescribed rehabilitation programs to strengthen your heart and body.</li><li><strong>Healthy Lifestyle:</strong> Adopt a heart-healthy diet, avoid smoking and excessive alcohol, and manage stress.</li><li><strong>Gentle Exercise:</strong> Start with short, frequent walks and gradually increase duration and intensity as advised.</li><li><strong>Wound Care:</strong> Keep incisions clean and dry to prevent infection. Report any signs of redness, swelling, or discharge.</li><li><strong>Emotional Support:</strong> Seek support from family, friends, or support groups. It's normal to experience emotional fluctuations during recovery.</li><li><strong>Avoid Heavy Lifting:</strong> Especially for open-heart surgery, avoid lifting heavy objects or pushing/pulling for several weeks to protect the sternum.</li><li><strong>Regular Follow-ups:</strong> Attend all scheduled follow-up appointments with your cardiologist.</li></ul><p>DivinHeal provides continuous support and guidance throughout your <strong>Heart Valve Repair (Mitral/Tricuspid) recovery time and tips</strong>, ensuring you have the resources needed for a smooth and successful recuperation.</p>

ECMO Support (as service capability)
Treatment Price
$15000.00 USDECMO support involves circulating blood outside the body through an artificial lung (oxygenator) and back into the bloodstream, bypassing the patient's own failing heart or lungs. This provides crucial time for native organ recovery or acts as a bridge to further interventions like transplantation. DivinHeal connects patients to leading critical care units with expertise in managing complex ECMO cases, ensuring the highest standards of safety and care.
ECMO support involves circulating blood outside the body through an artificial lung (oxygenator) and back into the bloodstream, bypassing the patient's own failing heart or lungs. This provides crucial time for native organ recovery or acts as a bridge to further interventions like transplantation. DivinHeal connects patients to leading critical care units with expertise in managing complex ECMO cases, ensuring the highest standards of safety and care.
Treatment Overview
ECMO support involves circulating blood outside the body through an artificial lung (oxygenator) and back into the bloodstream, bypassing the patient's own failing heart or lungs. This provides crucial time for native organ recovery or acts as a bridge to further interventions like transplantation. DivinHeal connects patients to leading critical care units with expertise in managing complex ECMO cases, ensuring the highest standards of safety and care.
Procedures
ECMO initiation involves cannulation, where large catheters are surgically inserted into major blood vessels, typically in the neck or groin. For VV-ECMO, catheters are placed in veins to draw deoxygenated blood and return oxygenated blood. For VA-ECMO, one catheter draws blood from a vein, and another returns oxygenated blood to an artery. The blood circulates through an external circuit containing a pump (artificial heart) and an oxygenator (artificial lung). The ECMO machine meticulously controls blood flow, oxygen and carbon dioxide levels, and temperature. The patient's vital signs, blood gas levels, and the ECMO circuit parameters are continuously monitored by a specialized team of intensivists, cardiothoracic surgeons, perfusionists, and critical care nurses. Daily assessments are performed to manage anticoagulation, prevent complications like bleeding or infection, and evaluate the patient's native organ recovery. Weaning from ECMO is a gradual process, reducing support as the patient's heart and lungs improve, eventually leading to decannulation when stable.
Benefits
<h2>Benefits of ECMO Support</h2><ul><li><h3>Life-Saving Intervention:</h3><p>ECMO can be a life-saving treatment for patients with severe heart or lung failure who are not responding to conventional therapies, providing a crucial bridge to recovery or further treatment.</p></li><li><h3>Organ Rest and Recovery:</h3><p>By taking over the functions of the heart and lungs, ECMO allows these vital organs to rest, heal, and recover from acute injury or disease.</p></li><li><h3>Improved Oxygenation:</h3><p>Ensures adequate oxygen supply to the body's organs, preventing multi-organ failure and improving patient outcomes in critical situations.</p></li><li><h3>Bridge to Transplant or VAD:</h3><p>Offers a vital temporary solution for patients awaiting heart or lung transplantation, or for those needing long-term mechanical circulatory support devices like VADs.</p></li><li><h3>Enhanced Survival Rates:</h3><p>For specific conditions like severe ARDS or cardiogenic shock, ECMO has significantly improved survival rates compared to conventional treatments alone.</p></li></ul>
Recovery Information
<h2>Recovery and Life After ECMO Support</h2><p>Recovery after ECMO Support is often a long and challenging process, requiring comprehensive rehabilitation. DivinHeal ensures patients have access to robust post-ECMO care and support:</p><ul><li><h3>Immediate Post-ECMO Period:</h3><p>After decannulation (removal of ECMO tubes), patients typically remain in the ICU for close monitoring. This phase focuses on stabilizing respiratory and cardiac function and managing any immediate complications.</p></li><li><h3>Physical Rehabilitation:</h3><p>Due to prolonged immobility and critical illness, patients often experience significant muscle weakness and deconditioning (Post-Intensive Care Syndrome or PICS). Intensive physical therapy, occupational therapy, and respiratory therapy are essential to regain strength, mobility, and lung function.</p></li><li><h3>Nutritional Support:</h3><p>Optimized nutrition is crucial for recovery, muscle rebuilding, and immune system strength. Dietary plans are tailored to individual needs.</p></li><li><h3>Psychological Support:</h3><p>The experience of critical illness and ECMO can be traumatic. Many patients and their families benefit from psychological counseling, support groups, or psychiatric evaluation to address anxiety, depression, PTSD, or cognitive impairments.</p></li><li><h3>Long-Term Follow-up:</h3><p>Regular follow-up appointments with pulmonologists, cardiologists, and rehabilitation specialists are vital to monitor progress, manage chronic conditions, and address any long-term effects of critical illness. DivinHeal assists in coordinating these crucial follow-ups.</p></li><li><h3>Lifestyle Modifications:</h3><p>Depending on the underlying cause, patients may need to adopt significant lifestyle changes, including medication adherence, dietary adjustments, and regular exercise, to support long-term health and prevent recurrence.</p></li></ul><p>DivinHeal's commitment extends to facilitating this comprehensive recovery journey, connecting patients with rehabilitation centers and specialists for ongoing support.</p>

