Centres Of Excellence
Our Centres of Excellence bring together multidisciplinary teams to deliver precise diagnosis, advanced treatments, and superior outcomes across a wide spectrum of medical specialties.

Related Links
Doctors For Treatment in Similar Locations
Treatments in India for Visitors
Other Treatments Nearby
Related Links
Best Hospital Near by for treatment
Doctors For Treatment in Similar Locations
Treatments in India for Visitors
- Oncology Treatment in Pune for Bangladesh
- Oncology Treatment in Bengaluru for Nigeria
- Oncology Treatment in Pune for Nigeria
- Oncology Treatment in Gurugram for Iraq
- Oncology Treatment in Gurugram for Bangladesh
- Oncology Treatment in Chennai for Iraq
- Oncology Treatment in India for Iraq
- Oncology Treatment in Mumbai for Bangladesh
- Oncology Treatment in Mumbai for Nigeria
- Oncology Treatment in Chennai for Ethiopia
- Oncology Treatment in Gurugram for Ethiopia
- Oncology Treatment in New Delhi for UAE
- Oncology Treatment in India for Ethiopia
- Oncology Treatment in Bengaluru for Ethiopia
- Oncology Treatment in Pune for Ethiopia
- Oncology Treatment in Pune for UAE
- Oncology Treatment in Gurugram for UAE
- Oncology Treatment in Gurugram for Nigeria
- Oncology Treatment in Hyderabad for UAE
- Oncology Treatment in New Delhi for Nigeria
- Oncology Treatment in India for UAE
- Oncology Treatment in Bengaluru for Iraq
- Oncology Treatment in Chennai for UAE
- Oncology Treatment in India for Nigeria
- Oncology Treatment in Pune for Iraq
- Oncology Treatment in Hyderabad for Ethiopia
- Oncology Treatment in New Delhi for Ethiopia
- Oncology Treatment in Mumbai for Ethiopia
- Oncology Treatment in Hyderabad for Iraq
- Oncology Treatment in Bengaluru for UAE
- Oncology Treatment in Hyderabad for Bangladesh
- Oncology Treatment in Mumbai for UAE
- Oncology Treatment in Chennai for Bangladesh
- Oncology Treatment in New Delhi for Bangladesh
- Oncology Treatment in Chennai for Nigeria
- Oncology Treatment in Hyderabad for Nigeria
- Oncology Treatment in India for Bangladesh
Other Treatments Nearby
Related Links
- Oncology Success Rate in India
- Oncology cost in Hyderabad
- Oncology cost in Bengaluru
- Oncology cost in Haryana
- Oncology cost in Mumbai
- Oncology cost in Pune
- Oncology cost in New Delhi
- Oncology cost in India
- Oncology Success Rate in Hyderabad
- Oncology Success Rate in Pune
- Oncology cost in Chennai
- Oncology Success Rate in New Delhi
Related Treatments

thyroid cancer surgery
Treatment Price
$0.00 USDNo overview available
No overview available
Treatment Overview
No overview available
Procedures
No procedure details available
Benefits
No benefits information available
Recovery Information
No recovery information available

colorectal cancer surgery
Treatment Price
$5000.00 USDOverview of Colorectal Cancer Surgery
Colorectal cancer surgery aims to remove cancerous tissue from the colon or rectum, prevent its spread, and restore digestive function. Procedures range from minimally invasive resections to more extensive operations like colectomy or proctectomy, often combined with chemotherapy or radiation therapy. DivinHeal ensures access to renowned colorectal surgeons and comprehensive care pathways for effective colorectal cancer treatment.
Overview of Colorectal Cancer Surgery
Colorectal cancer surgery aims to remove cancerous tissue from the colon or rectum, prevent its spread, and restore digestive function. Procedures range from minimally invasive resections to more extensive operations like colectomy or proctectomy, often combined with chemotherapy or radiation therapy. DivinHeal ensures access to renowned colorectal surgeons and comprehensive care pathways for effective colorectal cancer treatment.
Treatment Overview
<h2>Overview of Colorectal Cancer Surgery</h2><p>Colorectal cancer surgery aims to remove cancerous tissue from the colon or rectum, prevent its spread, and restore digestive function. Procedures range from minimally invasive resections to more extensive operations like colectomy or proctectomy, often combined with chemotherapy or radiation therapy. DivinHeal ensures access to renowned colorectal surgeons and comprehensive care pathways for effective <strong>colorectal cancer treatment</strong>.</p>
Procedures
Colorectal cancer surgery typically begins with general anesthesia. For open surgery, a single larger incision is made in the abdomen. For laparoscopic or robotic surgery, several small incisions are made, through which a camera and surgical instruments are inserted. The surgeon carefully identifies and isolates the cancerous section of the colon or rectum, along with a margin of healthy tissue and nearby lymph nodes. Blood vessels supplying the segment are ligated. The diseased portion is then removed. The remaining healthy ends of the bowel are reconnected (anastomosis) using sutures or surgical staples. In some cases, if reconnection is not immediately possible or safe, an ostomy (colostomy or ileostomy) is created, where a segment of the bowel is brought through an opening in the abdominal wall (stoma) to allow waste to exit into a collection bag. Drains may be placed to remove excess fluid, and incisions are closed with sutures or staples.
Benefits
<h2>Benefits of Colorectal Cancer Surgery</h2><ul><li><h3>High Cure Rates</h3><p>For early and localized colorectal cancer, surgery offers the highest chance of cure and long-term survival. Modern techniques contribute to an improved <strong>colorectal cancer success rate</strong>.</p></li><li><h3>Symptom Relief</h3><p>Surgical removal of the tumor can alleviate debilitating symptoms such as bowel obstruction, bleeding, pain, and fatigue, significantly improving the patient's quality of life.</p></li><li><h3>Accurate Staging</h3><p>Surgery allows for precise pathological staging of the cancer by examining the removed tissue and lymph nodes, which is critical for guiding subsequent treatment decisions.</p></li><li><h3>Reduced Recurrence Risk</h3><p>Combined with adjuvant therapies, surgical resection effectively removes primary tumors and minimizes the risk of local and distant recurrence.</p></li><li><h3>Access to Advanced Techniques</h3><p>DivinHeal's network provides access to minimally invasive (laparoscopic, robotic) and advanced open surgical techniques, leading to faster recovery, less pain, and smaller scars.</p></li></ul>
Recovery Information
<h2>Colorectal Cancer Surgery Recovery Time and Tips</h2><p>The <strong>colorectal cancer recovery time and tips</strong> vary depending on the extent of surgery, type of procedure (open vs. minimally invasive), and individual patient factors. Generally, hospital stays range from 5 to 10 days.</p><ul><li><h3>Immediate Post-Operative Period</h3><p>Patients typically experience pain managed with medication. Early mobilization (walking) is encouraged to prevent complications like blood clots and stimulate bowel function. A liquid diet progresses to soft foods as tolerated.</p></li><li><h3>First Few Weeks at Home (2-4 weeks)</h3><p>Patients gradually regain strength. Fatigue is common. Restrictions on heavy lifting and strenuous activities are typically advised. If an ostomy was created, patients receive education and support for its care.</p></li><li><h3>Full Recovery (6-12 weeks)</h3><p>Most patients can return to light activities and work within 4-8 weeks, with full recovery often taking 3-6 months. Physical therapy, dietary adjustments, and emotional support may be recommended. Regular follow-up with the oncology team is crucial for monitoring recovery and detecting any signs of recurrence.</p></li><li><h3>Long-Term Wellness</h3><p>Lifestyle modifications, including a healthy diet, regular exercise, and avoiding smoking and excessive alcohol, are important for long-term health and reducing recurrence risk. DivinHeal's care coordinators provide comprehensive guidance throughout this period.</p></li></ul>

bladder cancer surgery
Treatment Price
$6500.00 USDOverview of Bladder Cancer Surgery Treatment
Bladder cancer surgery is designed to remove malignant tissue and, in some cases, the entire bladder to prevent cancer spread. The primary goal is to achieve complete remission or significantly control the disease while preserving quality of life. Techniques vary widely, from endoscopic resection for early-stage cancers to complex open or robotic-assisted radical cystectomy with urinary diversion for advanced cases. DivinHeal ensures access to leading medical professionals proficient in the latest surgical innovations, offering hope and advanced care.
Overview of Bladder Cancer Surgery Treatment
Bladder cancer surgery is designed to remove malignant tissue and, in some cases, the entire bladder to prevent cancer spread. The primary goal is to achieve complete remission or significantly control the disease while preserving quality of life. Techniques vary widely, from endoscopic resection for early-stage cancers to complex open or robotic-assisted radical cystectomy with urinary diversion for advanced cases. DivinHeal ensures access to leading medical professionals proficient in the latest surgical innovations, offering hope and advanced care.
Treatment Overview
<h2>Overview of Bladder Cancer Surgery Treatment</h2><p>Bladder cancer surgery is designed to remove malignant tissue and, in some cases, the entire bladder to prevent cancer spread. The primary goal is to achieve complete remission or significantly control the disease while preserving quality of life. Techniques vary widely, from endoscopic resection for early-stage cancers to complex open or robotic-assisted radical cystectomy with urinary diversion for advanced cases. DivinHeal ensures access to leading medical professionals proficient in the latest surgical innovations, offering hope and advanced care.</p>
Procedures
Bladder cancer surgery encompasses several approaches. For early-stage, non-muscle invasive cancer, Transurethral Resection of Bladder Tumor (TURBT) is performed endoscopically through the urethra, using a resectoscope to shave off tumors. For muscle-invasive disease, a Partial Cystectomy removes only the cancerous part of the bladder, while a Radical Cystectomy involves removing the entire bladder, surrounding lymph nodes, and often adjacent organs (prostate/seminal vesicles in men, uterus/ovaries in women). Following radical cystectomy, a urinary diversion procedure is performed: either an ileal conduit (creating a stoma for an external collection bag) or a neobladder (creating an internal bladder from intestine, connected to the urethra). Robotic-assisted laparoscopic radical cystectomy is an increasingly common minimally invasive approach, offering quicker recovery.
Benefits
<h2>Benefits of Bladder Cancer Surgery</h2><h3>Positive Outcomes and Enhanced Quality of Life</h3><ul><li><h4>Effective Tumor Removal</h4><p>Surgical intervention is often the most definitive way to remove cancerous tissue, especially for muscle-invasive disease, offering the best chance for cure or long-term remission.</p></li><li><h4>Improved Prognosis</h4><p>Timely and expertly performed bladder cancer surgery significantly improves survival rates and reduces the risk of recurrence.</p></li><li><h4>Disease Control and Symptom Relief</h4><p>Surgery can alleviate symptoms caused by the tumor, such as pain, bleeding, or urinary obstruction, improving the patient's immediate quality of life.</p></li><li><h4>Personalized Treatment Paths</h4><p>With various surgical options (TURBT, partial, or radical cystectomy), treatment can be tailored to the specific stage and characteristics of the cancer, optimizing outcomes.</p></li><li><h4>Access to Advanced Techniques</h4><p>DivinHeal connects patients with hospitals offering robotic-assisted surgery, leading to smaller incisions, reduced blood loss, faster recovery, and greater surgical precision.</p></li><li><h4>Holistic Support for Recovery</h4><p>Beyond the surgery, comprehensive care ensures rehabilitation, emotional support, and guidance on adapting to life post-surgery, including management of urinary diversion.</p></li></ul>
Recovery Information
<h2>Bladder Cancer Surgery Recovery Time and Tips</h2><h3>A Guided Path to Wellness</h3><p>The recovery period following bladder cancer surgery varies significantly depending on the type of procedure performed:</p><ul><li><h4>Transurethral Resection of Bladder Tumor (TURBT)</h4><p>Typically, patients can return home within 1-2 days. Full recovery, including resolution of urinary discomfort and slight bleeding, usually takes 1-2 weeks. It's crucial to drink plenty of fluids and avoid strenuous activities.</p></li><li><h4>Partial Cystectomy</h4><p>Hospital stay is generally 3-5 days. Full recovery can take 4-6 weeks, during which physical activity should be restricted. A urinary catheter may be in place for some time.</p></li><li><h4>Radical Cystectomy with Urinary Diversion</h4><p>This is a major surgery requiring a longer hospital stay, typically 5-10 days. Full recovery can take 6-12 weeks or more. Patients will need to learn to manage their urinary diversion (e.g., stoma care for an ileal conduit or bladder training for a neobladder). Physical therapy and support are vital during this period.</p></li></ul><h3>General Recovery Tips:</h3><ul><li><strong>Follow Medical Advice:</strong> Adhere strictly to your surgeon's instructions regarding wound care, medication, and activity restrictions.</li><li><strong>Pain Management:</strong> Take prescribed pain relievers as directed to manage discomfort.</li><li><strong>Hydration:</strong> Drink ample fluids to help flush the urinary system and prevent complications.</li><li><strong>Gradual Activity:</strong> Slowly increase your activity level as tolerated. Avoid heavy lifting or strenuous exercise initially.</li><li><strong>Nutrition:</strong> Maintain a balanced diet to support healing. Your care team may recommend specific dietary adjustments, especially for urinary diversion.</li><li><strong>Emotional Support:</strong> It's normal to experience emotional challenges. Seek support from family, friends, or professional counselors, which DivinHeal can facilitate.</li><li><strong>Stoma Care (if applicable):</strong> If you have an ileal conduit, meticulous stoma care is essential to prevent skin irritation and infection. Our care coordinators will ensure you receive proper training.</li><li><strong>Regular Follow-ups:</strong> Adhere to all scheduled post-operative appointments for monitoring and surveillance.</li></ul>

interventional oncology
Treatment Price
$5000.00 USDInterventional oncology treatments leverage state-of-the-art imaging (ultrasound, CT, MRI, fluoroscopy) to precisely guide instruments into the body to deliver therapy directly to cancerous tumors. The primary goals include local tumor destruction (e.g., ablation), blocking blood supply to tumors (e.g., embolization), and targeted drug delivery, minimizing systemic side effects and preserving healthy tissue.
Interventional oncology treatments leverage state-of-the-art imaging (ultrasound, CT, MRI, fluoroscopy) to precisely guide instruments into the body to deliver therapy directly to cancerous tumors. The primary goals include local tumor destruction (e.g., ablation), blocking blood supply to tumors (e.g., embolization), and targeted drug delivery, minimizing systemic side effects and preserving healthy tissue.
Treatment Overview
Interventional oncology treatments leverage state-of-the-art imaging (ultrasound, CT, MRI, fluoroscopy) to precisely guide instruments into the body to deliver therapy directly to cancerous tumors. The primary goals include local tumor destruction (e.g., ablation), blocking blood supply to tumors (e.g., embolization), and targeted drug delivery, minimizing systemic side effects and preserving healthy tissue.
Procedures
Interventional oncology procedures typically follow a structured approach. First, the patient undergoes advanced imaging (CT, MRI, ultrasound) to precisely map the tumor's location and characteristics. Prior to the procedure, access is gained, usually through a small incision or needle puncture in the skin, guided by real-time imaging. A catheter, needle, or probe is then carefully advanced to the tumor. Once in position, the chosen therapeutic agent is delivered – this could be heat (radiofrequency/microwave ablation), cold (cryoablation), chemotherapy drugs (chemoembolization), or radioactive particles (radioembolization). The treatment delivery is closely monitored with imaging to ensure complete coverage of the tumor while sparing healthy surrounding tissue. After the treatment is complete, the instruments are withdrawn, and the access site is closed, often with just a small bandage.
Benefits
<h2>Benefits of Interventional Oncology Treatment</h2><ul><li><h3>Minimally Invasive</h3><p>Procedures involve tiny incisions or needle punctures, resulting in less pain, reduced blood loss, and minimal scarring compared to traditional open surgery.</p></li><li><h3>Highly Targeted Therapy</h3><p>Image guidance allows for precise targeting of tumors, minimizing damage to surrounding healthy tissues and reducing systemic side effects.</p></li><li><h3>Shorter Recovery Times</h3><p>Patients often experience quicker interventional oncology recovery time, allowing for shorter hospital stays and a faster return to daily activities.</p></li><li><h3>Improved Quality of Life</h3><p>By effectively controlling tumors and managing symptoms, interventional oncology can significantly enhance a patient's quality of life.</p></li><li><h3>Option for Inoperable Tumors</h3><p>These techniques offer viable treatment options for patients whose tumors are deemed inoperable due to size, location, or overall health status.</p></li><li><h3>Adjunctive Therapy</h3><p>Can be effectively combined with other interventional oncology chemotherapy and radiation therapy, or targeted and hormonal therapy, to improve overall outcomes.</p></li></ul>
Recovery Information
<h2>Interventional Oncology Recovery Time and Tips</h2><p>Recovery from interventional oncology procedures is generally much faster and less complex than traditional surgery. The exact interventional oncology recovery time depends on the specific procedure, the type of cancer, and your overall health.</p><ul><li><h3>Immediate Post-Procedure</h3><p>Most patients will spend a few hours to overnight in observation after the procedure. Pain is usually managed with oral medication and is typically mild to moderate.</p></li><li><h3>Hospital Stay</h3><p>For many procedures, the hospital stay is often 1-3 days. Some outpatient procedures might allow same-day discharge.</p></li><li><h3>Return to Activity</h3><p>Patients can typically resume light activities within a few days to a week. Strenuous activities and heavy lifting may be restricted for 2-4 weeks to ensure proper healing at the access site.</p></li><li><h3>Pain and Side Effects</h3><p>Some procedures, like TACE, may cause "post-embolization syndrome" (fever, pain, nausea) for a few days, which is manageable with medication. Ablation sites may have localized soreness.</p></li><li><h3>Long-term Wellness Tips</h3><ul><li>Follow all post-procedure instructions from your interventional oncologist carefully.</li><li>Maintain a healthy diet and stay hydrated.</li><li>Engage in gentle physical activity as advised to aid circulation and recovery.</li><li>Attend all scheduled follow-up appointments for imaging and blood tests to monitor treatment effectiveness and overall health.</li><li>Consider emotional counseling or support groups to manage the psychological aspects of cancer recovery.</li></ul></li></ul>