Cardiac Electrophysiology Study (EPS)
Treatment Price
$2500.00 USDUnderstanding Cardiac Electrophysiology Study (EPS)
A Cardiac Electrophysiology Study (EPS) is a minimally invasive procedure performed by a cardiac electrophysiologist to understand the heart's electrical system. Thin, flexible wires (catheters) are guided through blood vessels to the heart, where they record electrical signals and can stimulate the heart to induce and evaluate arrhythmias. The primary goal of an EPS is to accurately diagnose the type and origin of an arrhythmia, assess the risk of future heart problems, and determine the most appropriate course of treatment, often paving the way for curative procedures like catheter ablation. DivinHeal ensures access to cutting-edge facilities where these studies are performed with utmost precision and patient safety.
Understanding Cardiac Electrophysiology Study (EPS)
A Cardiac Electrophysiology Study (EPS) is a minimally invasive procedure performed by a cardiac electrophysiologist to understand the heart's electrical system. Thin, flexible wires (catheters) are guided through blood vessels to the heart, where they record electrical signals and can stimulate the heart to induce and evaluate arrhythmias. The primary goal of an EPS is to accurately diagnose the type and origin of an arrhythmia, assess the risk of future heart problems, and determine the most appropriate course of treatment, often paving the way for curative procedures like catheter ablation. DivinHeal ensures access to cutting-edge facilities where these studies are performed with utmost precision and patient safety.
Treatment Overview
<h2>Understanding Cardiac Electrophysiology Study (EPS)</h2><p>A Cardiac Electrophysiology Study (EPS) is a minimally invasive procedure performed by a cardiac electrophysiologist to understand the heart's electrical system. Thin, flexible wires (catheters) are guided through blood vessels to the heart, where they record electrical signals and can stimulate the heart to induce and evaluate arrhythmias. The primary goal of an EPS is to accurately diagnose the type and origin of an arrhythmia, assess the risk of future heart problems, and determine the most appropriate course of treatment, often paving the way for curative procedures like catheter ablation. DivinHeal ensures access to cutting-edge facilities where these studies are performed with utmost precision and patient safety.</p>
Procedures
A Cardiac Electrophysiology Study (EPS) begins with the patient lying on a procedure table in a specialized catheterization lab. After administering local anesthesia to the groin area and conscious sedation to ensure comfort, a small incision is made. Thin, flexible wires called catheters are then inserted into a vein (typically the femoral vein) and sometimes an artery. Using X-ray guidance (fluoroscopy), these catheters are carefully advanced through blood vessels to different chambers of the heart. Once in position, the catheters record the heart's electrical signals from various sites. The electrophysiologist then uses specialized equipment to deliver small electrical impulses to specific areas of the heart, attempting to induce and evaluate any arrhythmias. This 'programmed electrical stimulation' helps to map the electrical pathways and identify the precise origin of the irregular heart rhythm. If an arrhythmia is successfully induced and localized, this information is critical for planning future treatment, such as a catheter ablation. The procedure typically lasts 1-3 hours.
Benefits