debulking surgery cancer
Treatment Price
$6000.00 USDDebulking surgery's primary goal is to significantly reduce the tumor burden (cytoreduction), thereby making residual cancer more susceptible to adjuvant therapies and mitigating mass-effect symptoms. Techniques are highly variable, tailored to the tumor's location and extent, frequently involving extensive resection and, in some cases, specialized procedures like Hyperthermic Intraperitoneal Chemotherapy (HIPEC) for certain advanced abdominal cancers.
Debulking surgery's primary goal is to significantly reduce the tumor burden (cytoreduction), thereby making residual cancer more susceptible to adjuvant therapies and mitigating mass-effect symptoms. Techniques are highly variable, tailored to the tumor's location and extent, frequently involving extensive resection and, in some cases, specialized procedures like Hyperthermic Intraperitoneal Chemotherapy (HIPEC) for certain advanced abdominal cancers.
Treatment Overview
Debulking surgery's primary goal is to significantly reduce the tumor burden (cytoreduction), thereby making residual cancer more susceptible to adjuvant therapies and mitigating mass-effect symptoms. Techniques are highly variable, tailored to the tumor's location and extent, frequently involving extensive resection and, in some cases, specialized procedures like Hyperthermic Intraperitoneal Chemotherapy (HIPEC) for certain advanced abdominal cancers.
Procedures
1. **Pre-operative Assessment:** Comprehensive evaluation including advanced imaging (CT, MRI, PET scans), biopsies, and assessment of overall health and fitness for major surgery. Detailed discussions with oncologists, surgeons, and anesthesiologists. 2. **Anesthesia:** General anesthesia is administered, ensuring the patient is completely unconscious and pain-free throughout the procedure. 3. **Incision:** A major surgical incision is made, typically a midline incision for abdominal cancers, to provide wide and clear access to the tumor site and surrounding tissues. 4. **Exploration and Resection:** The surgeon meticulously explores the affected area, identifying all visible tumor sites. The primary tumor, metastatic lesions, and any visibly affected organs or lymph nodes are carefully and extensively removed. This may involve partial or complete removal of organs like intestines, ovaries, uterus, peritoneum, or other structures, with the goal of achieving optimal cytoreduction (leaving no visible disease larger than 1 cm). 5. **Reconstruction (if necessary):** Depending on the extent of organ removal, immediate reconstructive procedures may be performed, such as bowel re-anastomosis or the creation of an ostomy. 6. **Adjunctive Therapies (Optional):** For specific indications, such as peritoneal carcinomatosis, Hyperthermic Intraperitoneal Chemotherapy (HIPEC) may be administered immediately after tumor removal while the abdomen is still open, delivering heated chemotherapy directly to the abdominal cavity. 7. **Closure:** The surgical site is carefully closed in layers, and drains may be placed to manage any post-operative fluid accumulation. 8. **Post-operative Care:** Patients are transferred to a recovery unit or intensive care for close monitoring of vital signs, pain management, fluid balance, and early mobilization to prevent complications.
Benefits
<h2>Key Benefits of Debulking Surgery Cancer Treatment</h2><ul><li><h3>Significant Tumor Reduction</h3><p>The primary benefit is the substantial reduction in tumor mass, which effectively alleviates severe symptoms such as pain, pressure, or organ obstruction caused by large tumors. This immediately improves the patient's comfort and quality of life.</p></li><li><h3>Enhanced Efficacy of Adjuvant Therapies</h3><p>By drastically reducing the number of cancer cells, debulking surgery makes subsequent treatments, such as chemotherapy and radiation therapy, significantly more effective. With less tumor burden, these therapies can more efficiently target and eliminate residual cancer cells.</p></li><li><h3>Potential for Extended Survival</h3><p>For patients who achieve optimal debulking (leaving minimal or no visible residual disease), studies have shown a potential for extended progression-free survival and overall survival, offering a longer and healthier life trajectory.</p></li><li><h3>Improved Quality of Life</h3><p>Beyond survival, debulking surgery often leads to a marked improvement in the patient’s overall quality of life. By managing disease-related complications and symptoms, patients can engage more actively in daily life and recover better emotionally.</p></li><li><h3>Accurate Pathological Assessment</h3><p>The surgical removal of significant tumor tissue allows for a more comprehensive pathological assessment, which can provide critical information for personalized treatment planning, including identifying specific cancer subtypes or genetic markers.</p></li></ul>
Recovery Information
<h2>Debulking Surgery Cancer Recovery Time and Tips</h2><p>Recovery from debulking surgery cancer treatment is a significant process that varies based on the extent of the surgery, the patient's overall health, and any subsequent adjuvant therapies. DivinHeal supports you through every phase of your debulking surgery cancer recovery, providing comprehensive guidance and coordination.</p><h3>Expected Recovery Timeline:</h3><ul><li><strong>Initial Hospital Stay:</strong> Typically ranges from 7-14 days. This period focuses on immediate post-operative care, pain management, monitoring for complications, and initiation of early mobilization.</li><li><strong>Early Home Recovery:</strong> The first 2-4 weeks post-discharge involve continued rest, gradual increase in activity, and meticulous wound care. You will likely feel fatigued and require assistance with daily tasks.</li><li><strong>Full Physical Recovery:</strong> Complete physical recovery can take several weeks to months, often 6-12 weeks, especially if extensive organ resection was performed. During this time, you will gradually regain strength and stamina.</li><li><strong>Return to Normal Activities:</strong> Light activities may resume within 4-6 weeks, but strenuous activities, heavy lifting, and demanding work might need to be avoided for 3-6 months, or as advised by your surgeon.</li></ul><h3>Recovery Tips for Optimal Healing:</h3><ul><li><strong>Adhere to Medical Advice:</strong> Strictly follow all post-operative instructions from your medical team, including medication schedules, wound care, and activity restrictions.</li><li><strong>Pain Management:</strong> Do not hesitate to use prescribed pain medication. Effective pain control is crucial for comfort, mobility, and healing.</li><li><strong>Nutrition:</strong> Maintain a healthy, balanced diet rich in protein and nutrients to support tissue repair and boost immunity. Hydration is also vital.</li><li><strong>Gradual Mobilization:</strong> Gentle walking is encouraged early on to prevent complications like blood clots and aid bowel function. Gradually increase activity as tolerated, but avoid overexertion.</li><li><strong>Physical Therapy:</strong> If recommended, engage actively in physical therapy to regain strength, flexibility, and mobility, particularly if extensive abdominal surgery or organ removal was involved.</li><li><strong>Emotional Support:</strong> Debulking surgery and cancer diagnosis can be emotionally taxing. Seek support from family, friends, support groups, or professional counselors. DivinHeal can connect you with mental health resources.</li><li><strong>Monitor for Complications:</strong> Be vigilant for signs of infection (fever, redness, pus at incision site), excessive pain, swelling, or any unusual symptoms, and report them to your care team immediately.</li><li><strong>Regular Follow-ups:</strong> Attend all scheduled follow-up appointments to monitor your progress, assess healing, and plan for any further adjuvant therapies.</li></ul><p>DivinHeal provides continuous care coordination, ensuring you have the resources and support needed for a smooth and comprehensive recovery, including access to affordable debulking surgery packages that encompass post-operative care.</p>

palliative cancer surgery
Treatment Price
$4000.00 USDOverview of Palliative Cancer Surgery
Relief and Comfort Through Expert Care
Palliative cancer surgery is a crucial component of comprehensive cancer care for patients facing advanced or metastatic disease. Unlike curative surgery, its primary goal is to address specific symptoms that significantly impair a patient's quality of life. This can include relieving blockages in the digestive or respiratory tracts, reducing tumor bulk causing pain or pressure, stopping bleeding, or stabilizing fractures due to bone metastases. DivinHeal connects you with leading oncological surgeons who specialize in these intricate procedures, ensuring expert care focused on your comfort and dignity. Our network of accredited hospitals in India offers state-of-the-art facilities for these vital interventions, prioritizing patient safety and compassionate outcomes.
Overview of Palliative Cancer Surgery
Relief and Comfort Through Expert Care
Palliative cancer surgery is a crucial component of comprehensive cancer care for patients facing advanced or metastatic disease. Unlike curative surgery, its primary goal is to address specific symptoms that significantly impair a patient's quality of life. This can include relieving blockages in the digestive or respiratory tracts, reducing tumor bulk causing pain or pressure, stopping bleeding, or stabilizing fractures due to bone metastases. DivinHeal connects you with leading oncological surgeons who specialize in these intricate procedures, ensuring expert care focused on your comfort and dignity. Our network of accredited hospitals in India offers state-of-the-art facilities for these vital interventions, prioritizing patient safety and compassionate outcomes.
Treatment Overview
<h2>Overview of Palliative Cancer Surgery</h2><h3>Relief and Comfort Through Expert Care</h3><p>Palliative cancer surgery is a crucial component of comprehensive cancer care for patients facing advanced or metastatic disease. Unlike curative surgery, its primary goal is to address specific symptoms that significantly impair a patient's quality of life. This can include relieving blockages in the digestive or respiratory tracts, reducing tumor bulk causing pain or pressure, stopping bleeding, or stabilizing fractures due to bone metastases. DivinHeal connects you with leading oncological surgeons who specialize in these intricate procedures, ensuring expert care focused on your comfort and dignity. Our network of accredited hospitals in India offers state-of-the-art facilities for these vital interventions, prioritizing patient safety and compassionate outcomes.</p>
Procedures
Palliative cancer surgery encompasses a wide range of procedures, each tailored to alleviate specific symptoms caused by advanced cancer. While the exact steps vary greatly depending on the type of cancer and the targeted symptom, a general outline includes: 1. <b>Pre-operative Assessment:</b> Comprehensive evaluation of the patient's overall health, cancer stage, symptom severity, and suitability for surgery. This involves imaging (CT, MRI, PET scans), blood tests, and consultations with oncologists, surgeons, anesthesiologists, and palliative care specialists. 2. <b>Anesthesia:</b> General anesthesia is typically administered to ensure the patient is unconscious and pain-free throughout the procedure. Regional anesthesia may be used in conjunction for specific pain control. 3. <b>Surgical Access:</b> The surgeon makes an incision to access the affected area. The size and location of the incision depend on the surgical goal (e.g., abdominal for bowel obstruction, chest for lung issues, limb for bone lesions). Minimally invasive techniques (laparoscopy, thoracoscopy) may be used if appropriate to reduce recovery time. 4. <b>Symptom-Specific Intervention:</b> <ul> <li><b>For Obstruction (Bowel, Urinary, Airway):</b> Removal of a portion of the tumor, bypassing the obstruction (e.g., creating a stoma or bypass), or inserting a stent to keep the passage open.</li> <li><b>For Bleeding:</b> Ligating bleeding vessels, resecting the bleeding tumor, or using cautery to stop hemorrhage.</li> <li><b>For Pain/Pressure:</b> Debulking a tumor pressing on nerves or organs, nerve blocks, or stabilization of fractured bones with plates/rods.</li> <li><b>For Fluid Accumulation (Pleural/Pericardial Effusion):</b> Drainage of fluid, insertion of a drain, or pleurodesis (to prevent fluid recurrence).</li> </ul> 5. <b>Closure:</b> After achieving the palliative goal, the surgical site is closed layer by layer, and dressings are applied. 6. <b>Post-operative Care:</b> Patients are moved to a recovery area for close monitoring of vital signs, pain management, and observation for any immediate complications.
Benefits
<h2>Benefits of Palliative Cancer Surgery</h2><h3>Enhancing Life Quality and Comfort</h3><ul><li><h4>Significant Symptom Relief</h4><p>The primary and most profound benefit is the alleviation of distressing symptoms such as severe pain, chronic bleeding, or obstructions in vital organs. This can dramatically improve daily comfort and reduce reliance on heavy medication.</p></li><li><h4>Improved Quality of Life</h4><p>By controlling symptoms, palliative surgery helps patients regain a sense of normalcy, allowing them to participate more in daily activities, spend quality time with loved ones, and experience a better overall sense of well-being.</p></li><li><h4>Prevention of Complications</h4><p>Surgical intervention can prevent life-threatening complications like complete bowel obstruction, severe internal bleeding, or spinal cord compression, which can lead to further suffering and urgent medical crises.</p></li><li><h4>Enhanced Functional Independence</h4><p>Relieving pain or improving organ function can restore a degree of physical independence, allowing patients to move more freely, eat more comfortably, or breathe easier.</p></li><li><h4>Psychological and Emotional Well-being</h4><p>Reducing physical distress often leads to a significant improvement in mental and emotional health, fostering a more positive outlook and reducing anxiety or depression associated with advanced cancer.</p></li><li><h4>Reduced Hospitalizations</h4><p>By proactively addressing potential complications, palliative surgery can sometimes decrease the need for frequent emergency room visits or prolonged hospital stays for symptom management.</p></li><li><h4>Customized Care</h4><p>Palliative surgical plans are highly individualized, tailored to the specific needs and goals of each patient, ensuring that the intervention directly targets their most pressing symptoms.</p></li></ul>
Recovery Information
<h2>Recovery After Palliative Cancer Surgery: Focused on Comfort and Well-being</h2><h3>A Personalized Path to Enhanced Comfort</h3><p>Recovery following palliative cancer surgery is highly individualized, depending on the type and extent of the surgery, the patient's overall health, and the stage of their cancer. Unlike recovery from curative surgery which often emphasizes a return to full activity, recovery from palliative surgery prioritizes comfort, symptom management, and a quick return to baseline functional status with improved quality of life.</p><h3>Immediate Post-Operative Period (Hospital Stay)</h3><ul><li><h4>Pain Management</h4><p>Effective pain control is paramount. You will receive tailored pain medication, often through intravenous lines or epidurals initially, transitioning to oral medications as soon as possible. Our medical teams are highly skilled in managing post-surgical pain for cancer patients.</p></li><li><h4>Monitoring & Care</h4><p>Nurses and doctors will closely monitor your vital signs, wound healing, and any surgical drains. Early detection and management of complications are crucial.</p></li><li><h4>Early Mobilization</h4><p>Gentle movement, such as sitting up and short walks, is encouraged early to prevent complications like blood clots and pneumonia, always within your comfort level.</p></li><li><h4>Nutritional Support</h4><p>Depending on the surgery, you may start with clear liquids and gradually advance your diet. Nutritional counseling is often provided to ensure adequate intake and support healing.</p></li><li><h4>Emotional Support</h4><p>The emotional impact of advanced cancer and surgery is recognized. Support teams are available to provide counseling and comfort for both patients and families.</p></li></ul><h3>Returning Home & Long-Term Wellness (Post-Discharge)</h3><ul><li><h4>Activity Levels</h4><p>Your surgical team will provide specific guidelines on activity restrictions. The goal is to gradually increase activity without overexertion, focusing on what improves your comfort and daily function.</p></li><li><h4>Wound Care</h4><p>Clear instructions for wound care will be provided to prevent infection and promote healing. DivinHeal's coordinators can assist with follow-up appointments and home care coordination.</p></li><li><h4>Medication Management</h4><p>You will likely be discharged with prescriptions for pain relief and other supportive medications. Understanding your medication schedule is vital.</p></li><li><h4>Ongoing Palliative Care</h4><p>Palliative surgery is often part of a broader palliative care plan. This may involve ongoing pain clinics, symptom management, nutritional support, and psychological counseling to ensure sustained well-being.</p></li><li><h4>Lifestyle Adjustments</h4><p>Focus on aspects that enhance your quality of life: gentle exercise, balanced nutrition, adequate rest, and engaging in activities you enjoy within your physical limits.</p></li><li><h4>Follow-up Appointments</h4><p>Regular follow-ups with your oncologist and palliative care team are essential to monitor your recovery, manage any persistent symptoms, and adjust your overall care plan as needed.</p></li></ul><p>DivinHeal ensures continuous support throughout your recovery, facilitating communication with your medical team and providing resources for a comfortable and dignified post-surgical period, aligning with your goals for enhanced quality of life.</p>

stem cell transplant cancer
Treatment Price
$25000.00 USDStem cell transplant cancer treatment involves replacing damaged or diseased bone marrow with healthy blood-forming stem cells. This procedure aims to cure certain cancers by enabling patients to receive aggressive cancer therapies that would otherwise be fatal. It restores the immune system and blood-producing capacity, offering renewed hope for long-term remission and survival. The primary goal is to eradicate cancer cells and rebuild a healthy hematopoietic system.
Stem cell transplant cancer treatment involves replacing damaged or diseased bone marrow with healthy blood-forming stem cells. This procedure aims to cure certain cancers by enabling patients to receive aggressive cancer therapies that would otherwise be fatal. It restores the immune system and blood-producing capacity, offering renewed hope for long-term remission and survival. The primary goal is to eradicate cancer cells and rebuild a healthy hematopoietic system.
Treatment Overview
Stem cell transplant cancer treatment involves replacing damaged or diseased bone marrow with healthy blood-forming stem cells. This procedure aims to cure certain cancers by enabling patients to receive aggressive cancer therapies that would otherwise be fatal. It restores the immune system and blood-producing capacity, offering renewed hope for long-term remission and survival. The primary goal is to eradicate cancer cells and rebuild a healthy hematopoietic system.
Procedures
The stem cell transplant cancer treatment procedure involves several distinct phases: 1. **Patient Evaluation:** Comprehensive medical tests to assess overall health, cancer stage, and suitability for transplant. 2. **Donor Selection (for Allogeneic):** Identifying a compatible donor, often through HLA (Human Leukocyte Antigen) matching. This can be a related donor (sibling), unrelated donor, or umbilical cord blood. 3. **Stem Cell Collection:** * **Autologous:** Patient's own stem cells are mobilized from bone marrow into the bloodstream using growth factors, then collected via apheresis and cryopreserved. * **Allogeneic:** Donor's stem cells are collected either from peripheral blood (most common) or directly from bone marrow under anesthesia. 4. **Conditioning Regimen:** High-dose chemotherapy, sometimes combined with radiation therapy, is administered over several days. This aims to destroy remaining cancer cells and suppress the immune system to prevent rejection of transplanted cells. This is an intense period with significant side effects. 5. **Stem Cell Infusion:** The collected stem cells (autologous or allogeneic) are thawed and infused intravenously, similar to a blood transfusion. The cells then travel to the bone marrow and begin the process of engraftment (settling in and producing new blood cells). 6. **Engraftment and Recovery:** This is the critical phase where the patient's new bone marrow begins to function. Close monitoring for infections, bleeding, and other complications is essential. Growth factors may be administered to stimulate blood cell production. 7. **Post-Transplant Care:** Long-term follow-up includes managing medications, monitoring for complications like Graft-versus-Host Disease (GvHD), and providing supportive care. This phase extends for months to years, with gradual recovery of immune function.
Benefits
The primary benefits of stem cell transplant cancer treatment include: <ul> <li><strong>Potential for Cure:</strong> For many blood cancers, it offers the best chance for long-term remission or cure.</li> <li><strong>Enables High-Dose Therapy:</strong> Allows patients to receive very aggressive chemotherapy and/or radiation doses that would otherwise be lethal to bone marrow.</li> <li><strong>Restores Immune System:</strong> Rebuilds a healthy immune system capable of fighting infections and, in allogeneic transplants, potentially targeting residual cancer cells (graft-versus-leukemia effect).</li> <li><strong>Improved Survival Rates:</strong> Significantly improves survival rates for specific types of leukemia, lymphoma, and multiple myeloma.</li> <li><strong>Treats Genetic Disorders:</strong> Can correct underlying genetic defects in blood cell production for conditions like aplastic anemia.</li> </ul>
Recovery Information
Recovery from stem cell transplant cancer treatment is a marathon, not a sprint. The acute hospital stay for conditioning and engraftment typically ranges from 3 to 6 weeks. During this period, the patient is highly susceptible to infections as their immune system rebuilds. Full immune recovery can take anywhere from 6 months to several years, especially after an allogeneic transplant. <p>Key aspects of <strong>stem cell transplant cancer recovery time and tips</strong> include:</p> <ul> <li><strong>Strict Infection Control:</strong> Meticulous hygiene, protective isolation, and avoiding crowds are crucial for months post-transplant.</li> <li><strong>Medication Adherence:</strong> Taking immunosuppressants (for allogeneic transplants), antibiotics, and other prescribed medications diligently.</li> <li><strong>Regular Follow-ups:</strong> Frequent blood tests and consultations with the transplant team to monitor engraftment, detect complications, and manage side effects.</li> <li><strong>Nutrition and Hydration:</strong> A balanced diet and adequate fluid intake are vital for recovery and energy.</li> <li><strong>Gentle Exercise:</strong> Gradually reintroducing physical activity under medical guidance to rebuild strength and stamina.</li> <li><strong>Psychological Support:</strong> Emotional counseling and support groups can help patients and families cope with the emotional and psychological challenges of recovery.</li> <li><strong>Return to Normal Activities:</strong> Gradual return to work, school, and social activities, often taking several months to a year or more, depending on individual progress and type of transplant.</li> </ul> <p>DivinHeal's dedicated care coordination extends through your recovery, providing guidance and support for a holistic healing journey.</p>

precision oncology
Treatment Price
$10500.00 USDPrecision oncology focuses on identifying specific biomarkers, genetic mutations, or protein expressions in a patient's tumor to select the most appropriate and effective therapies. This approach involves advanced diagnostic tools like genomic sequencing and comprehensive molecular profiling, leading to highly personalized treatment plans including targeted therapies, immunotherapies, and optimized conventional treatments.
Precision oncology focuses on identifying specific biomarkers, genetic mutations, or protein expressions in a patient's tumor to select the most appropriate and effective therapies. This approach involves advanced diagnostic tools like genomic sequencing and comprehensive molecular profiling, leading to highly personalized treatment plans including targeted therapies, immunotherapies, and optimized conventional treatments.
Treatment Overview
Precision oncology focuses on identifying specific biomarkers, genetic mutations, or protein expressions in a patient's tumor to select the most appropriate and effective therapies. This approach involves advanced diagnostic tools like genomic sequencing and comprehensive molecular profiling, leading to highly personalized treatment plans including targeted therapies, immunotherapies, and optimized conventional treatments.
Procedures
Precision oncology treatment typically begins with comprehensive molecular diagnostic testing of a tumor biopsy or liquid biopsy (blood sample). This involves advanced genomic sequencing (e.g., Next-Generation Sequencing or NGS) to identify specific genetic mutations, gene fusions, amplifications, or protein expressions (biomarkers) that are driving the cancer's growth. Based on these findings, a multidisciplinary team of oncologists, pathologists, and genetic counselors devises a personalized treatment plan. This plan may involve prescribing targeted therapy drugs (small molecule inhibitors or monoclonal antibodies) that specifically block the identified abnormal pathways, immunotherapies that harness the body's immune system to fight cancer, or selecting optimal conventional treatments like chemotherapy or radiation if specific markers indicate a higher likelihood of response. Treatment administration varies by drug type: oral medications are taken at home, while intravenous therapies are given in an outpatient clinic over several cycles. Throughout the treatment, patients are closely monitored for efficacy and side effects.
Benefits
<h2>Benefits of Precision Oncology Treatment</h2><ul><li><h3>Personalized & Targeted Care</h3><p>Treatments are specifically chosen based on your tumor's unique genetic profile, leading to highly individualized and effective therapy plans.</p></li><li><h3>Improved Efficacy & Outcomes</h3><p>By targeting specific cancer drivers, precision oncology often yields higher response rates and longer progression-free survival for eligible patients compared to conventional treatments.</p></li><li><h3>Reduced Side Effects</h3><p>Targeted therapies are designed to selectively attack cancer cells while sparing healthy cells, potentially leading to fewer and less severe side effects than broad-spectrum chemotherapy.</p></li><li><h3>Hope for Advanced & Refractory Cancers</h3><p>Precision oncology offers new treatment avenues for patients with advanced or metastatic cancers that may not respond to traditional therapies.</p></li><li><h3>Enhanced Quality of Life</h3><p>With more tolerable treatments and better disease control, patients often experience an improved quality of life during and after therapy.</p></li><li><h3>Access to Innovative Therapies</h3><p>DivinHeal provides access to the latest targeted drugs and immunotherapies, often unavailable or prohibitively expensive elsewhere.</p></li></ul>
Recovery Information
<h2>Recovery and Life After Precision Oncology Treatment</h2><p>Recovery from precision oncology treatment is highly individualized, depending on the specific therapies received, the stage of cancer, and the patient's overall health. While targeted therapies and immunotherapies generally have fewer systemic side effects than traditional chemotherapy, some patients may still experience fatigue, skin reactions, gastrointestinal issues, or immune-related adverse events.</p><h3>Expected Recovery Timeline</h3><ul><li><strong>Immediate Post-Treatment:</strong> Many targeted therapies are taken orally, allowing for treatment in outpatient settings. Initial recovery focuses on managing any acute side effects and monitoring treatment response.</li><li><strong>Short-term (Weeks to Months):</strong> Patients typically resume daily activities relatively quickly. Regular follow-up appointments, blood tests, and imaging scans are crucial to monitor treatment effectiveness and manage any lingering side effects.</li><li><strong>Long-term (Months to Years):</strong> Precision oncology often involves ongoing therapy for extended periods. Long-term recovery focuses on disease surveillance, managing potential long-term side effects, and focusing on overall wellness through diet, exercise, and mental health support.</li></ul><h3>Tips for a Smooth Recovery</h3><ul><li><strong>Adhere to Medication:</strong> Follow your prescribed drug regimen meticulously and report any new side effects to your medical team.</li><li><strong>Maintain a Healthy Lifestyle:</strong> A balanced diet, regular light exercise (as advised by your doctor), and adequate rest can significantly aid recovery.</li><li><strong>Psychological Support:</strong> Dealing with cancer and its treatment can be emotionally challenging. Seek counseling, join support groups, or connect with patient communities.</li><li><strong>Regular Follow-ups:</strong> Consistent monitoring with your oncologist is vital for adjusting treatment if needed and catching any recurrence early.</li><li><strong>DivinHeal’s Continued Support:</strong> Our care coordinators remain available for post-treatment queries, follow-up scheduling, and connecting you with wellness resources.</li></ul>

theranostics therapy
Treatment Price
$5000.00 USDOverview of Theranostics Therapy
Theranostics, a portmanteau of 'therapeutics' and 'diagnostics', represents a paradigm shift in personalized cancer treatment. Its primary goal is to precisely locate and destroy cancer cells by leveraging specific molecular targets on tumor surfaces. This dual approach ensures that therapy is only delivered to cells expressing the target, leading to higher efficacy and reduced side effects compared to conventional treatments. DivinHeal facilitates access to world-class theranostics therapy options, ensuring patients receive highly specialized and effective care.
Overview of Theranostics Therapy
Theranostics, a portmanteau of 'therapeutics' and 'diagnostics', represents a paradigm shift in personalized cancer treatment. Its primary goal is to precisely locate and destroy cancer cells by leveraging specific molecular targets on tumor surfaces. This dual approach ensures that therapy is only delivered to cells expressing the target, leading to higher efficacy and reduced side effects compared to conventional treatments. DivinHeal facilitates access to world-class theranostics therapy options, ensuring patients receive highly specialized and effective care.
Treatment Overview
<h2>Overview of Theranostics Therapy</h2><p>Theranostics, a portmanteau of 'therapeutics' and 'diagnostics', represents a paradigm shift in personalized cancer treatment. Its primary goal is to precisely locate and destroy cancer cells by leveraging specific molecular targets on tumor surfaces. This dual approach ensures that therapy is only delivered to cells expressing the target, leading to higher efficacy and reduced side effects compared to conventional treatments. DivinHeal facilitates access to world-class theranostics therapy options, ensuring patients receive highly specialized and effective care.</p>
Procedures
Theranostics therapy typically involves several steps, starting with diagnostic imaging. First, a diagnostic radiopharmaceutical (e.g., Gallium-68 PSMA or Gallium-68 DOTATATE) is administered intravenously. This tracer binds to specific receptors on cancer cells, and a PET/CT scan is performed to visualize the tumor's location and extent throughout the body. If the diagnostic scan confirms sufficient receptor expression, indicating the cancer cells can be targeted, the therapeutic phase begins. A therapeutic radiopharmaceutical (e.g., Lutetium-177 PSMA or Lutetium-177 DOTATATE) is then administered intravenously. This therapeutic agent, which binds to the same receptors, delivers targeted radiation (beta particles) directly to the cancer cells, causing their destruction while minimizing damage to surrounding healthy tissues. The therapy is often given in multiple cycles, typically 6-8 weeks apart, over several months. Each cycle involves an infusion that lasts from minutes to a few hours, followed by a short observation period.
Benefits
<h2>Benefits of Theranostics Therapy</h2><ul><li><h3>Highly Targeted Treatment</h3><p>Delivers radiation directly to cancer cells, minimizing damage to healthy tissues and reducing side effects.</p></li><li><h3>Improved Efficacy</h3><p>Demonstrates significant clinical benefits, including tumor regression, disease stabilization, and improved survival rates for specific advanced cancers.</p></li><li><h3>Personalized Approach</h3><p>Ensures that treatment is given only to patients whose tumors express the target, maximizing the chances of success.</p></li><li><h3>Enhanced Diagnosis</h3><p>Pre-therapy diagnostic imaging precisely stages the disease and identifies metastatic sites that may not be visible with conventional scans.</p></li><li><h3>Reduced Side Effects</h3><p>Compared to conventional chemotherapy or external beam radiation, systemic side effects are often milder and more manageable.</p></li><li><h3>Hope for Advanced Cases</h3><p>Offers a new lifeline for patients with advanced or metastatic cancers who have exhausted other treatment options.</p></li></ul>
Recovery Information
<h2>Theranostics Therapy Recovery Time and Tips</h2><p>The theranostics therapy recovery time is generally minimal compared to surgery or intensive chemotherapy. Most patients experience few or mild side effects, allowing for a relatively quick return to daily activities.</p><ul><li><h3>Immediate Post-Treatment</h3><p>Patients are monitored for a few hours post-infusion. Some mild nausea or fatigue may occur but usually subsides quickly. Radiation safety precautions will be provided, typically for a few days post-treatment.</p></li><li><h3>Short-Term Recovery (Days to Weeks)</h3><p>You may feel tired for a few days or weeks. Blood counts will be monitored, as there might be a temporary drop, particularly in white blood cells. Staying hydrated and getting adequate rest are crucial theranostics therapy recovery tips.</p></li><li><h3>Long-Term Wellness</h3><p>Regular follow-up appointments, including blood tests and imaging, are essential to monitor treatment response and manage any long-term effects. DivinHeal's care coordinators will assist in scheduling these and connecting you with support services, including nutritional guidance and emotional counseling, if needed. Adopting a healthy lifestyle and adhering to medical advice are key for sustained well-being.</p></li></ul>

chemoembolization
Treatment Price
$4500.00 USDChemoembolization aims to control tumor growth, alleviate symptoms, and potentially prolong survival for patients with inoperable liver cancers. Performed by interventional radiologists, it involves inserting a catheter into the femoral artery and guiding it to the hepatic artery supplying the tumor. Chemotherapeutic agents are then injected, followed by embolizing agents that block the blood flow, essentially starving the tumor of nutrients. DivinHeal connects you with top-tier hospitals offering advanced chemoembolization techniques for optimal outcomes.
Chemoembolization aims to control tumor growth, alleviate symptoms, and potentially prolong survival for patients with inoperable liver cancers. Performed by interventional radiologists, it involves inserting a catheter into the femoral artery and guiding it to the hepatic artery supplying the tumor. Chemotherapeutic agents are then injected, followed by embolizing agents that block the blood flow, essentially starving the tumor of nutrients. DivinHeal connects you with top-tier hospitals offering advanced chemoembolization techniques for optimal outcomes.
Treatment Overview
<p>Chemoembolization aims to control tumor growth, alleviate symptoms, and potentially prolong survival for patients with inoperable liver cancers. Performed by interventional radiologists, it involves inserting a catheter into the femoral artery and guiding it to the hepatic artery supplying the tumor. Chemotherapeutic agents are then injected, followed by embolizing agents that block the blood flow, essentially starving the tumor of nutrients. DivinHeal connects you with top-tier hospitals offering advanced chemoembolization techniques for optimal outcomes.</p>
Procedures
Chemoembolization (TACE) involves a precise, multi-step process. First, local anesthesia is administered at the groin, and a small incision is made to access the femoral artery. A thin catheter is then guided under fluoroscopic imaging through the arterial network to the specific hepatic artery supplying the liver tumor. An angiogram is performed to map the tumor's blood supply. Next, a mixture of chemotherapy drugs (e.g., Doxorubicin, Cisplatin) and an oily contrast agent (Lipiodol) is injected directly into the tumor. Following this, embolizing agents (e.g., gelatin sponge particles, microspheres) are introduced to block the feeding artery, effectively trapping the drugs and cutting off the tumor's blood supply. The catheter is then removed, and pressure is applied to the groin site.
Benefits
<p><h2>Key Benefits of Chemoembolization Treatment</h2><ul><li><h3>Highly Targeted Therapy</h3><p>Delivers high concentrations of chemotherapy drugs directly to the tumor, minimizing exposure and side effects on healthy tissues.</p></li><li><h3>Minimally Invasive Procedure</h3><p>Performed through a small incision, leading to less pain, shorter hospital stays, and quicker recovery compared to open surgery.</p></li><li><h3>Effective Tumor Control</h3><p>Combines drug delivery with blood supply blockage, significantly shrinking tumors and slowing disease progression for liver cancer management.</p></li><li><h3>Reduced Systemic Side Effects</h3><p>Localized drug delivery leads to fewer severe side effects commonly associated with traditional systemic chemotherapy.</p></li><li><h3>Improved Quality of Life</h3><p>By controlling tumor growth and alleviating symptoms, chemoembolization can significantly improve the patient's overall well-being and life expectancy.</p></li><li><h3>Bridging to Liver Transplant</h3><p>Can downstage tumors, making patients eligible for liver transplantation or serving as a crucial bridge therapy.</p></li></ul></p>
Recovery Information
<p><h2>Chemoembolization Recovery Time and Tips</h2><p>Recovery after chemoembolization typically involves a hospital stay of 1 to 3 days. Patients usually experience a phenomenon known as Post-Embolization Syndrome (PES), characterized by abdominal pain, nausea, vomiting, and fever. These symptoms are generally manageable with medication and usually subside within a few days to a week. DivinHeal provides comprehensive guidance and support throughout your recovery.</p><h3>Immediate Post-Procedure Care</h3><ul><li><strong>Hospital Stay:</strong> Close monitoring for any complications, pain management, and hydration.</li><li><strong>Rest:</strong> Essential in the first few days to allow your body to heal.</li><li><strong>Medication:</strong> Pain relievers, anti-nausea drugs, and potentially antibiotics will be prescribed to manage symptoms and prevent infection.</li></ul><h3>Returning Home: Recovery Tips for Chemoembolization</h3><ul><li><strong>Activity Restriction:</strong> Avoid strenuous activities, heavy lifting, and intense exercise for at least 1-2 weeks, or as advised by your doctor. Gradual return to normal activities is key.</li><li><strong>Hydration:</strong> Drink plenty of fluids to help your body recover and flush out toxins.</li><li><strong>Diet:</strong> Start with a light, bland diet and gradually return to your regular eating habits as tolerated.</li><li><strong>Follow-up:</strong> Regular follow-up appointments with your oncologist and interventional radiologist are crucial to monitor your recovery and assess the treatment's effectiveness. This typically includes imaging scans (CT/MRI) 4-6 weeks post-procedure.</li><li><strong>Emotional Support:</strong> It's normal to feel fatigued or emotionally drained. Seek support from family, friends, or counseling services. DivinHeal connects you with resources for holistic well-being.</li></ul><p>The full recovery for chemoembolization treatment can vary, but most patients feel significantly better within 2-4 weeks. Your medical team will provide personalized advice to ensure a smooth and effective recovery journey.</p></p>

radiofrequency ablation cancer
Treatment Price
$4500.00 USDOverview of Radiofrequency Ablation (RFA) Treatment Goals
Radiofrequency Ablation (RFA) aims to precisely destroy cancerous tumors with minimal invasion, offering an alternative or adjunct to surgery for suitable patients. The primary goals include tumor eradication, local disease control, pain relief, and improving quality of life. RFA utilizes image-guidance (ultrasound, CT, or MRI) to accurately place a specialized needle probe directly into the tumor. Radiofrequency energy then heats the tissue around the probe tip to temperatures lethal to cancer cells, coagulating and destroying them. This targeted approach minimizes impact on healthy tissue and typically allows for quicker recovery compared to open surgery.
Overview of Radiofrequency Ablation (RFA) Treatment Goals
Radiofrequency Ablation (RFA) aims to precisely destroy cancerous tumors with minimal invasion, offering an alternative or adjunct to surgery for suitable patients. The primary goals include tumor eradication, local disease control, pain relief, and improving quality of life. RFA utilizes image-guidance (ultrasound, CT, or MRI) to accurately place a specialized needle probe directly into the tumor. Radiofrequency energy then heats the tissue around the probe tip to temperatures lethal to cancer cells, coagulating and destroying them. This targeted approach minimizes impact on healthy tissue and typically allows for quicker recovery compared to open surgery.
Treatment Overview
<h3>Overview of Radiofrequency Ablation (RFA) Treatment Goals</h3><p>Radiofrequency Ablation (RFA) aims to precisely destroy cancerous tumors with minimal invasion, offering an alternative or adjunct to surgery for suitable patients. The primary goals include tumor eradication, local disease control, pain relief, and improving quality of life. RFA utilizes image-guidance (ultrasound, CT, or MRI) to accurately place a specialized needle probe directly into the tumor. Radiofrequency energy then heats the tissue around the probe tip to temperatures lethal to cancer cells, coagulating and destroying them. This targeted approach minimizes impact on healthy tissue and typically allows for quicker recovery compared to open surgery.</p>
Procedures
The Radiofrequency Ablation (RFA) procedure typically involves the following steps: Firstly, the patient is positioned, and local anesthesia, sedation, or general anesthesia is administered for comfort. Using real-time imaging guidance such as ultrasound, CT, or MRI, the interventional radiologist carefully inserts a thin, needle-like RFA electrode directly into the tumor. Once the tip of the electrode is precisely within the tumor, radiofrequency energy is delivered through it. This energy causes the ions in the surrounding tissue to vibrate, generating heat that raises the tissue temperature to 60-100°C. This high heat destroys the cancer cells through coagulative necrosis, while carefully controlled to minimize damage to nearby healthy tissue. The ablation process usually takes 10-30 minutes, depending on the tumor size. After the ablation is complete, the electrode is carefully withdrawn, and a small dressing is applied to the insertion site. The patient is then monitored for a few hours or overnight before discharge.
Benefits
<h3>Benefits of Radiofrequency Ablation (RFA) for Cancer</h3><ul><li><strong>Minimally Invasive:</strong> Requires only a small skin incision, resulting in less pain, reduced scarring, and faster recovery than traditional surgery.</li><li><strong>High Precision:</strong> Performed under real-time imaging guidance (CT, ultrasound), allowing for highly accurate targeting of tumors while preserving healthy surrounding tissue.</li><li><strong>Effective Tumor Destruction:</strong> Generates localized heat to effectively destroy cancer cells, often achieving complete ablation for suitable tumors.</li><li><strong>Reduced Hospital Stay:</strong> Often an outpatient procedure or requires only a short hospital stay (typically 1-2 days).</li><li><strong>Fewer Complications:</strong> Generally associated with a lower risk of complications compared to open surgical procedures.</li><li><strong>Repeatable Option:</strong> Can be safely repeated for new or recurrent tumors, providing ongoing local disease control.</li><li><strong>Alternative to Surgery:</strong> Excellent option for patients who are not surgical candidates due to age, co-morbidities, or tumor location.</li><li><strong>Improved Quality of Life:</strong> Contributes to local tumor control, symptom relief (e.g., pain from bone metastases), and potentially extended survival, enhancing overall patient well-being.</li></ul>
Recovery Information
<h3>Radiofrequency Ablation (RFA) Recovery Time and Tips</h3><p>Recovery after Radiofrequency Ablation (RFA) for cancer is generally quicker and less demanding compared to open surgical procedures, reflecting its minimally invasive nature. Most patients experience a smooth recovery, often returning to normal activities within a short period.</p><ul><li><strong>Immediate Post-Procedure:</strong> You will be monitored in the recovery area for a few hours to a day, depending on the site of ablation and your overall condition. Pain medication will be provided as needed to manage any discomfort at the ablation site.</li><li><strong>Hospital Stay:</strong> Many RFA procedures are performed on an outpatient basis. For more complex cases or specific organ ablations (e.g., liver), a hospital stay of 1-2 days might be recommended for observation.</li><li><strong>Pain Management:</strong> Mild to moderate pain or discomfort at the procedure site is common for a few days, managed with prescribed oral pain relievers.</li><li><strong>Activity Restrictions:</strong> You might be advised to limit strenuous activities, heavy lifting, and intense exercise for 1-2 weeks. Most patients can resume light activities within a few days.</li><li><strong>Follow-up:</strong> Your doctor will schedule follow-up appointments, including imaging scans (CT or MRI), typically within 1-3 months, to assess the success of the ablation and monitor for any recurrence.</li><li><strong>Recovery Tips:</strong><ul><li><strong>Rest:</strong> Allow your body sufficient rest, especially in the first few days post-procedure.</li><li><strong>Hydration:</strong> Drink plenty of fluids to aid recovery.</li><li><strong>Nutrition:</strong> Maintain a balanced, healthy diet.</li><li><strong>Monitor Symptoms:</strong> Report any persistent fever, severe pain, redness, or swelling at the incision site to your doctor immediately.</li><li><strong>Emotional Support:</strong> Engage with support groups or counseling if needed; DivinHeal can assist in connecting you with resources.</li></ul></li></ul><p>DivinHeal provides comprehensive post-procedure support, ensuring you have clear instructions and access to medical advice throughout your recovery journey, helping you return to optimal health as quickly and safely as possible.</p>