<h2>Benefits of a Cardiac Electrophysiology Study (EPS)</h2><p>A Cardiac Electrophysiology Study (EPS) offers numerous significant benefits, especially for individuals suffering from unexplained heart rhythm disorders:</p><ul><li><strong>Accurate Diagnosis:</strong> EPS is considered the gold standard for precisely identifying the type, origin, and mechanism of complex arrhythmias that other tests might miss. This clarity is crucial for effective treatment planning.</li><li><strong>Guidance for Targeted Therapy:</strong> The detailed mapping provided by an EPS allows cardiac electrophysiologists to pinpoint the exact locations responsible for the arrhythmia. This information is invaluable for guiding curative procedures like catheter ablation, ensuring higher success rates.</li><li><strong>Risk Stratification:</strong> For patients with certain heart conditions or a history of fainting, EPS can assess the risk of developing dangerous, life-threatening arrhythmias, helping to determine the need for an implantable cardioverter-defibrillator (ICD).</li><li><strong>Optimized Treatment Plans:</strong> By understanding the specific electrical pathways involved, doctors can tailor medication regimens more effectively or recommend the most appropriate intervention, leading to better outcomes and improved quality of life.</li><li><strong>Improved Quality of Life:</strong> By accurately diagnosing and guiding treatment for arrhythmias, EPS can alleviate distressing symptoms such as palpitations, dizziness, and fainting, allowing patients to live more active and normal lives.</li><li><strong>Peace of Mind:</strong> For many patients, getting a definitive diagnosis and a clear treatment path for their heart rhythm disorder brings immense relief and peace of mind.</li></ul>
Recovery Information
<h2>Recovery and Life After Cardiac Electrophysiology Study (EPS)</h2><h3>Immediate Post-Procedure Recovery</h3><p>Following your Cardiac Electrophysiology Study (EPS), you will be moved to a recovery area for observation. The primary focus immediately after the procedure is to ensure the access site (usually in the groin) remains stable and to monitor for any complications. You will typically need to lie flat for 4-6 hours to prevent bleeding or bruising at the catheter insertion site. Nurses will regularly check your vital signs and the access site. Pain medication will be provided as needed, though discomfort is usually minimal.</p><h3>Hospital Stay and Discharge</h3><p>Most patients are discharged on the same day as the EPS or the following morning, depending on their condition and the electrophysiologist's assessment. Before discharge, you will receive detailed instructions on wound care, activity restrictions, and signs to watch out for that warrant medical attention. DivinHeal ensures clear communication of all post-procedure guidelines.</p><h3>At-Home Recovery and Activity</h3><ul><li><strong>Activity Restrictions:</strong> For the first 24-48 hours, avoid strenuous activities, heavy lifting, and prolonged standing or walking to allow the access site to heal.</li><li><strong>Wound Care:</strong> Keep the dressing clean and dry. You may be advised to avoid baths for a few days, opting for showers instead. Some bruising or mild soreness at the insertion site is normal.</li><li><strong>Medications:</strong> Continue all prescribed medications as instructed by your doctor.</li><li><strong>Driving:</strong> You should not drive for at least 24-48 hours after the procedure due to the effects of sedation.</li><li><strong>Return to Normal Activities:</strong> Most patients can resume light activities within 2-3 days and their normal routine within a week, based on their doctor's advice.</li></ul><h3>Long-Term Outlook and Follow-up</h3><p>After your EPS, your electrophysiologist will discuss the findings and recommend a personalized treatment plan, which could include medications, lifestyle modifications, or procedures like catheter ablation. DivinHeal's comprehensive support includes coordinating your follow-up appointments and ensuring you have access to ongoing care, fostering a path to sustained heart health and improved quality of life.</p>