hipec surgery
Treatment Price
$8000.00 USDHIPEC surgery aims to significantly improve survival rates and quality of life for patients battling peritoneal carcinomatosis, a condition where cancer has spread to the lining of the abdominal cavity. The treatment involves a meticulously performed cytoreductive surgery to remove all macroscopic tumor implants, followed by the direct delivery of heated chemotherapy drugs to eradicate any remaining microscopic cancer cells. This maximizes drug concentration in the abdomen while minimizing systemic side effects.
HIPEC surgery aims to significantly improve survival rates and quality of life for patients battling peritoneal carcinomatosis, a condition where cancer has spread to the lining of the abdominal cavity. The treatment involves a meticulously performed cytoreductive surgery to remove all macroscopic tumor implants, followed by the direct delivery of heated chemotherapy drugs to eradicate any remaining microscopic cancer cells. This maximizes drug concentration in the abdomen while minimizing systemic side effects.
Treatment Overview
HIPEC surgery aims to significantly improve survival rates and quality of life for patients battling peritoneal carcinomatosis, a condition where cancer has spread to the lining of the abdominal cavity. The treatment involves a meticulously performed cytoreductive surgery to remove all macroscopic tumor implants, followed by the direct delivery of heated chemotherapy drugs to eradicate any remaining microscopic cancer cells. This maximizes drug concentration in the abdomen while minimizing systemic side effects.
Procedures
HIPEC surgery involves two main phases: first, Cytoreductive Surgery (CRS), where the surgeon removes all visible cancerous tumors from the abdominal cavity. This may include removing affected organs or parts of organs (e.g., parts of the colon, spleen, gallbladder, ovaries). The goal is to leave no visible cancer behind. Second, once all visible tumors are removed, a heated chemotherapy solution is continuously circulated through the abdominal cavity for a specific duration (typically 60-120 minutes) using specialized equipment. The chemotherapy is heated to a temperature around 41-42°C, which helps it penetrate deeper into tissues and enhances its cancer-killing effect. After the chemotherapy infusion, the solution is drained, and the abdominal incision is closed. The entire procedure can take anywhere from 6 to 12 hours or even longer, depending on the extent of cancer.
Benefits
<h2>Benefits of HIPEC Surgery</h2><ul><li><h3>Enhanced Chemotherapy Delivery</h3><p>Direct application of chemotherapy to the abdominal cavity ensures higher concentration at the tumor site, improving drug efficacy against peritoneal cancer cells while minimizing systemic side effects.</p></li><li><h3>Improved Survival Rates</h3><p>For carefully selected patients with peritoneal carcinomatosis, HIPEC surgery has demonstrated significantly improved overall survival and disease-free survival rates compared to traditional treatments alone.</p></li><li><h3>Targeted Treatment for Microscopic Disease</h3><p>The heated chemotherapy effectively targets and eliminates microscopic cancer cells that may remain after visible tumors are removed, reducing the risk of recurrence.</p></li><li><h3>Reduced Systemic Toxicity</h3><p>By confining chemotherapy to the abdomen, the treatment reduces exposure of vital organs to high-dose chemotherapy, leading to fewer severe side effects commonly associated with intravenous chemotherapy.</p></li><li><h3>Hope for Advanced Cancers</h3><p>HIPEC offers a crucial treatment option for patients with advanced abdominal cancers previously considered untreatable, providing a renewed sense of hope and significantly improving their prognosis.</p></li></ul>
Recovery Information
<h2>HIPEC Surgery Recovery Time and Tips</h2><h3>Immediate Post-Operative Care</h3><p>Recovery from HIPEC surgery is an intensive process, typically requiring a hospital stay of 10-14 days, though this can vary. Patients will be monitored closely in the intensive care unit (ICU) initially for pain management, fluid balance, and vital organ function. Early mobilization and respiratory exercises are crucial to prevent complications.</p><h3>Long-Term Recovery and Rehabilitation</h3><p>Full recovery can take several weeks to months (3-6 months), involving a gradual return to normal activities. Patients may experience fatigue, changes in bowel habits, and require nutritional support. Physical therapy, dietary counseling, and emotional support are vital components of the recovery process. DivinHeal provides comprehensive guidance for HIPEC surgery recovery, connecting patients with rehabilitation specialists and support groups to ensure optimal healing and quality of life post-treatment.</p><h3>Important Recovery Tips:</h3><ul><li>Follow all post-operative instructions meticulously.</li><li>Engage in gentle, progressive physical activity as advised by your medical team.</li><li>Maintain a healthy, balanced diet to aid healing.</li><li>Attend all follow-up appointments and screenings.</li><li>Seek psychological and emotional support to cope with the challenges of recovery.</li></ul>

cyberknife treatment
Treatment Price
$5000.00 USDCyberKnife Treatment: Precision Radiation Therapy
CyberKnife treatment is a cutting-edge, non-surgical robotic radiosurgery system designed to treat cancerous and non-cancerous tumors throughout the body with unparalleled precision. Its primary goal is to deliver high doses of radiation directly to the target area while sparing surrounding healthy tissue, thereby reducing side effects and improving patient outcomes. The system uses real-time image guidance and a robotic arm to track tumor movement, ensuring extreme accuracy even as the patient breathes or moves slightly.
Techniques and Goals
- Stereotactic Radiosurgery (SRS): For tumors in the brain and spine, typically delivered in 1-5 sessions.
- Stereotactic Body Radiation Therapy (SBRT): For tumors in the lung, prostate, liver, kidney, pancreas, and other areas, also typically in 1-5 sessions.
- High Precision: The CyberKnife's robotic arm can reach hundreds of angles, allowing for highly conformal radiation delivery that matches the exact shape of the tumor.
- Real-time Tracking: It continuously monitors the tumor's position and patient's breathing, adjusting radiation beams dynamically.
- Non-Invasive: Eliminates the need for incisions, reducing risks associated with traditional surgery.
- Pain-Free & Outpatient: Most treatments are performed on an outpatient basis, allowing patients to return to their normal activities quickly.
CyberKnife Treatment: Precision Radiation Therapy
CyberKnife treatment is a cutting-edge, non-surgical robotic radiosurgery system designed to treat cancerous and non-cancerous tumors throughout the body with unparalleled precision. Its primary goal is to deliver high doses of radiation directly to the target area while sparing surrounding healthy tissue, thereby reducing side effects and improving patient outcomes. The system uses real-time image guidance and a robotic arm to track tumor movement, ensuring extreme accuracy even as the patient breathes or moves slightly.
Techniques and Goals
- Stereotactic Radiosurgery (SRS): For tumors in the brain and spine, typically delivered in 1-5 sessions.
- Stereotactic Body Radiation Therapy (SBRT): For tumors in the lung, prostate, liver, kidney, pancreas, and other areas, also typically in 1-5 sessions.
- High Precision: The CyberKnife's robotic arm can reach hundreds of angles, allowing for highly conformal radiation delivery that matches the exact shape of the tumor.
- Real-time Tracking: It continuously monitors the tumor's position and patient's breathing, adjusting radiation beams dynamically.
- Non-Invasive: Eliminates the need for incisions, reducing risks associated with traditional surgery.
- Pain-Free & Outpatient: Most treatments are performed on an outpatient basis, allowing patients to return to their normal activities quickly.
Treatment Overview
<h2>CyberKnife Treatment: Precision Radiation Therapy</h2><p>CyberKnife treatment is a cutting-edge, non-surgical robotic radiosurgery system designed to treat cancerous and non-cancerous tumors throughout the body with unparalleled precision. Its primary goal is to deliver high doses of radiation directly to the target area while sparing surrounding healthy tissue, thereby reducing side effects and improving patient outcomes. The system uses real-time image guidance and a robotic arm to track tumor movement, ensuring extreme accuracy even as the patient breathes or moves slightly.</p><h3>Techniques and Goals</h3><ul><li><strong>Stereotactic Radiosurgery (SRS):</strong> For tumors in the brain and spine, typically delivered in 1-5 sessions.</li><li><strong>Stereotactic Body Radiation Therapy (SBRT):</strong> For tumors in the lung, prostate, liver, kidney, pancreas, and other areas, also typically in 1-5 sessions.</li><li><strong>High Precision:</strong> The CyberKnife's robotic arm can reach hundreds of angles, allowing for highly conformal radiation delivery that matches the exact shape of the tumor.</li><li><strong>Real-time Tracking:</strong> It continuously monitors the tumor's position and patient's breathing, adjusting radiation beams dynamically.</li><li><strong>Non-Invasive:</strong> Eliminates the need for incisions, reducing risks associated with traditional surgery.</li><li><strong>Pain-Free & Outpatient:</strong> Most treatments are performed on an outpatient basis, allowing patients to return to their normal activities quickly.</li></ul>
Procedures
The CyberKnife treatment procedure is a multi-step process designed for maximum precision and patient comfort. It typically begins with a detailed planning phase: high-resolution imaging (CT, MRI, PET) is used to create a 3D model of the tumor and surrounding anatomy. Tiny gold markers (fiducials) may be implanted near the tumor for real-time tracking, especially for tumors that move with respiration. A custom immobilization device (e.g., a body mold or head frame) is then created to ensure the patient remains still during treatment. During the actual treatment, the patient lies comfortably on a robotic couch. The CyberKnife's robotic arm delivers precise radiation beams from hundreds of angles around the patient, targeting the tumor while avoiding healthy tissue. Throughout the session, the system continuously monitors the tumor's position using X-ray cameras and adjusts the robotic arm in real-time to compensate for any patient movement or respiratory motion. This dynamic tracking ensures that the radiation always hits the target with sub-millimeter accuracy. Each session lasts 30-90 minutes, and treatment is usually completed in 1-5 outpatient sessions over several days.
Benefits
<h2>Key Benefits of CyberKnife Treatment</h2><p>CyberKnife offers numerous advantages, making it a preferred choice for many patients seeking effective, non-invasive cancer treatment.</p><ul><li><strong>Exceptional Precision:</strong> Sub-millimeter accuracy minimizes radiation exposure to healthy tissues, reducing side effects.</li><li><strong>Non-Invasive:</strong> No incisions, no anesthesia, no hospital stay, and typically no pain during the procedure.</li><li><strong>Shorter Treatment Course:</strong> Often completed in 1-5 sessions, significantly fewer than conventional radiation therapy (20-40 sessions).</li><li><strong>Real-time Tracking:</strong> The system adapts to tumor movement caused by breathing or slight patient shifts, ensuring consistent accuracy.</li><li><strong>Treats Inoperable Tumors:</strong> Can effectively treat tumors located in challenging or sensitive areas that are difficult or impossible to treat surgically.</li><li><strong>Outpatient Procedure:</strong> Patients can typically return home immediately after each treatment session, resuming normal activities sooner.</li><li><strong>Reduced Side Effects:</strong> By sparing healthy tissue, CyberKnife often leads to fewer and less severe side effects compared to traditional radiation or surgery.</li><li><strong>High Success Rates:</strong> Demonstrated high local control rates for various cancers, often comparable to surgical outcomes.</li><li><strong>Improved Quality of Life:</strong> Minimal disruption to daily life during and after treatment, supporting a faster return to well-being.</li></ul>
Recovery Information
<h2>CyberKnife Treatment Recovery Time and Tips</h2><p>One of the significant advantages of CyberKnife treatment is its minimal impact on a patient's daily life, leading to a generally swift and manageable recovery.</p><h3>Immediate Post-Treatment</h3><ul><li><strong>Outpatient Procedure:</strong> Most patients return home immediately after each CyberKnife session.</li><li><strong>Minimal Side Effects:</strong> Many patients experience no immediate side effects. Some might report mild fatigue, slight headache (especially for brain treatments), or minor nausea, which are typically temporary and manageable with medication.</li><li><strong>Resume Daily Activities:</strong> Most individuals can resume light daily activities, including work, shortly after treatment. Strenuous exercise might be advised against for a short period.</li></ul><h3>Short-Term Recovery (Days to Weeks)</h3><ul><li><strong>Fatigue:</strong> This is the most commonly reported side effect, which can persist for a few days to a few weeks after the final session. Ensure adequate rest.</li><li><strong>Skin Changes:</strong> While rare, some patients might experience mild skin redness or irritation at the treatment site.</li><li><strong>Localized Symptoms:</strong> Depending on the treated area, some localized swelling or discomfort might occur, which usually resolves quickly.</li><li><strong>Follow-up Appointments:</strong> Regular check-ups with your oncologist are crucial to monitor your response to treatment and manage any emerging side effects.</li></ul><h3>Long-Term Wellness and Tips</h3><ul><li><strong>Hydration:</strong> Drink plenty of fluids to help your body recover.</li><li><strong>Nutrition:</strong> Maintain a balanced, healthy diet. Consult with a nutritionist if needed.</li><li><strong>Gentle Exercise:</strong> Light walking and stretching can aid recovery and boost energy levels.</li><li><strong>Listen to Your Body:</strong> Rest when you feel tired and gradually increase activity levels.</li><li><strong>Emotional Support:</strong> Seek support from family, friends, or counseling services. DivinHeal can connect you with mental health professionals to navigate the emotional aspects of cancer recovery.</li><li><strong>Avoid Irritants:</strong> Depending on the treatment area, avoid alcohol, smoking, or certain foods that might exacerbate symptoms.</li><li><strong>Long-term Monitoring:</strong> Ongoing imaging scans (MRI, CT) will be scheduled to monitor tumor response and ensure long-term control.</li></ul><p>DivinHeal's dedicated care coordinators will provide detailed recovery instructions and support throughout your post-treatment journey, ensuring a smooth and hopeful path to full recovery.</p>

gamma knife surgery
Treatment Price
$5500.00 USDOverview of Gamma Knife Surgery
Gamma Knife surgery is an advanced, non-invasive radiosurgical technique primarily used to treat brain and head conditions. Its main goal is to deliver a high dose of radiation precisely to a targeted area while minimizing exposure to surrounding healthy brain tissue. This highly focused approach allows for treatment of complex conditions, often in a single session, reducing risks associated with traditional open surgery and offering hope for patients seeking less invasive options. DivinHeal connects you to world-class facilities offering state-of-the-art gamma knife surgery, ensuring safety and optimal outcomes.
Overview of Gamma Knife Surgery
Gamma Knife surgery is an advanced, non-invasive radiosurgical technique primarily used to treat brain and head conditions. Its main goal is to deliver a high dose of radiation precisely to a targeted area while minimizing exposure to surrounding healthy brain tissue. This highly focused approach allows for treatment of complex conditions, often in a single session, reducing risks associated with traditional open surgery and offering hope for patients seeking less invasive options. DivinHeal connects you to world-class facilities offering state-of-the-art gamma knife surgery, ensuring safety and optimal outcomes.
Treatment Overview
<h2>Overview of Gamma Knife Surgery</h2><p>Gamma Knife surgery is an advanced, non-invasive radiosurgical technique primarily used to treat brain and head conditions. Its main goal is to deliver a high dose of radiation precisely to a targeted area while minimizing exposure to surrounding healthy brain tissue. This highly focused approach allows for treatment of complex conditions, often in a single session, reducing risks associated with traditional open surgery and offering hope for patients seeking less invasive options. DivinHeal connects you to world-class facilities offering state-of-the-art gamma knife surgery, ensuring safety and optimal outcomes.</p>
Procedures
Gamma Knife surgery is performed in a series of precise steps. First, a lightweight stereotactic head frame is temporarily affixed to the patient's head to ensure complete immobility and pinpoint accuracy. High-resolution imaging, such as MRI or CT scans, is then performed with the frame in place to precisely map the target lesion. A specialized team, including a neurosurgeon, radiation oncologist, and medical physicist, collaborates to create a personalized treatment plan, determining the exact radiation dose and beam configuration. During the treatment, the patient lies on a couch that slides into the Gamma Knife unit, and the radiation is delivered from multiple cobalt-60 sources to the pre-determined target. The patient feels no pain during the procedure. After the treatment, the head frame is removed, and the patient can typically go home the same day.
Benefits
<h2>Benefits of Gamma Knife Surgery</h2><p>Gamma Knife surgery offers numerous advantages, making it a preferred option for many neurological conditions:</p><ul><li><h3>Minimally Invasive:</h3><p>No surgical incision means reduced risk of complications like infection, hemorrhage, and general anesthesia risks.</p></li><li><h3>High Precision:</h3><p>Targets lesions with sub-millimeter accuracy, preserving surrounding healthy brain tissue and critical structures.</p></li><li><h3>Fast Recovery:</h3><p>Patients typically experience a quicker gamma knife surgery recovery time and can return to their normal activities within a few days.</p></li><li><h3>Outpatient Procedure:</h3><p>Often performed as an outpatient procedure, eliminating the need for extended hospital stays.</p></li><li><h3>Effective Treatment:</h3><p>Demonstrates high gamma knife surgery success rate for various conditions, including tumors and vascular malformations.</p></li><li><h3>Reduced Pain & Discomfort:</h3><p>Generally associated with less pain and discomfort compared to traditional open brain surgery.</p></li></ul>
Recovery Information
<h2>Gamma Knife Surgery Recovery Time and Tips</h2><p>One of the significant advantages of gamma knife surgery is its relatively quick recovery period compared to conventional surgery. Most patients can expect to return to their normal routine within a few days. However, the exact gamma knife surgery recovery time can vary based on the treated condition, its size, and the patient's overall health.</p><h3>Immediate Post-Procedure:</h3><ul><li>You may experience a mild headache or nausea immediately after the procedure, which can be managed with medication.</li><li>Some patients report slight discomfort or swelling where the head frame was attached, which typically resolves quickly.</li><li>You'll usually be discharged on the same day or after an overnight observation.</li></ul><h3>Short-Term Recovery (First Few Days to Weeks):</h3><ul><li>Rest is important, but light activities can generally be resumed.</li><li>Avoid strenuous physical activity for a week or two, as advised by your doctor.</li><li>Follow any specific dietary or medication instructions.</li></ul><h3>Long-Term Recovery & Follow-up:</h3><ul><li>The full effects of gamma knife surgery often become apparent over weeks to months as the treated lesion gradually shrinks or becomes inactive.</li><li>Regular follow-up MRI scans will be scheduled by your neuro-oncologist to monitor progress.</li><li>DivinHeal's comprehensive support extends to post-treatment follow-up, helping you navigate your gamma knife surgery recovery and ensuring continued care.</li></ul>