Heart Failure Program (Advanced HF Management)
Treatment Price
$3500.00 USDOur Advanced Heart Failure Management program aims to provide personalized care for individuals whose heart failure symptoms persist despite standard treatments. It encompasses detailed diagnostic evaluations, advanced pharmacological interventions, consideration of device therapies like pacemakers, defibrillators, or ventricular assist devices, and comprehensive cardiac rehabilitation. The goal is to stabilize the condition, alleviate symptoms, reduce hospital readmissions, and enhance overall patient well-being through a holistic approach.
Our Advanced Heart Failure Management program aims to provide personalized care for individuals whose heart failure symptoms persist despite standard treatments. It encompasses detailed diagnostic evaluations, advanced pharmacological interventions, consideration of device therapies like pacemakers, defibrillators, or ventricular assist devices, and comprehensive cardiac rehabilitation. The goal is to stabilize the condition, alleviate symptoms, reduce hospital readmissions, and enhance overall patient well-being through a holistic approach.
Treatment Overview
Our Advanced Heart Failure Management program aims to provide personalized care for individuals whose heart failure symptoms persist despite standard treatments. It encompasses detailed diagnostic evaluations, advanced pharmacological interventions, consideration of device therapies like pacemakers, defibrillators, or ventricular assist devices, and comprehensive cardiac rehabilitation. The goal is to stabilize the condition, alleviate symptoms, reduce hospital readmissions, and enhance overall patient well-being through a holistic approach.
Procedures
The Heart Failure Program (Advanced HF Management) involves several key stages: 1. **Comprehensive Diagnostic Evaluation:** Includes advanced imaging (echocardiogram, cardiac MRI), stress tests, and blood markers to assess heart function and identify underlying causes. 2. **Personalized Treatment Plan:** A multidisciplinary team reviews findings to create an individualized plan, which may involve optimizing medications (beta-blockers, ACE inhibitors, ARBs, diuretics, novel agents like SGLT2 inhibitors). 3. **Advanced Device Therapy Evaluation:** Assessment for suitability of Implantable Cardioverter-Defibrillators (ICDs) for arrhythmia prevention, Cardiac Resynchronization Therapy (CRT) for improved pumping efficiency, or Ventricular Assist Devices (LVADs) for mechanical support. 4. **Device Implantation (if indicated):** Surgical procedure for implanting ICDs, CRTs, or LVADs. 5. **Cardiac Rehabilitation:** A structured program involving supervised exercise, nutritional counseling, and education to improve heart health and functional capacity. 6. **Continuous Monitoring & Follow-up:** Regular clinical assessments, device checks, and medication adjustments to ensure optimal management and prevent complications. 7. **Palliative Care Integration:** For some patients, integrating palliative care to improve symptom control and quality of life.
Benefits
<ul><li>Significant improvement in heart failure symptoms, such as shortness of breath and fatigue.</li><li>Enhanced quality of life and increased functional capacity.</li><li>Reduced risk of hospital readmissions due to heart failure exacerbations.</li><li>Prolonged survival rates for patients with advanced heart failure.</li><li>Access to cutting-edge device therapies and novel pharmacological treatments.</li><li>Personalized care plans tailored to individual patient needs and disease progression.</li><li>Comprehensive cardiac rehabilitation to regain strength and independence.</li><li>Expert care from multidisciplinary teams of renowned cardiologists and specialists.</li></ul>
Recovery Information
Recovery in advanced heart failure management is an ongoing process focused on stabilization and long-term well-being rather than a complete 'cure.' Post-intervention (e.g., device implantation), initial recovery might involve a hospital stay of 5-10 days. Patients will then enter a phase of cardiac rehabilitation, which can last several weeks to months, focusing on monitored exercise, education, and lifestyle modifications. Long-term recovery involves consistent adherence to medication regimens, regular follow-up appointments, diligent symptom monitoring, and maintaining a heart-healthy lifestyle. DivinHeal provides ongoing support and coordinates follow-up care to ensure sustained benefits.