brachytherapy
Treatment Price
$4500.00 USDBrachytherapy: Precision Internal Radiation for Cancer Treatment
Brachytherapy, also known as internal radiation therapy, involves placing radioactive sources directly inside or very close to the tumor. This allows for a very high dose of radiation to be delivered to the cancer cells with minimal impact on surrounding healthy tissue. It's a highly precise and effective treatment often used for cancers of the prostate, cervix, breast, skin, and head & neck, emphasizing hope and a path to recovery.
Why Choose Brachytherapy for Quality Care?
- Targeted Treatment: Delivers radiation directly to the tumor, maximizing effectiveness while sparing healthy organs.
- Minimized Side Effects: Reduces radiation exposure to nearby healthy organs, leading to a better quality of life during and after treatment.
- Shorter Treatment Times: Often requires fewer treatment sessions compared to external beam radiation, offering convenience and efficiency.
- High Success Rates: Proven efficacy and excellent local control rates in various cancer types, offering peace of mind.
Brachytherapy: Precision Internal Radiation for Cancer Treatment
Brachytherapy, also known as internal radiation therapy, involves placing radioactive sources directly inside or very close to the tumor. This allows for a very high dose of radiation to be delivered to the cancer cells with minimal impact on surrounding healthy tissue. It's a highly precise and effective treatment often used for cancers of the prostate, cervix, breast, skin, and head & neck, emphasizing hope and a path to recovery.
Why Choose Brachytherapy for Quality Care?
- Targeted Treatment: Delivers radiation directly to the tumor, maximizing effectiveness while sparing healthy organs.
- Minimized Side Effects: Reduces radiation exposure to nearby healthy organs, leading to a better quality of life during and after treatment.
- Shorter Treatment Times: Often requires fewer treatment sessions compared to external beam radiation, offering convenience and efficiency.
- High Success Rates: Proven efficacy and excellent local control rates in various cancer types, offering peace of mind.
Treatment Overview
<h2>Brachytherapy: Precision Internal Radiation for Cancer Treatment</h2><p>Brachytherapy, also known as internal radiation therapy, involves placing radioactive sources directly inside or very close to the tumor. This allows for a very high dose of radiation to be delivered to the cancer cells with minimal impact on surrounding healthy tissue. It's a highly precise and effective treatment often used for cancers of the prostate, cervix, breast, skin, and head & neck, emphasizing hope and a path to recovery.</p><h3>Why Choose Brachytherapy for Quality Care?</h3><ul><li><strong>Targeted Treatment:</strong> Delivers radiation directly to the tumor, maximizing effectiveness while sparing healthy organs.</li><li><strong>Minimized Side Effects:</strong> Reduces radiation exposure to nearby healthy organs, leading to a better quality of life during and after treatment.</li><li><strong>Shorter Treatment Times:</strong> Often requires fewer treatment sessions compared to external beam radiation, offering convenience and efficiency.</li><li><strong>High Success Rates:</strong> Proven efficacy and excellent local control rates in various cancer types, offering peace of mind.</li></ul>
Procedures
Brachytherapy involves several key steps, executed with precision and care to ensure optimal outcomes: 1. **Consultation and Planning:** After diagnosis, a detailed evaluation is conducted, often including advanced imaging (CT, MRI, ultrasound) to precisely map the tumor and surrounding healthy tissues. A multidisciplinary team, including a radiation oncologist, medical physicist, and dosimetrist, develops a personalized treatment plan. This plan determines the specific type of brachytherapy (LDR or HDR), the radioactive source to be used, its exact placement, and the precise dosage required. 2. **Applicator Placement:** Depending on the cancer site (e.g., prostate, cervix, breast), a specialized applicator (such as needles, catheters, balloons, or cylinders) is meticulously inserted into the tumor or adjacent to it. This step may require local, regional, or general anesthesia to ensure patient comfort and safety. 3. **Image Guidance:** Real-time imaging techniques (e.g., ultrasound, fluoroscopy, CT scans) are used during the procedure to confirm the accurate placement of the applicator and to fine-tune the treatment plan, ensuring optimal and safe dose distribution. 4. **Radioactive Source Delivery:** * **HDR Brachytherapy:** A computer-controlled machine, known as an afterloader, delivers a high-dose radioactive source (most commonly Iridium-192) through the applicator tubes for a precise, short duration (typically minutes). The source is then safely retracted. This process is repeated over several scheduled sessions. * **LDR Brachytherapy:** Tiny radioactive seeds (e.g., Iodine-125, Palladium-103) are permanently implanted directly into the tumor through thin needles. These seeds remain in place and gradually release radiation over weeks to months, after which their radioactivity decays to negligible levels. 5. **Post-Procedure Care:** After HDR sessions, the applicator is removed. For LDR, the seeds remain embedded. Patients are carefully monitored for any immediate side effects and are provided with comprehensive instructions for post-treatment care and follow-up appointments.
Benefits
<h2>Key Benefits of Brachytherapy Treatment: Hope for a Healthier Tomorrow</h2><h3>Why Brachytherapy is a Preferred Option for Precision Cancer Care</h3><ul><li><strong>Highly Targeted Radiation Delivery:</strong> The primary advantage is the ability to deliver a very high dose of radiation directly to the tumor, precisely minimizing damage to surrounding healthy tissues and organs. This precision contributes to fewer and milder side effects, enhancing patient safety.</li><li><strong>Reduced Treatment Time:</strong> Often, brachytherapy requires fewer treatment sessions or a shorter overall treatment course compared to external beam radiation therapy. This can significantly reduce the inconvenience and duration of treatment, getting you back to life sooner.</li><li><strong>High Local Control Rates:</strong> For many cancers, brachytherapy offers excellent local tumor control rates, meaning the cancer is effectively eliminated or kept from growing in the treated area. This translates to higher success rates and greater hope for long-term remission.</li><li><strong>Effective for Various Cancers:</strong> Proven efficacy in treating a wide range of localized cancers, including prostate, cervical, breast, skin, and head & neck cancers, offering a versatile treatment solution.</li><li><strong>Versatility:</strong> Can be used alone, or effectively combined with surgery, external beam radiation, chemotherapy, or hormonal therapy to enhance overall treatment outcomes and achieve comprehensive cancer control.</li><li><strong>Improved Quality of Life:</strong> By preserving healthy tissue and reducing systemic side effects, brachytherapy can lead to a better quality of life during and after treatment, with fewer long-term complications, fostering a sense of hope and well-being.</li></ul>
Recovery Information
<h2>Brachytherapy Recovery Time and Tips for Optimal Healing</h2><h3>What to Expect After Brachytherapy Treatment</h3><p>Recovery from brachytherapy largely depends on the type of brachytherapy (LDR or HDR), the treated area, and whether it was combined with other treatments. Generally, brachytherapy is well-tolerated, and recovery is often quicker than with more invasive procedures, offering a smooth path to recovery.</p><h3>Immediate Post-Procedure: Focusing on Safety and Comfort</h3><ul><li><strong>HDR Brachytherapy:</strong> For temporary implants (HDR), the applicator is removed after each session. Patients typically experience minimal discomfort and can often return to normal activities fairly quickly. Some localized soreness or swelling may occur, which is usually manageable.</li><li><strong>LDR Brachytherapy:</strong> For permanent implants (LDR seeds), patients might experience some localized pain, swelling, or bruising at the implant site for a few days to weeks. Your doctor will provide effective pain management strategies.</li><li><strong>Common Side Effects:</strong> Fatigue is common, as is localized discomfort, swelling, or tenderness in the treated area. Depending on the treated site, you might experience temporary urinary changes (e.g., prostate/cervical brachytherapy), bowel changes (e.g., prostate/cervical/rectal brachytherapy), or skin irritation (e.g., skin/breast brachytherapy).</li></ul><h3>Brachytherapy Recovery Timeline: A Gradual Return to Wellness</h3><ul><li><strong>Short-Term (Days to Weeks):</strong> Most patients can resume light daily activities within a few days. Significant recovery from immediate discomfort typically resolves within 1-3 weeks.</li><li><strong>Long-Term (Weeks to Months):</strong> Some subtle side effects like persistent fatigue or minor urinary/bowel changes can linger for several weeks or months, gradually improving over time. Your medical team will monitor these closely, ensuring your long-term well-being.</li></ul><h3>Brachytherapy Recovery Tips for a Smooth Journey</h3><ul><li><strong>Follow Medical Advice:</strong> Adhere strictly to your oncologist's post-treatment instructions, including medication regimens, activity restrictions, and any specific wound care, prioritizing your safety.</li><li><strong>Rest Adequately:</strong> Allow your body sufficient rest to heal and recover from treatment-related fatigue.</li><li><strong>Hydration and Nutrition:</strong> Maintain a healthy, balanced diet and stay well-hydrated to support your body's healing processes.</li><li><strong>Gentle Activity:</strong> Gradually reintroduce physical activity as tolerated, avoiding strenuous exercise initially to prevent complications.</li><li><strong>Manage Side Effects:</strong> Discuss any persistent or worsening side effects with your medical team. Medications or lifestyle adjustments can often help alleviate symptoms effectively.</li><li><strong>Emotional Support:</strong> Seek support from family, friends, or professional counselors to cope with the emotional aspects of cancer treatment and recovery, fostering hope.</li><li><strong>Regular Follow-ups:</strong> Attend all scheduled follow-up appointments to monitor your recovery, assess treatment effectiveness, and detect any potential recurrences early. DivinHeal assists with coordinating these vital appointments.</li></ul>

imrt radiation therapy
Treatment Price
$4000.00 USDIMRT radiation therapy revolutionizes cancer treatment by precisely shaping and modulating radiation beams to conform to the exact contours of a tumor. The primary goal is to maximize the radiation dose delivered to cancer cells, thereby increasing the chance of tumor control or eradication, while meticulously sparing vital organs and healthy tissues. This leads to improved patient outcomes and a better quality of life during and after treatment. DivinHeal connects you with top-tier hospitals offering this cutting-edge technology.
IMRT radiation therapy revolutionizes cancer treatment by precisely shaping and modulating radiation beams to conform to the exact contours of a tumor. The primary goal is to maximize the radiation dose delivered to cancer cells, thereby increasing the chance of tumor control or eradication, while meticulously sparing vital organs and healthy tissues. This leads to improved patient outcomes and a better quality of life during and after treatment. DivinHeal connects you with top-tier hospitals offering this cutting-edge technology.
Treatment Overview
IMRT radiation therapy revolutionizes cancer treatment by precisely shaping and modulating radiation beams to conform to the exact contours of a tumor. The primary goal is to maximize the radiation dose delivered to cancer cells, thereby increasing the chance of tumor control or eradication, while meticulously sparing vital organs and healthy tissues. This leads to improved patient outcomes and a better quality of life during and after treatment. DivinHeal connects you with top-tier hospitals offering this cutting-edge technology.
Procedures
IMRT radiation therapy involves several precise steps: (1) **Consultation and Diagnosis:** Comprehensive review of medical history, imaging, and pathology. (2) **Treatment Planning (Simulation):** A CT scan, often combined with MRI or PET, is performed with the patient in a comfortable, immobilized position to map the exact tumor location and critical organs. (3) **Contouring:** A radiation oncologist precisely outlines the tumor volume and healthy organs on the simulation images. (4) **Dosimetry and Inverse Planning:** Medical physicists and dosimetrists use specialized software to design a treatment plan, determining the optimal radiation beam angles, shapes, and intensities to deliver a high dose to the tumor while sparing normal tissues. (5) **Quality Assurance:** The treatment plan undergoes rigorous checks to ensure accuracy and safety. (6) **Daily Treatment Delivery:** Patients lie on a treatment couch, in the same position as during simulation. A linear accelerator delivers the radiation, typically in short, painless sessions (15-30 minutes) daily, five days a week, over several weeks. Image-Guided Radiation Therapy (IGRT) is often used daily to ensure precise targeting before each treatment. (7) **Monitoring and Follow-up:** Regular check-ups with the care team during and after treatment to manage side effects and monitor response.
Benefits
IMRT radiation therapy offers significant benefits for cancer patients seeking effective and precise treatment:<ul><li><strong>Superior Tumor Targeting:</strong> Delivers highly conformal radiation doses, precisely matching the tumor's shape and location.</li><li><strong>Reduced Side Effects:</strong> By sparing healthy tissues and critical organs, IMRT minimizes common radiation side effects such as skin irritation, fatigue, or organ damage, improving overall patient comfort.</li><li><strong>Higher Dose Delivery:</strong> Allows for the safe delivery of higher, more potent radiation doses to the tumor, potentially increasing treatment efficacy and tumor control rates.</li><li><strong>Improved Quality of Life:</strong> Less severe side effects mean patients can maintain a better quality of life during and after their treatment course.</li><li><strong>Versatility:</strong> Effective for a wide range of cancers, including those in sensitive or complex anatomical locations.</li><li><strong>Personalized Treatment:</strong> Each IMRT plan is uniquely tailored to the individual patient's anatomy and tumor characteristics.</li></ul>
Recovery Information
Recovery from IMRT radiation therapy is generally managed on an outpatient basis. Patients can usually continue with most daily activities throughout their treatment course. However, side effects, which vary depending on the treated area, may develop and intensify towards the middle or end of the treatment, gradually subsiding in the weeks following completion. Common recovery aspects include:<ul><li><strong>Fatigue:</strong> A common side effect, which can be managed with rest and light activity.</li><li><strong>Skin Reactions:</strong> Mild redness, dryness, or itching in the treated area. Skin care instructions will be provided.</li><li><strong>Site-Specific Side Effects:</strong> For head and neck treatments, temporary swallowing difficulties or dry mouth; for pelvic treatments, bladder or bowel changes. These are typically less severe than with conventional radiation.</li><li><strong>Emotional Support:</strong> It's important to seek emotional support as needed, as cancer treatment can be taxing.</li></ul><p>DivinHeal provides comprehensive post-treatment support, including access to nutritionists, physical therapists, and counselors, to ensure a smooth and holistic recovery journey. Regular follow-up appointments with your oncologist are crucial to monitor progress and address any long-term concerns.</p>

chemotherapy for cancer
Treatment Price
$3000.00 USDChemotherapy Treatment Overview
Chemotherapy is a vital medical therapy designed to combat cancer by utilizing potent chemicals that target and eliminate rapidly dividing cells, characteristic of cancerous growths. This systemic approach can be employed as a primary treatment, neoadjuvant (before surgery), adjuvant (after surgery), or palliative care to manage symptoms. DivinHeal connects you with world-class oncology centers offering advanced chemotherapy protocols, ensuring personalized and effective care.
Chemotherapy Treatment Overview
Chemotherapy is a vital medical therapy designed to combat cancer by utilizing potent chemicals that target and eliminate rapidly dividing cells, characteristic of cancerous growths. This systemic approach can be employed as a primary treatment, neoadjuvant (before surgery), adjuvant (after surgery), or palliative care to manage symptoms. DivinHeal connects you with world-class oncology centers offering advanced chemotherapy protocols, ensuring personalized and effective care.
Treatment Overview
<h2>Chemotherapy Treatment Overview</h2><p>Chemotherapy is a vital medical therapy designed to combat cancer by utilizing potent chemicals that target and eliminate rapidly dividing cells, characteristic of cancerous growths. This systemic approach can be employed as a primary treatment, neoadjuvant (before surgery), adjuvant (after surgery), or palliative care to manage symptoms. DivinHeal connects you with world-class oncology centers offering advanced chemotherapy protocols, ensuring personalized and effective care.</p>
Procedures
Chemotherapy administration typically involves several steps: 1. **Preparation**: Before each cycle, blood tests are performed to ensure the patient's body can safely receive treatment. Medications to prevent nausea or allergic reactions may be given. 2. **Drug Mixing**: Chemotherapy drugs are precisely mixed by pharmacists, often in a sterile environment, tailored to the patient's specific protocol and body surface area. 3. **Administration**: Most commonly, chemotherapy is given intravenously (IV) through a vein in the arm, hand, or via a central line (PICC line, port-a-cath) for longer courses. Oral chemotherapy is also available for some cancers. 4. **Monitoring**: During administration, patients are closely monitored by nurses for any immediate reactions or discomfort. 5. **Cycle & Schedule**: Chemotherapy is administered in cycles, with periods of treatment followed by rest periods to allow the body to recover. The number of cycles and duration vary widely. 6. **Supportive Care**: Throughout treatment, supportive medications (anti-emetics, growth factors) are provided to manage side effects and maintain quality of life.
Benefits
<h2>Benefits of Chemotherapy for Cancer</h2><ul><li><h3>Cancer Cell Destruction:</h3><p>Chemotherapy directly targets and destroys cancer cells throughout the body, including those that may have spread to distant sites (metastases).</p></li><li><h3>Tumor Shrinkage:</h3><p>Can significantly reduce tumor size, making surgery easier or alleviating pressure on organs, improving quality of life.</p></li><li><h3>Disease Control & Remission:</h3><p>For many cancers, chemotherapy can lead to complete remission or long-term control of the disease, extending life expectancy.</p></li><li><h3>Adjuvant/Neoadjuvant Therapy:</h3><p>Used before surgery (neoadjuvant) to shrink tumors or after surgery (adjuvant) to kill any remaining cancer cells, reducing recurrence risk.</p></li><li><h3>Palliative Care:</h3><p>Can relieve cancer-related symptoms like pain or obstruction, significantly improving a patient's comfort and quality of life in advanced stages.</p></li><li><h3>Part of Multimodal Treatment:</h3><p>Often combined with radiation, surgery, targeted therapy, or immunotherapy to enhance overall treatment effectiveness.</p></li></ul>
Recovery Information
<h2>Recovery and Life After Chemotherapy</h2><p>Recovery from chemotherapy is a gradual process that varies greatly depending on the individual, the type and duration of chemotherapy, and the cancer being treated. While the acute side effects typically subside weeks to months after the last cycle, some long-term effects may persist.</p><h3>Immediate Post-Treatment</h3><ul><li><strong>Managing Side Effects:</strong> Fatigue, nausea, hair loss, mouth sores, and increased infection risk are common. Your medical team will provide medications and strategies to manage these.</li><li><strong>Rest and Nutrition:</strong> Adequate rest and a balanced diet are crucial for recovery and rebuilding strength.</li></ul><h3>Long-Term Recovery & Wellness</h3><ul><li><strong>Regular Follow-ups:</strong> Essential for monitoring your health, checking for recurrence, and managing any persistent side effects.</li><li><strong>Physical Therapy:</strong> May be recommended to regain strength and mobility, especially if muscle weakness or neuropathy occurred.</li><li><strong>Emotional and Psychological Support:</strong> Dealing with cancer and its treatment can be emotionally challenging. Counseling, support groups, or psychological therapy can be highly beneficial. DivinHeal offers access to such support services.</li><li><strong>Lifestyle Adjustments:</strong> Adopting a healthy lifestyle, including regular exercise (as tolerated) and a nutritious diet, is vital for long-term well-being and reducing the risk of recurrence.</li><li><strong>Fertility Preservation:</strong> Discuss options if chemotherapy impacts fertility, a critical consideration for many patients.</li></ul><p>DivinHeal's care coordinators will guide you through this recovery phase, connecting you with specialists and resources to ensure a holistic healing journey.</p>

radiation therapy cancer
Treatment Price
$4000.00 USDTreatment Overview
Radiation therapy for cancer aims to destroy cancerous cells while minimizing damage to surrounding healthy tissue. This is achieved by precisely delivering high doses of radiation to the tumor area. Techniques range from conventional external beam radiation to highly sophisticated methods like Intensity-Modulated Radiation Therapy (IMRT), Stereotactic Body Radiation Therapy (SBRT), and proton therapy. DivinHeal facilitates access to cutting-edge technology and experienced radiation oncologists worldwide, ensuring personalized treatment plans focused on optimal outcomes and patient safety for <strong>radiation therapy cancer</strong> patients.
Procedures
Radiation therapy for cancer involves several precise steps to ensure effective treatment delivery: 1. **Consultation and Diagnosis:** An initial consultation with a radiation oncologist to review diagnosis, medical history, and suitability for radiation therapy. 2. **Treatment Planning (Simulation):** This crucial phase involves a CT scan (sometimes combined with MRI or PET) of the treatment area. The data is used to create a detailed 3D map of the tumor and surrounding healthy organs. The radiation oncologist and medical physicist then design a personalized treatment plan, determining the exact angles, intensity, and dosage of radiation. 3. **Fiducial Placement (if needed):** For some treatments, tiny markers (fiducials) may be placed inside the body to help precisely target the radiation. 4. **Treatment Delivery:** Patients lie on a treatment table, often with immobilization devices, while a linear accelerator (LINAC) or other specialized machine delivers radiation. Each session typically lasts 15-30 minutes, with the actual radiation delivery lasting only a few minutes. 5. **Frequency:** Sessions are usually given once a day, five days a week, for a period ranging from 1 to 8 weeks, depending on the cancer type and treatment goal. 6. **Monitoring:** Throughout the course, patients are regularly monitored by their care team for side effects and treatment response. Imaging scans may be repeated to ensure accurate targeting as the tumor shrinks or body changes occur. 7. **Post-Treatment Follow-up:** After the final session, follow-up appointments are scheduled to assess recovery, manage side effects, and monitor for recurrence.
Benefits
The benefits of radiation therapy for cancer are substantial and include: <ul> <li><strong>High Efficacy:</strong> Effectively destroys cancer cells and shrinks tumors, often leading to a cure, especially in early-stage cancers or when combined with other therapies.</li> <li><strong>Organ Preservation:</strong> In many cases, it can eliminate the need for surgery or allow for less invasive surgery, preserving organ function and appearance (e.g., breast cancer, larynx cancer).</li> <li><strong>Pain Relief:</strong> Excellent for palliative care, significantly reducing pain, bleeding, or other symptoms caused by advanced tumors.</li> <li><strong>Precision:</strong> Modern techniques like IMRT, SBRT, and proton therapy allow for highly targeted radiation delivery, minimizing damage to healthy tissues and reducing side effects.</li> <li><strong>Outpatient Convenience:</strong> Most radiation therapy sessions are conducted on an outpatient basis, allowing patients to maintain a relatively normal daily routine.</li> <li><strong>Improved Quality of Life:</strong> By effectively treating cancer and managing symptoms, radiation therapy can significantly improve a patient's quality of life.</li> </ul> DivinHeal ensures access to centers with advanced technology for precise and effective <strong>radiation therapy cancer treatment</strong>.
Recovery Information
Recovery from radiation therapy for cancer can vary widely depending on the treated area, the dose received, and the individual's overall health. Common short-term side effects include skin irritation (redness, dryness, peeling), fatigue, and localized pain or swelling. These usually subside within a few weeks to months after treatment ends. Long-term recovery may involve managing persistent fatigue, subtle tissue changes, or potential secondary effects depending on the treated site. Patients are encouraged to follow a healthy diet, stay hydrated, engage in gentle exercise, and attend all follow-up appointments. DivinHeal's post-treatment care coordination includes advice on nutrition, physical therapy, and emotional support to aid in a holistic recovery, helping patients navigate the challenges of <strong>radiation therapy cancer recovery time and tips</strong> for optimal well-being.

melanoma surgery
Treatment Price
$3500.00 USDOverview of Melanoma Surgery Goals and Techniques
The primary goal of melanoma surgery is curative, focusing on complete removal of the cancerous lesion. Depending on the stage and depth of the melanoma, techniques range from wide local excision for early-stage melanomas to more complex procedures like sentinel lymph node biopsy (SLNB) or complete lymph node dissection (CLND) for more advanced cases. Reconstruction may also be performed to optimize aesthetic and functional outcomes. DivinHeal connects patients with leading surgical oncologists specializing in advanced dermatological oncology.
Overview of Melanoma Surgery Goals and Techniques
The primary goal of melanoma surgery is curative, focusing on complete removal of the cancerous lesion. Depending on the stage and depth of the melanoma, techniques range from wide local excision for early-stage melanomas to more complex procedures like sentinel lymph node biopsy (SLNB) or complete lymph node dissection (CLND) for more advanced cases. Reconstruction may also be performed to optimize aesthetic and functional outcomes. DivinHeal connects patients with leading surgical oncologists specializing in advanced dermatological oncology.
Treatment Overview
<h2>Overview of Melanoma Surgery Goals and Techniques</h2><p>The primary goal of melanoma surgery is curative, focusing on complete removal of the cancerous lesion. Depending on the stage and depth of the melanoma, techniques range from wide local excision for early-stage melanomas to more complex procedures like sentinel lymph node biopsy (SLNB) or complete lymph node dissection (CLND) for more advanced cases. Reconstruction may also be performed to optimize aesthetic and functional outcomes. DivinHeal connects patients with leading surgical oncologists specializing in advanced dermatological oncology.</p>
Procedures
The specific steps of melanoma surgery vary based on the type of procedure. For a **Wide Local Excision**: 1. **Anesthesia:** Local anesthesia is typically used for smaller lesions; general anesthesia may be used for larger or more complex cases. 2. **Incision:** The surgeon makes an incision around the melanoma, including the predefined margin of healthy skin, forming an elliptical shape. 3. **Tissue Removal:** The cancerous tissue and the healthy margin are carefully excised. 4. **Wound Closure:** The wound is then closed with sutures. For larger defects, skin grafting or flap surgery may be required. For a **Sentinel Lymph Node Biopsy (SLNB)**: 1. **Injection:** A radioactive tracer and/or blue dye is injected near the melanoma. 2. **Mapping:** The tracer/dye travels to the first lymph nodes (sentinel nodes) to which the cancer cells would most likely spread. 3. **Removal:** The surgeon identifies and removes these sentinel nodes. 4. **Pathology:** The nodes are sent for immediate pathological analysis to detect microscopic cancer cells. If positive, further treatment may be considered.
Benefits
<h2>Benefits of Melanoma Surgery</h2><ul><li><h3>High Success Rate</h3><p>Especially when detected early, melanoma surgery offers a high cure rate and excellent long-term prognosis.</p></li><li><h3>Curative Potential</h3><p>For localized melanoma, surgical excision is often curative, completely removing the cancerous cells.</p></li><li><h3>Precise Tumor Removal</h3><p>Techniques like wide local excision ensure thorough removal of the primary tumor and surrounding at-risk tissue.</p></li><li><h3>Reduced Risk of Metastasis</h3><p>Timely surgical intervention significantly reduces the likelihood of the cancer spreading to lymph nodes or distant organs.</p></li><li><h3>Improved Quality of Life</h3><p>Successful surgery alleviates health concerns, allowing patients to return to a normal, active life.</p></li><li><h3>Access to Advanced Care</h3><p>DivinHeal provides access to hospitals with cutting-edge surgical technology and multidisciplinary teams, including reconstructive surgeons.</p></li></ul>
Recovery Information
<h2>Melanoma Surgery Recovery Time and Tips</h2><h3>Immediate Post-Operative Period</h3><p>After melanoma surgery, patients typically experience some pain, swelling, and bruising around the surgical site. Pain is usually managed with prescribed medication. The wound will be dressed, and instructions for wound care will be provided.</p><h3>Recovery Timeline</h3><ul><li><h4>Simple Excision</h4><p>For small, superficial melanomas, recovery is often quick. Stitches are typically removed within 7-14 days. Full activity can often resume within 2-3 weeks, though heavy lifting may be restricted longer.</p></li><li><h4>Larger Excisions & Lymph Node Dissection</h4><p>Recovery can take 4-6 weeks or longer. Drains may be placed after lymph node dissection and removed when fluid output decreases. Physical therapy may be recommended to regain full range of motion, especially if lymph nodes in the armpit or groin were removed.</p></li></ul><h3>Key Recovery Tips</h3><ul><li><h4>Follow Wound Care Instructions</h4><p>Keep the surgical site clean and dry. Report any signs of infection (redness, warmth, pus, increasing pain).</p></li><li><h4>Manage Pain</h4><p>Take prescribed pain medication as directed.</p></li><li><h4>Avoid Strenuous Activity</h4><p>Limit activities that could put tension on the incision line to prevent complications and promote healing.</p></li><li><h4>Sun Protection</h4><p>Strictly protect all skin from sun exposure, especially the surgical scar, using high SPF sunscreen, protective clothing, and seeking shade.</p></li><li><h4>Scar Management</h4><p>Once the wound has healed, discuss scar management options (e.g., silicone sheets, massage) with your surgeon.</p></li><li><h4>Emotional Support</h4><p>Connect with support groups or counseling services to address any emotional or psychological impact of the diagnosis and treatment.</p></li><li><h4>Regular Follow-ups</h4><p>Adhere to your oncologist's schedule for follow-up appointments, which are crucial for monitoring recurrence and performing skin exams.</p></li><li><h4>DivinHeal Post-Care</h4><p>Our dedicated care coordinators will remain in touch, assisting with remote consultations and ensuring continuity of care.</p></li></ul>

sarcoma surgery
Treatment Price
$5000.00 USDSarcoma surgery involves the careful excision of malignant tumors arising from connective tissues like bone, cartilage, fat, muscle, blood vessels, or fibrous tissue. The primary goal is complete tumor removal (R0 resection) with clear margins to prevent recurrence. Advanced techniques, including limb-sparing surgery and reconstructive procedures, are often employed to maintain functionality and cosmetic appearance. Adjuvant therapies like radiation or chemotherapy may complement surgery to eliminate remaining cancer cells.
Sarcoma surgery involves the careful excision of malignant tumors arising from connective tissues like bone, cartilage, fat, muscle, blood vessels, or fibrous tissue. The primary goal is complete tumor removal (R0 resection) with clear margins to prevent recurrence. Advanced techniques, including limb-sparing surgery and reconstructive procedures, are often employed to maintain functionality and cosmetic appearance. Adjuvant therapies like radiation or chemotherapy may complement surgery to eliminate remaining cancer cells.
Treatment Overview
Sarcoma surgery involves the careful excision of malignant tumors arising from connective tissues like bone, cartilage, fat, muscle, blood vessels, or fibrous tissue. The primary goal is complete tumor removal (R0 resection) with clear margins to prevent recurrence. Advanced techniques, including limb-sparing surgery and reconstructive procedures, are often employed to maintain functionality and cosmetic appearance. Adjuvant therapies like radiation or chemotherapy may complement surgery to eliminate remaining cancer cells.
Procedures
Sarcoma surgery involves several critical steps: 1. <strong>Pre-operative Planning:</strong> Detailed imaging (MRI, CT, PET scans) and biopsy results are reviewed by a multidisciplinary team to precisely map the tumor's location, size, and relationship to vital structures. 2. <strong>Anesthesia:</strong> General anesthesia is administered. 3. <strong>Incision:</strong> A carefully planned incision is made to provide adequate access to the tumor while minimizing damage to surrounding healthy tissue. 4. <strong>Tumor Resection:</strong> The surgical oncologist meticulously removes the sarcoma along with a margin of healthy tissue (wide local excision) to ensure clear margins and reduce the risk of recurrence. For bone sarcomas, this may involve removing a segment of bone and replacing it with a prosthesis or bone graft (limb-sparing surgery). For soft tissue sarcomas, care is taken to preserve nerves, blood vessels, and muscles where possible. 5. <strong>Lymph Node Dissection (if indicated):</strong> Although sarcomas rarely spread to lymph nodes, in specific types (e.g., rhabdomyosarcoma, epithelioid sarcoma), lymph node removal may be performed. 6. <strong>Reconstruction:</strong> If a significant amount of tissue or bone has been removed, reconstructive surgery (using local tissue flaps, free flaps, or prosthetic implants) may be performed immediately to restore function and appearance. 7. <strong>Wound Closure:</strong> The surgical site is carefully closed in layers. Drains may be placed to remove excess fluid, and a sterile dressing is applied. 8. <strong>Post-operative Care:</strong> Patients are monitored in recovery, and pain management is initiated. Rehabilitation often begins soon after surgery.
Benefits
<h2>Benefits of Sarcoma Surgery</h2> <ul> <li><strong>Primary Cure:</strong> For many localized sarcomas, surgery offers the best chance for complete removal of the tumor and a potential cure.</li> <li><strong>Disease Control:</strong> Even in advanced cases, surgical removal can reduce tumor burden, alleviate symptoms, and improve quality of life.</li> <li><strong>Limb Preservation:</strong> Advanced surgical techniques, often combined with neo-adjuvant therapies, allow for the removal of tumors while preserving the affected limb and its function, avoiding amputation.</li> <li><strong>Pain Relief:</strong> Removal of a bulky or nerve-compressing tumor can significantly reduce pain and discomfort.</li> <li><strong>Improved Functionality:</strong> When combined with reconstructive surgery and physical therapy, sarcoma surgery can help restore function to affected areas.</li> <li><strong>Enhanced Prognosis:</strong> Complete surgical resection is a critical factor in improving long-term survival rates for sarcoma patients.</li> <li><strong>Accurate Staging:</strong> Surgical samples provide detailed pathological information vital for accurate staging and guiding further treatment decisions.</li> </ul>
Recovery Information
<h2>Recovery After Sarcoma Surgery</h2> <p>Recovery time following sarcoma surgery can vary significantly depending on the tumor's location, size, the complexity of the surgery, and whether reconstructive procedures were performed. Generally, patients can expect:</p> <ul> <li><strong>Initial Hospital Stay:</strong> Typically 3 to 7 days, during which pain management, wound care, and early mobilization are managed.</li> <li><strong>Acute Recovery (First 2-4 Weeks):</strong> Focus on wound healing, managing post-operative pain and swelling, and gradually increasing activity levels. Patients may require assistance with daily activities.</li> <li><strong>Rehabilitation and Physical Therapy (Weeks to Months):</strong> Crucial for regaining strength, mobility, and function, especially after limb-sparing surgery. A structured rehabilitation program, often with a physical therapist, is essential for optimal recovery.</li> <li><strong>Return to Normal Activities:</strong> Most patients can gradually return to light activities within 4-8 weeks, with full recovery and resumption of strenuous activities potentially taking 3-6 months or longer.</li> <li><strong>Emotional Support:</strong> Dealing with a cancer diagnosis and major surgery can be emotionally challenging. Counseling and support groups are invaluable during this period.</li> <li><strong>Long-term Follow-up:</strong> Regular check-ups with the oncology team, including imaging scans, are vital for monitoring recovery and detecting any signs of recurrence.</li> </ul>

lung cancer surgery
Treatment Price
$7000.00 USDOverview of Lung Cancer Surgery Goals
The primary goal of lung cancer surgery is to completely remove the tumor and surrounding affected lymph nodes, preventing recurrence and spreading. Techniques range from minimally invasive Video-Assisted Thoracoscopic Surgery (VATS) or Robotic-Assisted Thoracoscopic Surgery (RATS) for smaller tumors to traditional open thoracotomy for larger or more complex cases, ensuring precision and optimal patient safety.
Overview of Lung Cancer Surgery Goals
The primary goal of lung cancer surgery is to completely remove the tumor and surrounding affected lymph nodes, preventing recurrence and spreading. Techniques range from minimally invasive Video-Assisted Thoracoscopic Surgery (VATS) or Robotic-Assisted Thoracoscopic Surgery (RATS) for smaller tumors to traditional open thoracotomy for larger or more complex cases, ensuring precision and optimal patient safety.
Treatment Overview
<h2>Overview of Lung Cancer Surgery Goals</h2><p>The primary goal of lung cancer surgery is to completely remove the tumor and surrounding affected lymph nodes, preventing recurrence and spreading. Techniques range from minimally invasive Video-Assisted Thoracoscopic Surgery (VATS) or Robotic-Assisted Thoracoscopic Surgery (RATS) for smaller tumors to traditional open thoracotomy for larger or more complex cases, ensuring precision and optimal patient safety.</p>
Procedures
Lung cancer surgery typically begins with general anesthesia. For open thoracotomy, a large incision is made on the chest, and ribs are spread to access the lung. For minimally invasive VATS or RATS, several small incisions are made, through which a camera and surgical instruments are inserted. The surgeon carefully dissects the lung tissue, identifies the tumor, and removes the affected lobe (lobectomy), segment (segmentectomy), or entire lung (pneumonectomy) along with surrounding lymph nodes. Blood vessels and airways are sealed. After ensuring no air leaks and proper hemostasis, chest tubes are inserted to drain fluids and air, and the incisions are closed with sutures or staples.
Benefits
<h2>Benefits of Lung Cancer Surgery</h2><p>For eligible patients, lung cancer surgery offers several significant benefits:</p><ul><li><strong>Potential for Cure:</strong> Especially in early-stage lung cancer, surgical removal of the tumor can lead to complete remission and significantly improved long-term survival rates.</li><li><strong>Improved Quality of Life:</strong> Removing cancerous tissue can alleviate symptoms such as pain, coughing, and breathing difficulties, enhancing overall well-being.</li><li><strong>Accurate Staging:</strong> Surgical removal allows for precise pathological examination of the tumor and lymph nodes, leading to more accurate cancer staging and guiding further treatment.</li><li><strong>Reduced Risk of Recurrence:</strong> Complete tumor removal minimizes the chances of local recurrence and spread to other parts of the body.</li><li><strong>Integration with Multimodal Therapy:</strong> Surgery can be combined effectively with chemotherapy, radiation therapy, or targeted therapy to optimize outcomes, particularly in more advanced cases.</li></ul><p>DivinHeal connects you with top-tier thoracic surgeons who prioritize patient safety and effective outcomes for your lung cancer surgery.</p>
Recovery Information
<h2>Lung Cancer Surgery Recovery Time and Tips</h2><p>Recovery after lung cancer surgery varies based on the type of procedure (e.g., VATS vs. open thoracotomy), the patient's overall health, and potential complications. Generally, patients can expect:</p><ul><li><strong>Hospital Stay:</strong> Typically 5-10 days, during which pain management, breathing exercises, and early mobilization are crucial.</li><li><strong>Initial Recovery (First 2-4 Weeks):</strong> Patients will experience some pain or discomfort at the incision site, fatigue, and shortness of breath. Gradual increase in activity is encouraged.</li><li><strong>Full Recovery:</strong> Most patients can resume light activities within 4-6 weeks, with a full return to normal activities taking 2-3 months. Pulmonary rehabilitation plays a vital role in restoring lung function.</li></ul><h3>Tips for a Smooth Recovery:</h3><ul><li><strong>Follow Medical Advice:</strong> Adhere strictly to your surgeon's instructions regarding wound care, medications, and activity levels.</li><li><strong>Pain Management:</strong> Utilize prescribed pain medication to stay comfortable and facilitate movement and breathing exercises.</li><li><strong>Breathing Exercises:</strong> Regularly perform deep breathing and coughing exercises to prevent pneumonia and improve lung capacity.</li><li><strong>Physical Activity:</strong> Start with gentle walks and gradually increase activity as tolerated to regain strength and prevent blood clots.</li><li><strong>Nutrition:</strong> Maintain a healthy, balanced diet to support healing and energy levels.</li><li><strong>Smoking Cessation:</strong> If you smoke, quitting is imperative for recovery and long-term health.</li><li><strong>Emotional Support:</strong> Seek support from family, friends, or support groups to cope with the emotional aspects of recovery.</li></ul><p>DivinHeal's dedicated care coordinators provide continuous support and guidance throughout your recovery journey, connecting you with resources for rehabilitation and emotional well-being after your lung cancer surgery.</p>