Cardiac MRI
Treatment Price
$300.00 USDCardiac MRI: A Comprehensive Overview
Goals of Cardiac MRI
- Accurate diagnosis of heart diseases, including coronary artery disease, cardiomyopathy, myocarditis, and congenital heart defects.
- Assessment of heart function (ejection fraction, ventricular volumes).
- Evaluation of myocardial viability and scar tissue.
- Guidance for surgical planning and interventional procedures.
Cardiac MRI Techniques
Cardiac MRI uses strong magnetic fields and radio waves to generate detailed images. Unlike X-rays or CT scans, it does not use ionizing radiation. Contrast agents, such as gadolinium, may be used to enhance image quality and provide more specific information about blood flow and tissue characteristics.
Cardiac MRI: A Comprehensive Overview
Goals of Cardiac MRI
- Accurate diagnosis of heart diseases, including coronary artery disease, cardiomyopathy, myocarditis, and congenital heart defects.
- Assessment of heart function (ejection fraction, ventricular volumes).
- Evaluation of myocardial viability and scar tissue.
- Guidance for surgical planning and interventional procedures.
Cardiac MRI Techniques
Cardiac MRI uses strong magnetic fields and radio waves to generate detailed images. Unlike X-rays or CT scans, it does not use ionizing radiation. Contrast agents, such as gadolinium, may be used to enhance image quality and provide more specific information about blood flow and tissue characteristics.
Treatment Overview
<h2>Cardiac MRI: A Comprehensive Overview</h2><h3>Goals of Cardiac MRI</h3><ul><li>Accurate diagnosis of heart diseases, including coronary artery disease, cardiomyopathy, myocarditis, and congenital heart defects.</li><li>Assessment of heart function (ejection fraction, ventricular volumes).</li><li>Evaluation of myocardial viability and scar tissue.</li><li>Guidance for surgical planning and interventional procedures.</li></ul><h3>Cardiac MRI Techniques</h3><p>Cardiac MRI uses strong magnetic fields and radio waves to generate detailed images. Unlike X-rays or CT scans, it does not use ionizing radiation. Contrast agents, such as gadolinium, may be used to enhance image quality and provide more specific information about blood flow and tissue characteristics.</p>
Procedures
A Cardiac MRI involves lying on a movable table that slides into a large, tunnel-like scanner. You will be asked to lie still and may receive instructions via an intercom to hold your breath for short periods to ensure clear images. Electrodes will be placed on your chest to monitor your heart's electrical activity during the scan (ECG gating). An intravenous line may be started in your arm if a contrast agent is needed. The scanner produces loud knocking or buzzing noises, for which earplugs or headphones are provided. A trained technologist will monitor you throughout the entire procedure from an adjacent control room.
Benefits
<h2>Benefits of Undergoing a Cardiac MRI</h2><p>A Cardiac MRI offers numerous benefits, making it an invaluable diagnostic tool for cardiac health:</p><ul><li><strong>Highly Accurate Diagnosis:</strong> Provides clear, detailed images that help pinpoint the exact nature and extent of heart conditions, often surpassing other imaging modalities.</li><li><strong>Comprehensive Cardiac Assessment:</strong> Evaluates heart structure, function, blood flow, and tissue characteristics simultaneously.</li><li><strong>Non-Invasive and Radiation-Free:</strong> Safely performed without surgery or exposure to ionizing radiation, suitable for all ages and repeated scans.</li><li><strong>Early Detection:</strong> Can identify subtle changes in heart tissue or function before symptoms become severe, allowing for earlier intervention.</li><li><strong>Guides Treatment Planning:</strong> Crucial for cardiologists to determine the most effective treatment strategies, whether medical, interventional, or surgical.</li><li><strong>Monitors Disease Progression:</strong> Enables precise tracking of how heart conditions evolve over time and the effectiveness of ongoing therapies.</li><li><strong>Improved Patient Outcomes:</strong> By providing a definitive diagnosis, Cardiac MRI contributes significantly to better management and ultimately, improved health outcomes for patients with heart disease.</li></ul>
Recovery Information
<h2>Cardiac MRI: Immediate Post-Procedure & Follow-up</h2><p>As a non-invasive diagnostic procedure, a Cardiac MRI typically involves minimal 'recovery' time. Most patients can resume their normal activities immediately after the scan. However, there are a few considerations:</p><ul><li><h3>Immediate Post-Scan</h3><p>If a contrast agent (gadolinium) was administered, you might be asked to drink extra fluids to help flush it out of your system. There are no restrictions on eating, drinking, or physical activity unless otherwise advised by your doctor.</p></li><li><h3>Results and Consultation</h3><p>The primary 'recovery' aspect involves waiting for the radiologist's report and discussing the findings with your cardiologist. DivinHeal ensures swift report delivery and facilitates prompt follow-up consultations to interpret your results and outline the next steps in your cardiac care journey.</p></li><li><h3>Emotional Reassurance</h3><p>Receiving diagnostic results can be an anxious time. Our care coordinators are available to provide support and connect you with resources, ensuring you feel informed and reassured throughout the process. Understanding your diagnosis is the first step towards effective management and recovery of your heart health.</p></li></ul>

CT Coronary Angiography
Treatment Price
$250.00 USDOverview of CT Coronary Angiography
This advanced diagnostic procedure is crucial for detecting coronary artery disease (CAD) early and assessing its severity. It offers a detailed, 3D view of the heart's blood vessels, helping physicians plan treatment or further diagnostic steps. DivinHeal connects you with world-class hospitals in India offering state-of-the-art CT Coronary Angiography, ensuring accurate diagnosis, safety, and affordability. It's a key tool in preventive cardiology and for evaluating chest pain of unclear origin.
Overview of CT Coronary Angiography
This advanced diagnostic procedure is crucial for detecting coronary artery disease (CAD) early and assessing its severity. It offers a detailed, 3D view of the heart's blood vessels, helping physicians plan treatment or further diagnostic steps. DivinHeal connects you with world-class hospitals in India offering state-of-the-art CT Coronary Angiography, ensuring accurate diagnosis, safety, and affordability. It's a key tool in preventive cardiology and for evaluating chest pain of unclear origin.
Treatment Overview
<h3>Overview of CT Coronary Angiography</h3><p>This advanced diagnostic procedure is crucial for detecting coronary artery disease (CAD) early and assessing its severity. It offers a detailed, 3D view of the heart's blood vessels, helping physicians plan treatment or further diagnostic steps. DivinHeal connects you with world-class hospitals in India offering state-of-the-art CT Coronary Angiography, ensuring accurate diagnosis, safety, and affordability. It's a key tool in preventive cardiology and for evaluating chest pain of unclear origin.</p>
Procedures
CT Coronary Angiography involves lying on a movable table that slides into a large, donut-shaped CT scanner. An intravenous line (IV) will be inserted into a vein in your arm to administer the contrast dye. You might feel a warm flush as the dye is injected. The technologist will provide instructions, such as holding your breath for short intervals. Electrodes will be placed on your chest to monitor your heart's electrical activity (ECG) and synchronize the imaging. The scanner will rotate around you, capturing multiple X-ray images, which are then processed by a computer to create detailed 3D views of your coronary arteries.
Benefits
<h3>Benefits of CT Coronary Angiography</h3><ul><li><b>Non-Invasive:</b> Unlike conventional angiography, it does not require arterial puncture, reducing risks.</li><li><b>High Accuracy:</b> Provides highly detailed images of coronary arteries, detecting even small plaques.</li><li><b>Early Detection:</b> Allows for early diagnosis of coronary artery disease, enabling timely intervention.</li><li><b>Quick Procedure:</b> The scan itself is typically very fast, minimizing patient discomfort.</li><li><b>Comprehensive Information:</b> Can assess not only the lumen of the arteries but also the vessel walls and surrounding structures.</li><li><b>Risk Stratification:</b> Helps in accurately assessing a patient's risk for future cardiac events.</li><li><b>Affordable CT Coronary Angiography packages:</b> Especially in India, offering world-class care at a fraction of the cost in Western countries.</li></ul>
Recovery Information
<h3>Recovery and Life After CT Coronary Angiography</h3><p>Recovery from a CT Coronary Angiography is typically very straightforward as it is a non-invasive diagnostic procedure. You can usually resume your normal activities immediately after the scan. The primary focus of recovery is to ensure the contrast dye is flushed out of your system. You will be advised to drink plenty of fluids for the next 24 hours.</p><ul><li><b>Immediate Post-Procedure:</b> You may be monitored for a short period to ensure there are no adverse reactions to the contrast dye.</li><li><b>Hydration:</b> Crucial for kidney health to help eliminate the contrast agent from your body.</li><li><b>Results:</b> A radiologist will interpret your images, and your cardiologist will discuss the findings with you, usually within a few days.</li><li><b>Follow-up:</b> Based on the results, your doctor will recommend further steps, which could include lifestyle modifications, medication, or additional diagnostic or interventional procedures.</li><li><b>No Downtime:</b> There is generally no downtime, and you can drive and return to work or daily routines immediately.</li></ul>