kidney cancer surgery
Treatment Price
$6500.00 USDKidney Cancer Surgery: A Path to Recovery
Kidney cancer surgery, often referred to as nephrectomy, is a critical intervention designed to treat renal cell carcinoma and other kidney malignancies. The primary goal is to eradicate the cancerous tissue, preventing its spread and safeguarding the patient's long-term health. At DivinHeal, we facilitate access to state-of-the-art hospitals in India renowned for their expertise in urological oncology, employing techniques like open, laparoscopic, and robotic-assisted surgeries for precision and quicker recovery. Our focus is on providing comprehensive, quality care that is both effective and affordable.
Kidney Cancer Surgery: A Path to Recovery
Kidney cancer surgery, often referred to as nephrectomy, is a critical intervention designed to treat renal cell carcinoma and other kidney malignancies. The primary goal is to eradicate the cancerous tissue, preventing its spread and safeguarding the patient's long-term health. At DivinHeal, we facilitate access to state-of-the-art hospitals in India renowned for their expertise in urological oncology, employing techniques like open, laparoscopic, and robotic-assisted surgeries for precision and quicker recovery. Our focus is on providing comprehensive, quality care that is both effective and affordable.
Treatment Overview
<h2>Kidney Cancer Surgery: A Path to Recovery</h2><p>Kidney cancer surgery, often referred to as nephrectomy, is a critical intervention designed to treat renal cell carcinoma and other kidney malignancies. The primary goal is to eradicate the cancerous tissue, preventing its spread and safeguarding the patient's long-term health. At DivinHeal, we facilitate access to state-of-the-art hospitals in India renowned for their expertise in urological oncology, employing techniques like open, laparoscopic, and robotic-assisted surgeries for precision and quicker recovery. Our focus is on providing comprehensive, quality care that is both effective and affordable.</p>
Procedures
Kidney cancer surgery, primarily nephrectomy, involves removing part or all of the cancerous kidney. In a radical nephrectomy, the entire kidney, a portion of the ureter, the adrenal gland, and surrounding fatty tissue/lymph nodes are removed through an incision in the abdomen or side. A partial nephrectomy, or kidney-sparing surgery, removes only the tumor and a small amount of surrounding healthy tissue, preserving the rest of the kidney. These procedures can be performed via traditional open surgery, or minimally invasively using laparoscopy or robotic assistance, where small incisions are made, and specialized instruments and a camera are used to perform the surgery.
Benefits
<h2>Benefits of Modern Kidney Cancer Surgery</h2><ul><li><h3>High Success Rates:</h3><p>Especially for early-stage kidney cancers, surgical removal offers excellent long-term survival rates.</p></li><li><h3>Minimally Invasive Options:</h3><p>Laparoscopic and robotic-assisted techniques lead to less pain, smaller scars, reduced blood loss, and faster recovery compared to open surgery.</p></li><li><h3>Kidney-Sparing Possibilities:</h3><p>Partial nephrectomy allows for the preservation of healthy kidney tissue, crucial for patients with pre-existing kidney conditions or those at risk of future kidney problems.</p></li><li><h3>Improved Quality of Life:</h3><p>Effective treatment can alleviate symptoms, prevent disease progression, and restore a sense of well-being.</p></li><li><h3>Access to Advanced Care:</h3><p>DivinHeal ensures access to hospitals equipped with the latest surgical technology and highly skilled urological oncology teams.</p></li></ul>
Recovery Information
<h2>Kidney Cancer Surgery Recovery Time and Tips</h2><p>Recovery from kidney cancer surgery varies depending on the type of procedure performed (open vs. minimally invasive) and individual health factors. Generally:</p><ul><li><h3>Hospital Stay:</h3><p>Typically 3-7 days for open surgery, and 2-5 days for laparoscopic or robotic procedures.</p></li><li><h3>Initial Recovery (First 2-4 Weeks):</h3><p>Focus on managing pain, gradually increasing activity, and adhering to dietary recommendations. Patients may experience fatigue and mild discomfort.</p></li><li><h3>Full Recovery (6-12 Weeks):</h3><p>Most patients can resume normal activities, including work and light exercise. Strenuous activities and heavy lifting should be avoided for several weeks.</p></li></ul><h3>Recovery Tips:</h3><ul><li><strong>Follow Medical Advice:</strong> Adhere strictly to post-operative instructions regarding wound care, medication, and activity levels.</li><li><strong>Stay Hydrated:</strong> Drink plenty of fluids to support kidney function.</li><li><strong>Gentle Movement:</strong> Start with short walks to aid circulation and prevent complications.</li><li><strong>Balanced Diet:</strong> Focus on nutrient-rich foods to support healing.</li><li><strong>Emotional Support:</strong> Utilize counseling or support groups to manage emotional aspects of recovery. DivinHeal assists with connecting you to comprehensive post-operative support.</li></ul>

prostate cancer surgery
Treatment Price
$8000.00 USDProstate Cancer Surgery: Overview and Goals
Prostate cancer surgery, primarily radical prostatectomy, aims to remove cancerous tissue from the prostate gland, often along with nearby lymph nodes, to achieve a cure for localized prostate cancer. Modern techniques, especially Robotic-Assisted Radical Prostatectomy (RARP), prioritize precise cancer removal while striving to preserve urinary continence and erectile function. DivinHeal connects you with top uro-oncologists and advanced facilities in India specializing in these life-saving procedures.
Prostate Cancer Surgery: Overview and Goals
Prostate cancer surgery, primarily radical prostatectomy, aims to remove cancerous tissue from the prostate gland, often along with nearby lymph nodes, to achieve a cure for localized prostate cancer. Modern techniques, especially Robotic-Assisted Radical Prostatectomy (RARP), prioritize precise cancer removal while striving to preserve urinary continence and erectile function. DivinHeal connects you with top uro-oncologists and advanced facilities in India specializing in these life-saving procedures.
Treatment Overview
<h2>Prostate Cancer Surgery: Overview and Goals</h2><p>Prostate cancer surgery, primarily radical prostatectomy, aims to remove cancerous tissue from the prostate gland, often along with nearby lymph nodes, to achieve a cure for localized prostate cancer. Modern techniques, especially Robotic-Assisted Radical Prostatectomy (RARP), prioritize precise cancer removal while striving to preserve urinary continence and erectile function. DivinHeal connects you with top uro-oncologists and advanced facilities in India specializing in these life-saving procedures.</p>
Procedures
Prostate cancer surgery, specifically a radical prostatectomy, involves several key steps. After general anesthesia, the surgeon makes an incision (for open surgery) or several small incisions (for laparoscopic/robotic surgery) in the lower abdomen. If using a robotic system, the surgeon controls robotic arms equipped with surgical tools and a high-definition 3D camera. The prostate gland, along with the seminal vesicles, is carefully dissected and separated from surrounding tissues. Nerves responsible for erectile function are meticulously preserved if the cancer's location allows (nerve-sparing technique). Nearby lymph nodes may also be removed if there's a risk of spread. Finally, the remaining urethra is reconnected to the bladder, and a temporary catheter is inserted to drain urine while the connection heals. All incisions are then closed.
Benefits
<h2>Benefits of Prostate Cancer Surgery</h2><ul><li><strong>High Cure Rates:</strong> For localized prostate cancer, radical prostatectomy offers excellent long-term survival rates.</li><li><strong>Definitive Treatment:</strong> Removes the entire cancerous gland, offering immediate pathological staging.</li><li><strong>Improved Quality of Life:</strong> For many, successful surgery leads to a return to a healthy, cancer-free life.</li><li><strong>Minimally Invasive Options:</strong> Robotic-assisted surgery offers benefits like less blood loss, reduced pain, shorter hospital stays, and quicker overall recovery.</li><li><strong>Expert Uro-Oncologists:</strong> DivinHeal connects you with world-class surgeons specializing in complex prostate procedures.</li></ul>
Recovery Information
<h2>Recovery and Life After Prostate Cancer Surgery</h2><p>Recovery after prostate cancer surgery, especially radical prostatectomy, is a gradual process focusing on regaining urinary continence and, for some, erectile function. The initial hospital stay is typically 3-7 days.</p><ul><li><strong>Catheter Care:</strong> A urinary catheter will remain in place for 1-3 weeks post-surgery to allow the urethra to heal.</li><li><strong>Pain Management:</strong> Mild pain and discomfort are common and managed with medication.</li><li><strong>Activity Levels:</strong> Gentle walking is encouraged soon after surgery. Strenuous activities and heavy lifting should be avoided for 4-6 weeks.</li><li><strong>Urinary Continence:</strong> Most men experience some degree of temporary incontinence immediately after catheter removal. Pelvic floor exercises (Kegels) are crucial for regaining bladder control, often improving significantly over 3-12 months.</li><li><strong>Erectile Function:</strong> Recovery of erectile function can take several months to two years and varies greatly among individuals, depending on factors like age, pre-operative function, and nerve-sparing techniques. Medications or other therapies may be prescribed to assist recovery.</li><li><strong>Follow-up:</strong> Regular PSA monitoring is essential to track cancer recurrence.</li></ul><p>DivinHeal offers comprehensive post-operative support, including access to rehabilitation specialists and follow-up care coordination to optimize your recovery journey.</p>

uterine cancer surgery
Treatment Price
$5000.00 USDUterine cancer surgery aims to eliminate cancerous cells, accurately determine the cancer's stage, and prevent its spread. Techniques range from minimally invasive laparoscopic or robotic-assisted procedures to traditional open surgery, commonly involving hysterectomy (removal of the uterus), salpingo-oophorectomy (removal of ovaries and fallopian tubes), and lymph node dissection. DivinHeal connects patients with leading oncological surgeons and state-of-the-art facilities, ensuring access to the best hospitals for uterine cancer surgery for optimal outcomes and peace of mind.
Uterine cancer surgery aims to eliminate cancerous cells, accurately determine the cancer's stage, and prevent its spread. Techniques range from minimally invasive laparoscopic or robotic-assisted procedures to traditional open surgery, commonly involving hysterectomy (removal of the uterus), salpingo-oophorectomy (removal of ovaries and fallopian tubes), and lymph node dissection. DivinHeal connects patients with leading oncological surgeons and state-of-the-art facilities, ensuring access to the best hospitals for uterine cancer surgery for optimal outcomes and peace of mind.
Treatment Overview
Uterine cancer surgery aims to eliminate cancerous cells, accurately determine the cancer's stage, and prevent its spread. Techniques range from minimally invasive laparoscopic or robotic-assisted procedures to traditional open surgery, commonly involving hysterectomy (removal of the uterus), salpingo-oophorectomy (removal of ovaries and fallopian tubes), and lymph node dissection. DivinHeal connects patients with leading oncological surgeons and state-of-the-art facilities, ensuring access to the best hospitals for uterine cancer surgery for optimal outcomes and peace of mind.
Procedures
Uterine cancer surgery typically involves several meticulous steps. After administering general anesthesia, the surgeon makes an incision (either an abdominal incision for open surgery or several small incisions for laparoscopic/robotic-assisted surgery). The primary procedure is a hysterectomy, which is the complete removal of the uterus. This often includes a bilateral salpingo-oophorectomy (removal of both ovaries and fallopian tubes) to prevent recurrence and further disease spread. Lymph node dissection may also be performed to check if cancer cells have spread to the lymph nodes, which is crucial for accurate staging. For very early-stage cases in select patients, a less extensive surgery might be considered to preserve fertility. After the cancerous tissues are carefully removed, the surgical site is meticulously closed. The removed tissue is then sent for thorough pathological examination to confirm the diagnosis, accurately stage the cancer, and guide any further adjuvant treatments such as uterine cancer chemotherapy and radiation therapy.
Benefits
<h2>Benefits of Uterine Cancer Surgery Treatment</h2><ul><li><h3>High Success Rates</h3><p>Especially for early-stage uterine cancer, surgical removal offers excellent long-term survival rates, giving patients the best chance at a full recovery and a healthy future.</p></li><li><h3>Accurate Staging</h3><p>Surgery allows for definitive pathological staging, which is crucial for guiding subsequent uterine cancer diagnosis and therapy options and ensuring a precise prognosis.</p></li><li><h3>Effective Symptom Relief</h3><p>Can alleviate distressing symptoms such as abnormal bleeding, pain, or pressure caused by the tumor, significantly improving quality of life.</p></li><li><h3>Comprehensive Treatment Plan</h3><p>Often integrated into a multimodal treatment strategy alongside uterine cancer chemotherapy and radiation therapy, enhancing overall therapeutic efficacy and long-term outcomes.</p></li><li><h3>Access to Advanced Techniques</h3><p>DivinHeal connects you to leading hospitals offering minimally invasive options (laparoscopic, robotic surgery) resulting in faster uterine cancer surgery recovery time, less pain, and smaller scars, ensuring a more comfortable post-operative experience.</p></li></ul>
Recovery Information
<h2>Uterine Cancer Surgery Recovery Time and Tips</h2><h3>Immediate Post-Operative Period</h3><p>Recovery time varies based on the type of uterine cancer surgery (open vs. minimally invasive) and individual patient factors. Typically, the hospital stay is 3-7 days. Pain management, meticulous monitoring for complications, and early mobilization are key during this phase to promote healing.</p><h3>Long-Term Recovery and Rehabilitation</h3><p>Full uterine cancer surgery recovery time can range from 4-8 weeks for open surgery and 2-4 weeks for minimally invasive procedures. Patients will gradually resume normal activities, avoiding heavy lifting and strenuous exercise initially. DivinHeal assists with comprehensive post-operative care, including:<ul><li>Physical therapy guidance to restore strength and mobility.</li><li>Nutritional counseling for optimal healing and overall wellness.</li><li>Emotional and psychological support to cope with the diagnosis and treatment journey.</li><li>Regular follow-up appointments with top oncologists for uterine cancer surgery to monitor recovery and detect any recurrence, ensuring peace of mind.</li></ul></p>

whipple surgery
Treatment Price
$8500.00 USDOverview of Whipple Surgery Goals
The primary goal of Whipple surgery treatment is to completely remove cancerous or pre-cancerous tumors from the pancreatic head region, aiming for a potential cure and improved long-term survival. This procedure requires exceptional surgical precision and a multidisciplinary approach involving highly experienced surgical oncologists, gastroenterologists, radiologists, and pathologists. DivinHeal connects you with top-tier hospitals equipped with advanced facilities and teams specialized in performing this life-saving procedure.
Overview of Whipple Surgery Goals
The primary goal of Whipple surgery treatment is to completely remove cancerous or pre-cancerous tumors from the pancreatic head region, aiming for a potential cure and improved long-term survival. This procedure requires exceptional surgical precision and a multidisciplinary approach involving highly experienced surgical oncologists, gastroenterologists, radiologists, and pathologists. DivinHeal connects you with top-tier hospitals equipped with advanced facilities and teams specialized in performing this life-saving procedure.
Treatment Overview
<h2>Overview of Whipple Surgery Goals</h2><p>The primary goal of <b>Whipple surgery treatment</b> is to completely remove cancerous or pre-cancerous tumors from the pancreatic head region, aiming for a potential cure and improved long-term survival. This procedure requires exceptional surgical precision and a multidisciplinary approach involving highly experienced surgical oncologists, gastroenterologists, radiologists, and pathologists. DivinHeal connects you with top-tier hospitals equipped with advanced facilities and teams specialized in performing this life-saving procedure.</p>
Procedures
Whipple surgery involves a midline incision in the abdomen. The surgeon carefully dissects and removes the head of the pancreas, the duodenum (the C-shaped first part of the small intestine), the gallbladder, and a portion of the common bile duct. Lymph nodes near the pancreas are also typically removed for staging. After resection, the remaining pancreas, bile duct, and stomach are meticulously reconnected to different sections of the small intestine to restore digestive continuity. This complex reconstruction, often referred to as pancreaticojejunostomy, choledochojejunostomy, and gastrojejunostomy, is the most critical and delicate part of the operation.
Benefits
<h2>Benefits of Whipple Surgery Treatment</h2><ul><li><h3>Potential for Cure</h3><p>For resectable pancreatic, ampullary, or bile duct cancers, Whipple surgery offers the best chance for long-term survival or even a complete cure.</p></li><li><h3>Improved Quality of Life</h3><p>Successful tumor removal can alleviate symptoms like jaundice, pain, and digestive issues, significantly enhancing a patient's quality of life.</p></li><li><h3>Accurate Staging</h3><p>The surgical removal allows for precise pathological staging, guiding subsequent treatment decisions like <b>Whipple surgery chemotherapy and radiation therapy</b>.</p></li><li><h3>Pain Relief</h3><p>By removing the tumor causing obstruction or nerve compression, the surgery can provide significant relief from debilitating pain.</p></li><li><h3>Access to Advanced Therapies</h3><p>Post-surgery, patients may become eligible for adjuvant treatments, including targeted therapies, which further improve outcomes.</p></li></ul>
Recovery Information
<h2>Whipple Surgery Recovery Time and Tips</h2><p>Recovery from Whipple surgery is a gradual process requiring patience and diligent follow-up. Typically, patients remain in the hospital for 7 to 14 days, often with an initial stay in the ICU. The immediate post-operative period focuses on pain management, monitoring for complications like pancreatic leaks, and gradually reintroducing oral intake. Full recovery can take several months, with gradual return to normal activities. DivinHeal provides comprehensive guidance on <b>Whipple surgery recovery time and tips</b>, including:</p><ul><li><h3>Dietary Adjustments</h3><p>Initially, a liquid diet progresses to soft, low-fat meals. Smaller, more frequent meals are often recommended to aid digestion.</p></li><li><h3>Activity Restrictions</h3><p>Avoid heavy lifting and strenuous activities for 6-8 weeks. Gradual increase in activity, like short walks, is encouraged.</p></li><li><h3>Wound Care</h3><p>Keep the surgical incision clean and dry, watching for signs of infection. Our team provides detailed instructions.</p></li><li><h3>Pain Management</h3><p>Medication will be prescribed to manage post-operative pain effectively. Communicate any discomfort to your care team.</p></li><li><h3>Emotional Support</h3><p>Undergoing a major surgery can be emotionally challenging. Counseling and support groups can be beneficial.</p></li><li><h3>Monitoring for Complications</h3><p>Be aware of symptoms like fever, increased pain, jaundice, or changes in bowel habits, and report them promptly.</p></li></ul>

liver cancer surgery
Treatment Price
$18000.00 USDLiver cancer surgery aims to completely remove cancerous lesions from the liver while preserving as much healthy liver tissue as possible. Techniques range from partial hepatectomy (resection) for localized tumors to liver transplantation for select cases, particularly primary liver cancer (HCC) in cirrhotic patients. Adjunctive therapies like ablation, TACE, or systemic treatments may also be used. Our goal is to ensure you receive precise, effective, and safe liver cancer treatment.
Liver cancer surgery aims to completely remove cancerous lesions from the liver while preserving as much healthy liver tissue as possible. Techniques range from partial hepatectomy (resection) for localized tumors to liver transplantation for select cases, particularly primary liver cancer (HCC) in cirrhotic patients. Adjunctive therapies like ablation, TACE, or systemic treatments may also be used. Our goal is to ensure you receive precise, effective, and safe liver cancer treatment.
Treatment Overview
Liver cancer surgery aims to completely remove cancerous lesions from the liver while preserving as much healthy liver tissue as possible. Techniques range from partial hepatectomy (resection) for localized tumors to liver transplantation for select cases, particularly primary liver cancer (HCC) in cirrhotic patients. Adjunctive therapies like ablation, TACE, or systemic treatments may also be used. Our goal is to ensure you receive precise, effective, and safe liver cancer treatment.
Procedures
Liver cancer surgery involves several key steps. Prior to surgery, extensive imaging (CT, MRI) and blood tests are performed to assess tumor characteristics and liver function. During a partial hepatectomy, an incision is made, and the surgeon carefully resects the cancerous portion of the liver, ensuring clear margins. Blood vessels and bile ducts are meticulously ligated or stapled. For a liver transplant, the diseased liver is removed and replaced with a healthy donor liver. Minimally invasive approaches use small incisions and specialized instruments. The procedure concludes with closure of the surgical site. The specific technique depends on the tumor's size, location, and type of liver cancer.
Benefits
<h2>Benefits of Liver Cancer Surgery</h2><ul><li><h3>Potential for Cure</h3><p>For early-stage and resectable tumors, surgery offers the best chance for long-term survival and even complete cure, significantly improving the liver cancer success rate.</p></li><li><h3>Improved Quality of Life</h3><p>Successful removal of tumors can alleviate symptoms, improve liver function, and enhance overall well-being, leading to a better quality of life post-treatment.</p></li><li><h3>Advanced Surgical Techniques</h3><p>Access to highly skilled hepatobiliary surgeons employing advanced open, laparoscopic, and robotic techniques for precise tumor removal and faster recovery.</p></li><li><h3>Multidisciplinary Approach</h3><p>Treatment plans are developed by a team of oncologists, surgeons, radiologists, and pathologists, ensuring comprehensive and personalized care, often including liver cancer chemotherapy and radiation therapy.</p></li><li><h3>Cost-Effective Treatment</h3><p>Through DivinHeal, patients access world-class liver cancer surgery in India at significantly lower costs compared to Western countries, making vital treatment more accessible.</p></li></ul>
Recovery Information
<h2>Liver Cancer Surgery Recovery Time and Tips</h2><p>The liver cancer surgery recovery time varies based on the type of surgery (open vs. minimally invasive), the extent of resection, and individual patient factors. Typically, hospital stay ranges from 7-14 days. Full recovery can take anywhere from 6 weeks to several months.</p><h3>Key Aspects of Recovery:</h3><ul><li><strong>Pain Management:</strong> Effective pain control is crucial in the immediate post-operative period.</li><li><strong>Mobility:</strong> Early ambulation is encouraged to prevent complications like blood clots and aid recovery.</li><li><strong>Diet:</strong> A modified diet will be recommended initially, gradually transitioning back to normal.</li><li><strong>Activity Restrictions:</strong> Heavy lifting and strenuous activities are restricted for several weeks.</li><li><strong>Follow-up Care:</strong> Regular follow-up appointments, including imaging and blood tests, are essential to monitor recovery and detect any recurrence.</li><li><strong>Emotional Support:</strong> Counseling and support groups can be invaluable for emotional well-being during recovery.</li></ul><p>DivinHeal provides comprehensive guidance and support throughout your recovery phase, connecting you with rehabilitation specialists and ensuring a smooth transition back to daily life.</p>