Aortic Aneurysm Repair (Open/Endovascular)
Treatment Price
$7000.00 USDAortic Aneurysm Repair focuses on stabilizing or replacing the aneurysmal segment of the aorta to avert its potentially fatal rupture. Treatment goals include preventing complications, restoring normal blood flow, and ensuring long-term aortic health. Techniques range from complex open surgery, which involves directly replacing the damaged section with a synthetic graft, to advanced endovascular procedures (EVAR or TEVAR) where a stent-graft is deployed minimally invasively through catheters to reinforce the vessel wall.
Aortic Aneurysm Repair focuses on stabilizing or replacing the aneurysmal segment of the aorta to avert its potentially fatal rupture. Treatment goals include preventing complications, restoring normal blood flow, and ensuring long-term aortic health. Techniques range from complex open surgery, which involves directly replacing the damaged section with a synthetic graft, to advanced endovascular procedures (EVAR or TEVAR) where a stent-graft is deployed minimally invasively through catheters to reinforce the vessel wall.
Treatment Overview
Aortic Aneurysm Repair focuses on stabilizing or replacing the aneurysmal segment of the aorta to avert its potentially fatal rupture. Treatment goals include preventing complications, restoring normal blood flow, and ensuring long-term aortic health. Techniques range from complex open surgery, which involves directly replacing the damaged section with a synthetic graft, to advanced endovascular procedures (EVAR or TEVAR) where a stent-graft is deployed minimally invasively through catheters to reinforce the vessel wall.
Procedures
<h3>Open Aortic Aneurysm Repair:</h3><ol><li><strong>Anesthesia:</strong> General anesthesia is administered.</li><li><strong>Incision:</strong> A large incision is made in the abdomen or chest, depending on the aneurysm's location.</li><li><strong>Aorta Isolation:</strong> The diseased section of the aorta is exposed, and clamps are placed above and below the aneurysm to temporarily stop blood flow.</li><li><strong>Aneurysm Excision & Graft Placement:</strong> The aneurysm is opened, and a synthetic graft (usually made of Dacron) is carefully sewn into place, replacing the weakened segment.</li><li><strong>Closure:</strong> The native aortic wall is often wrapped around the new graft, and the incision is closed with sutures or staples.</li></ol><h3>Endovascular Aneurysm Repair (EVAR/TEVAR):</h3><ol><li><strong>Anesthesia:</strong> Local, regional, or general anesthesia may be used.</li><li><strong>Access:</strong> Small incisions are made, typically in both groins, to access the femoral arteries.</li><li><strong>Catheter Guidance:</strong> Catheters and guidewires are inserted and carefully advanced under X-ray guidance to the site of the aneurysm.</li><li><strong>Stent-Graft Deployment:</strong> A compressed stent-graft is delivered through the catheter and precisely deployed within the aorta, spanning the aneurysm. The graft expands and adheres to the healthy aortic wall, creating a new pathway for blood flow and excluding the aneurysm.</li><li><strong>Confirmation & Closure:</strong> Angiography is performed to confirm proper graft placement and ensure no leaks (endoleaks). The access sites in the groin are then closed.</li></ol>
Benefits
<h2>Benefits of Aortic Aneurysm Repair (Open/Endovascular)</h2><ul><li><h3>Life-Saving Intervention:</h3> The most critical benefit is the prevention of a potentially fatal aortic rupture.</li><li><h3>Improved Quality of Life:</h3> Alleviates symptoms such as pain or discomfort related to the aneurysm, and provides peace of mind.</li><li><h3>High Success Rates:</h3> Modern surgical and endovascular techniques boast excellent success rates when performed by experienced vascular surgeons.</li><li><h3>Minimally Invasive Option (EVAR):</h3> Endovascular repair offers shorter hospital stays, less post-operative pain, smaller incisions, and faster recovery for suitable candidates.</li><li><h3>Long-Term Durability:</h3> Both open repair with synthetic grafts and stent-grafts in EVAR are designed for long-lasting structural integrity of the aorta.</li><li><h3>Access to Expert Care via DivinHeal:</h3> Connect with top vascular surgeons for Aortic Aneurysm Repair and state-of-the-art facilities globally, especially in India, ensuring world-class outcomes.</li></ul>
Recovery Information
<h2>Aortic Aneurysm Repair Recovery Time and Tips</h2><p>Recovery from Aortic Aneurysm Repair varies significantly between open surgery and endovascular repair (EVAR).</p><h3>Open Repair Recovery:</h3><ul><li><strong>Hospital Stay:</strong> Typically 5-10 days, including time in the ICU initially.</li><li><strong>Full Recovery:</strong> Can take 6-12 weeks, with gradual return to normal activities.</li><li><strong>Pain Management:</strong> Managed with medication, gradually decreasing over weeks.</li><li><strong>Activity Restrictions:</strong> Avoid heavy lifting and strenuous activity for several weeks to months.</li><li><strong>Wound Care:</strong> Incision site needs careful monitoring for infection.</li></ul><h3>EVAR Recovery:</h3><ul><li><strong>Hospital Stay:</strong> Typically 2-4 days, often without an ICU stay.</li><li><strong>Full Recovery:</strong> Often much faster, 2-4 weeks for most light activities.</li><li><strong>Pain Management:</strong> Generally less pain, managed with oral medication.</li><li><strong>Activity Restrictions:</strong> Lighter restrictions, but still advised to avoid heavy lifting for a few weeks.</li><li><strong>Wound Care:</strong> Small groin incisions require less intensive care.</li></ul><h3>General Recovery Tips:</h3><ul><li><strong>Follow Medical Advice:</strong> Adhere strictly to your surgeon’s post-operative instructions, medication regimen, and follow-up schedule.</li><li><strong>Gradual Activity:</strong> Slowly increase activity levels as tolerated, starting with short walks.</li><li><strong>Healthy Lifestyle:</strong> Adopt a heart-healthy diet, manage blood pressure, quit smoking, and maintain a healthy weight to support long-term aortic health.</li><li><strong>Regular Follow-ups:</strong> Essential for monitoring the repair and detecting any complications, especially after EVAR which requires periodic imaging.</li><li><strong>Emotional Support:</strong> Seek support from family, friends, or counseling services as needed during your recovery journey.</li></ul>
Meet Our Doctors
Meet our team of highly qualified and experienced medical professionals dedicated to providing the best healthcare services.

Anjana Kharbanda
Sr. Consultant - Emergency
Emergency & Trauma Services
New Delhi
22+ Years
Experience
Artemis Hospital
Hospital
1500
Fees

Chandragouda Dodagoudar
Consultant
Cardiology
New Delhi
14+ Years
Experience
Apolo Delhi
Hospital
1500
Fees

Dr. Abhinandan
Sr. Consultant - Urology & Kidney Transplant Program (Unit I)
Organ Transplant, Urology
New Delhi
8+ Years
Experience
Artemis Hospital
Hospital
1500
Fees

Dr. Abhishek Gupta
Consultant - Internal Medicine
Internal Medicine
New Delhi
12+ Years
Experience
Apolo Delhi
Hospital
1500
Fees

Dr. Ajay Kumar
Chairman - Gastroenterology & Hepatology - Pan Max and HOD - BLK Institute for Digestive & Liver Diseases
Gastroenterology, Hepatology & Endoscopy
New Delhi
38+ Years
Experience
Max Hospital,Gurgaon
Hospital
1500
Fees

Dr. Ajay Kumar Gupta
Principal Consultant, Internal Medicine
Internal Medicine
New Delhi
25+ Years
Experience
Apolo Delhi
Hospital
1500
Fees

Dr Amit Jassal
Principal Consultant - Anaesthesia
Anaesthesia
New Delhi
15+ Years
Experience
Artemis Hospital
Hospital
1500
Fees

Dr. Amit Kumar Chaurasia
Chief Cath Lab & TAVI (Unit I), Director TAVI/TAVR and Structural Heart Disease and Senior Consultant Cardiology
Cardiology, Interventional Cardiology, TAVI / TAVR & Structural Heart Diseases
New Delhi
16+ Years
Experience
Artemis Hospital
Hospital
1500
Fees

Dr. Anand Kumar Saxena
Director - CTVS
Cardiac Surgery
New Delhi
27+ Years
Experience
Apolo Delhi
Hospital
1500
Fees

Dr. Anil Kumar Kansal
Director
Cardiology
New Delhi
24+ Years
Experience
Apolo Delhi
Hospital
1500
Fees

Dr. Anil Vardani
Director & Head - Cardiac Sciences
Cardiology
New Delhi
23+ Years
Experience
Apolo Delhi
Hospital
1500
Fees
Dr. Aniruddha Vidyadhar Kulkarni
Director - Cardiac Sciences
Cardiology
New Delhi
21+ Years
Experience
Apolo Delhi
Hospital
1500
Fees

Dr. Anjani Kumar Agrawal
Associate Director - Internal Medicine
Internal Medicine
New Delhi
31+ Years
Experience
Apolo Delhi
Hospital
1500
Fees

Dr. Arun Dewan
Principal Director (Critical Care) & Director (Internal Medicine)
Internal Medicine, Critical Care
New Delhi
40+ Years
Experience
Max Hospital,Gurgaon
Hospital
1500
Fees

Dr. Ashok Kumar Jhingan
Director - Cardiology
Cardiology
New Delhi
37+ Years
Experience
Apolo Delhi
Hospital
1500
Fees

Dr. Atul Prasad
Vice Chairman & HOD, Neurology Department at BLK-Max Super Speciality Hospital, New Delhi
Neurology
New Delhi
15+ Years
Experience
Max Hospital,Gurgaon
Hospital
1500
Fees

Dr. Balbir Singh
Chairman of Cardiology, Pan Max Healthcare
Cardiology, Interventional Cardiology, Electrophysiology
New Delhi
29+ Years
Experience
Max Hospital,Gurgaon
Hospital
1500
Fees

Dr. Bhushan Nariani
Chairman - Orthopaedics (Joint Diseases & Joint Replacement)
Orthopaedics, Joint Replacement, Robotic Surgery
New Delhi
25+ Years
Experience
Max Hospital,Gurgaon
Hospital
1500
Fees

Dr. Bijoy Kumar Nayak
Director - Cardiac Sciences
Cardiology
New Delhi
18+ Years
Experience
Apolo Delhi
Hospital
1500
Fees

Dr. Bipin Kumar Dubey
HOD - Cardiology
Cardiology
New Delhi
40+ Years
Experience
Max Hospital,Gurgaon
Hospital
1500
Fees