pancreatic cancer surgery
Treatment Price
$8000.00 USDOverview of Pancreatic Cancer Surgery
Pancreatic cancer surgery involves the removal of part or all of the pancreas affected by a tumor, often along with surrounding tissues such as parts of the small intestine, bile duct, gallbladder, and lymph nodes. The primary goal is curative resection for early-stage, resectable tumors. For locally advanced or borderline resectable cases, surgery might be part of a multi-modal approach following neoadjuvant chemotherapy or radiation. The procedure requires highly skilled surgical oncologists and advanced medical facilities, which DivinHeal ensures access to through its global network.
Overview of Pancreatic Cancer Surgery
Pancreatic cancer surgery involves the removal of part or all of the pancreas affected by a tumor, often along with surrounding tissues such as parts of the small intestine, bile duct, gallbladder, and lymph nodes. The primary goal is curative resection for early-stage, resectable tumors. For locally advanced or borderline resectable cases, surgery might be part of a multi-modal approach following neoadjuvant chemotherapy or radiation. The procedure requires highly skilled surgical oncologists and advanced medical facilities, which DivinHeal ensures access to through its global network.
Treatment Overview
<h2>Overview of Pancreatic Cancer Surgery</h2><p>Pancreatic cancer surgery involves the removal of part or all of the pancreas affected by a tumor, often along with surrounding tissues such as parts of the small intestine, bile duct, gallbladder, and lymph nodes. The primary goal is curative resection for early-stage, resectable tumors. For locally advanced or borderline resectable cases, surgery might be part of a multi-modal approach following neoadjuvant chemotherapy or radiation. The procedure requires highly skilled surgical oncologists and advanced medical facilities, which DivinHeal ensures access to through its global network.</p>
Procedures
Pancreatic cancer surgery, most commonly the Whipple procedure (pancreaticoduodenectomy), involves several meticulous steps. The patient is placed under general anesthesia. An incision is made in the abdomen, allowing the surgical team access to the pancreas. The surgeon carefully removes the head of the pancreas, the duodenum (the first part of the small intestine), the gallbladder, and a portion of the bile duct. Lymph nodes in the vicinity are also often removed to check for cancer spread. In some cases, a part of the stomach may also be removed. After the cancerous tissues are excised, the remaining digestive organs—the stomach, bile duct, and pancreas—are reconnected to the jejunum (middle part of the small intestine) to restore the flow of bile, digestive enzymes, and food. This complex reconstruction allows for normal digestion to resume. Drains are typically placed to remove fluid from the surgical site, and the incision is closed. The entire procedure can take 4-12 hours, depending on the complexity and the surgeon's technique.
Benefits
<h2>Benefits of Pancreatic Cancer Surgery</h2><ul><li><h3>Potential for Cure:</h3><p>For patients with early-stage, resectable tumors, surgery offers the best chance for complete eradication of the cancer and long-term survival.</p></li><li><h3>Improved Quality of Life:</h3><p>Successful surgery can alleviate symptoms such as pain, jaundice, and digestive issues caused by the tumor, significantly improving a patient's quality of life.</p></li><li><h3>Accurate Staging:</h3><p>Surgical removal allows for precise pathological examination of the tumor and surrounding lymph nodes, providing critical information for accurate staging and guiding subsequent treatment decisions.</p></li><li><h3>Enhanced Efficacy of Adjuvant Therapies:</h3><p>Removing the bulk of the tumor through surgery can make adjuvant chemotherapy or radiation therapy more effective in targeting remaining microscopic cancer cells and reducing recurrence risk.</p></li><li><h3>Access to Advanced Care via DivinHeal:</h3><p>With DivinHeal, you gain access to top-tier surgical oncologists and advanced facilities globally, ensuring the highest standards of care, even for complex procedures like pancreatic cancer surgery.</p></li></ul>
Recovery Information
<h2>Recovery and Life After Pancreatic Cancer Surgery</h2><p>Recovery from pancreatic cancer surgery, particularly a Whipple procedure, is a significant process that requires patience and dedicated care. The initial hospital stay typically ranges from 7 to 14 days, followed by several weeks or months of recovery at home.</p><h3>Key Aspects of Recovery:</h3><ul><li><h4>Pain Management:</h4><p>Post-operative pain is managed with medication, gradually decreasing as you heal.</p></li><li><h4>Dietary Adjustments:</h4><p>You'll start with liquids and slowly progress to soft foods. Many patients require pancreatic enzyme supplements to aid digestion due to changes in the digestive system.</p></li><li><h4>Activity Restrictions:</h4><p>Heavy lifting and strenuous activities are restricted for several weeks to prevent complications like hernias. Gradual increase in activity, including walking, is encouraged.</p></li><li><h4>Monitoring for Complications:</h4><p>Close follow-up is essential to monitor for potential complications such as pancreatic leaks, infections, or changes in blood sugar levels (diabetes).</p></li><li><h4>Emotional and Nutritional Support:</h4><p>DivinHeal provides resources for emotional counseling and connects you with dietitians specializing in post-pancreatectomy nutrition to ensure a holistic recovery. Adjuvant therapies like chemotherapy or radiation often begin several weeks after surgery, further impacting the recovery timeline.</p></li></ul><p>Living with pancreatic cancer long-term requires ongoing surveillance and a commitment to a healthy lifestyle. DivinHeal is here to support you every step of the way, connecting you to post-operative care and follow-up specialists.</p>

oral cancer surgery
Treatment Price
$3000.00 USDOral cancer surgery aims to surgically remove malignant tumors from the oral cavity. This can involve excising the tumor, margins, and potentially affected lymph nodes. Advanced techniques focus on preserving oral function and aesthetics, often incorporating reconstructive procedures to ensure the best possible post-operative quality of life.
Oral cancer surgery aims to surgically remove malignant tumors from the oral cavity. This can involve excising the tumor, margins, and potentially affected lymph nodes. Advanced techniques focus on preserving oral function and aesthetics, often incorporating reconstructive procedures to ensure the best possible post-operative quality of life.
Treatment Overview
Oral cancer surgery aims to surgically remove malignant tumors from the oral cavity. This can involve excising the tumor, margins, and potentially affected lymph nodes. Advanced techniques focus on preserving oral function and aesthetics, often incorporating reconstructive procedures to ensure the best possible post-operative quality of life.
Procedures
Oral cancer surgery typically begins with meticulous pre-operative planning, including imaging and tumor mapping. Under general anesthesia, an incision is made, often in the neck or inside the mouth, to access the tumor. The surgeon then carefully excises the cancerous tissue along with a margin of healthy surrounding tissue to ensure complete removal. If lymph node involvement is suspected or confirmed, a neck dissection is performed to remove affected lymph nodes. For larger resections, reconstructive surgery, often involving microvascular free flaps (transferring tissue with its blood supply from another part of the body), is undertaken to restore function and aesthetics. Finally, the surgical sites are closed.
Benefits
<h2>Benefits of Oral Cancer Surgery</h2><ul><li><h3>Definitive Cancer Removal</h3><p>Surgical excision offers the most direct and often curative approach to remove cancerous tumors, especially in early stages, providing a high probability of disease eradication.</p></li><li><h3>Improved Prognosis</h3><p>Early and effective surgical intervention significantly improves long-term survival rates and reduces the risk of recurrence.</p></li><li><h3>Functional Preservation and Restoration</h3><p>With advanced reconstructive techniques, including microvascular free flap surgery, surgeons can meticulously rebuild removed tissues, preserving vital functions like speaking, swallowing, and breathing, and restoring facial aesthetics.</p></li><li><h3>Reduced Need for Adjunctive Therapies</h3><p>In certain cases, successful surgery may reduce the need for extensive chemotherapy or radiation therapy, minimizing associated side effects.</p></li><li><h3>Enhanced Quality of Life</h3><p>By eradicating the cancer and restoring function, oral cancer surgery helps patients return to a better quality of life, allowing them to eat, speak, and socialize more comfortably.</p></li></ul>
Recovery Information
<h2>Recovery After Oral Cancer Surgery</h2><h3>Immediate Post-Operative Period</h3><p>Following oral cancer surgery, patients typically spend several days in the hospital, depending on the extent of the surgery and any reconstructive procedures. Initial recovery involves pain management, wound care, and monitoring for complications. A feeding tube might be temporarily used if swallowing is difficult.</p><h3>Mid-Term Recovery (Weeks 1-6)</h3><p>During the first few weeks at home, patients will gradually resume normal activities. Diet may be restricted to soft foods, and speech and swallowing therapy often begins to help regain function. Physical therapy may be recommended, especially for neck dissection. DivinHeal offers access to comprehensive rehabilitation services to aid in this critical phase.</p><h3>Long-Term Recovery and Follow-up</h3><p>Full recovery can take several months. Regular follow-up appointments with the surgeon and oncologist are crucial to monitor for recurrence and manage any long-term side effects. Emotional support and counseling are also vital for overall well-being. DivinHeal ensures continuous support, connecting patients with therapists and support groups for a holistic recovery journey.</p>

stomach cancer surgery
Treatment Price
$6000.00 USDOverview of Stomach Cancer Treatment
Stomach cancer treatment focuses on eradicating cancerous cells, managing symptoms, and improving patient prognosis. Surgical interventions, ranging from partial to total gastrectomy, are central to this. DivinHeal connects patients with leading oncological surgeons and state-of-the-art facilities specializing in advanced stomach cancer care, ensuring a holistic approach that includes pre-operative assessment, precise surgical techniques, and comprehensive post-operative management, all with an emphasis on quality and affordability.
Overview of Stomach Cancer Treatment
Stomach cancer treatment focuses on eradicating cancerous cells, managing symptoms, and improving patient prognosis. Surgical interventions, ranging from partial to total gastrectomy, are central to this. DivinHeal connects patients with leading oncological surgeons and state-of-the-art facilities specializing in advanced stomach cancer care, ensuring a holistic approach that includes pre-operative assessment, precise surgical techniques, and comprehensive post-operative management, all with an emphasis on quality and affordability.
Treatment Overview
<h2>Overview of Stomach Cancer Treatment</h2><p>Stomach cancer treatment focuses on eradicating cancerous cells, managing symptoms, and improving patient prognosis. Surgical interventions, ranging from partial to total gastrectomy, are central to this. DivinHeal connects patients with leading oncological surgeons and state-of-the-art facilities specializing in advanced stomach cancer care, ensuring a holistic approach that includes pre-operative assessment, precise surgical techniques, and comprehensive post-operative management, all with an emphasis on quality and affordability.</p>
Procedures
Stomach cancer surgery, primarily gastrectomy, involves removing part or all of the stomach. The procedure begins with general anesthesia. The surgeon makes an incision (either open laparotomy or several small incisions for laparoscopic/robotic surgery). The cancerous portion of the stomach is identified and carefully resected, along with surrounding lymph nodes (lymphadenectomy), which is critical for staging and removing microscopic spread. For a partial gastrectomy, the remaining stomach is reconnected to the small intestine. For a total gastrectomy, the esophagus is directly connected to the small intestine (esophagojejunostomy). Drains may be placed to remove fluid, and a feeding tube might be inserted. The incisions are then closed. The removed tissue is sent for pathological examination to confirm clear margins and determine the cancer's stage.
Benefits
<h2>Benefits of Stomach Cancer Surgery</h2><ul><li><h3>Potential for Cure</h3><p>For early and localized stomach cancer, surgery offers the best chance for complete eradication and long-term survival.</p></li><li><h3>Symptom Relief</h3><p>Surgery can alleviate debilitating symptoms such as obstruction, bleeding, pain, and difficulty eating, significantly improving quality of life, even in advanced stages.</p></li><li><h3>Improved Prognosis</h3><p>When successful, especially when combined with adjuvant therapies, stomach cancer surgery can significantly extend life expectancy and improve overall prognosis.</p></li><li><h3>Accurate Staging</h3><p>Surgical removal of the tumor and lymph nodes allows for precise pathological staging, which guides subsequent treatment decisions.</p></li><li><h3>Access to Advanced Techniques</h3><p>With DivinHeal, patients can access hospitals offering minimally invasive (laparoscopic/robotic) stomach cancer surgery, leading to smaller incisions, less pain, and faster recovery.</p></li></ul>
Recovery Information
<h2>Recovery After Stomach Cancer Surgery</h2><ul><li><h3>Immediate Post-Operative Period (1-2 weeks)</h3><p>Patients typically stay in the hospital for 7-14 days. Initial recovery involves pain management, monitoring for complications, and gradual reintroduction of liquids and soft foods. Nutritional support, often via a feeding tube initially, is crucial.</p></li><li><h3>Medium-Term Recovery (1-3 months)</h3><p>Once home, patients will need to adhere to a strict post-gastrectomy diet, eating small, frequent meals and avoiding certain foods. Fatigue is common. Physical activity will be gradually increased. Follow-up appointments with the surgeon and nutritionist are essential.</p></li><li><h3>Long-Term Recovery & Lifestyle Adjustments</h3><p>Living without a full stomach requires permanent dietary changes to prevent 'dumping syndrome' and ensure adequate nutrient absorption. Supplements (e.g., B12) may be necessary. Emotional counseling and support groups can aid psychological recovery. Most patients can return to normal activities, including work, within 3-6 months, though full recovery can take up to a year.</p></li></ul>

colon cancer surgery
Treatment Price
$6000.00 USDColon cancer surgery involves the surgical removal of a portion of the colon affected by cancerous cells, often along with adjacent lymph nodes. The main goal is to eradicate the tumor, achieve clear margins, and prevent the spread of the disease. Techniques range from open colectomy to minimally invasive laparoscopic or robotic-assisted procedures, tailored to the cancer's stage and location. DivinHeal connects patients with world-class colorectal surgeons and advanced oncology centers offering these precise and effective treatments.
Colon cancer surgery involves the surgical removal of a portion of the colon affected by cancerous cells, often along with adjacent lymph nodes. The main goal is to eradicate the tumor, achieve clear margins, and prevent the spread of the disease. Techniques range from open colectomy to minimally invasive laparoscopic or robotic-assisted procedures, tailored to the cancer's stage and location. DivinHeal connects patients with world-class colorectal surgeons and advanced oncology centers offering these precise and effective treatments.
Treatment Overview
Colon cancer surgery involves the surgical removal of a portion of the colon affected by cancerous cells, often along with adjacent lymph nodes. The main goal is to eradicate the tumor, achieve clear margins, and prevent the spread of the disease. Techniques range from open colectomy to minimally invasive laparoscopic or robotic-assisted procedures, tailored to the cancer's stage and location. DivinHeal connects patients with world-class colorectal surgeons and advanced oncology centers offering these precise and effective treatments.
Procedures
Colon cancer surgery typically involves several key steps: 1. **Pre-operative Preparation:** Patients undergo detailed evaluations, including blood tests, imaging scans, and bowel preparation (cleansing the colon) using laxatives and a clear liquid diet for a few days before surgery. 2. **Anesthesia:** General anesthesia is administered, ensuring the patient is completely unconscious and pain-free throughout the procedure. 3. **Incision:** For open surgery, a single long incision is made in the abdomen. For laparoscopic or robotic surgery, several small incisions (keyhole surgery) are made to insert a camera and specialized instruments. 4. **Identification and Mobilization:** The surgeon identifies the cancerous section of the colon and carefully mobilizes it from surrounding tissues and organs. 5. **Resection:** The segment of the colon containing the tumor, along with a margin of healthy tissue on either side, is surgically removed. Nearby lymph nodes are also dissected and sent for pathological examination. 6. **Anastomosis (Reconnection):** In most cases, the remaining healthy ends of the colon are reconnected (anastomosis) using staples or sutures, restoring the continuity of the digestive tract. 7. **Ostomy Creation (if necessary):** If immediate reconnection is not safe or feasible, a colostomy or ileostomy may be performed. This involves bringing a part of the intestine through an opening (stoma) in the abdominal wall, allowing waste to collect in an external bag. This can be temporary or permanent. 8. **Closure:** The surgical incisions are closed with sutures or staples. A drain might be placed temporarily to remove excess fluid. Post-surgery, the resected tissue is sent to a pathologist for detailed examination to confirm the diagnosis, determine the cancer stage, and evaluate the surgical margins, which guides further treatment decisions.
Benefits
<h2>Benefits of Colon Cancer Surgery</h2><ul><li><h3>Curative Potential</h3><p>For early-stage colon cancer, surgery is often curative, offering the best chance for complete eradication of the disease and a long-term, cancer-free life. It is the primary treatment for localized tumors.</p></li><li><h3>Prevention of Cancer Spread</h3><p>By removing the primary tumor and surrounding lymph nodes, surgery significantly reduces the risk of cancer metastasizing to distant organs, thereby improving overall prognosis.</p></li><li><h3>Symptom Relief and Improved Quality of Life</h3><p>Surgery can alleviate symptoms caused by the tumor, such as bowel obstruction, bleeding, pain, and discomfort, leading to a significant improvement in the patient's quality of life.</p></li><li><h3>Accurate Staging and Personalized Treatment</h3><p>The pathological examination of the resected tissue and lymph nodes provides crucial information for accurate cancer staging. This allows for a more precise and personalized adjuvant (post-surgery) treatment plan, optimizing outcomes.</p></li><li><h3>Access to Advanced Techniques</h3><p>With DivinHeal, patients gain access to hospitals offering advanced surgical techniques like laparoscopic and robotic-assisted colectomy, which often result in smaller incisions, less pain, shorter hospital stays, and faster colon cancer surgery recovery time.</p></li><li><h3>Long-Term Surveillance and Support</h3><p>Successful colon cancer surgery is followed by a structured surveillance program, including regular imaging and blood tests, to monitor for recurrence. DivinHeal ensures continued support through this crucial long-term phase.</p></li></ul>
Recovery Information
<h2>Colon Cancer Surgery Recovery Time and Tips</h2><ul><li><h3>Immediate Post-Operative Period (Hospital Stay: 5-10 days)</h3><p>After colon cancer surgery, patients typically spend 1-2 days in an intensive care unit (ICU) or high-dependency unit, followed by transfer to a regular ward. Pain management, fluid balance, and monitoring for complications are key. Early mobilization (walking) is encouraged to prevent blood clots and aid bowel function. Diet will gradually progress from liquids to soft foods. If an ostomy was created, stoma care education will begin.</p></li><li><h3>Early Recovery (First 2-4 Weeks Post-Discharge)</h3><p>Upon discharge, patients should continue to walk regularly and avoid heavy lifting or strenuous activities. Incision care is crucial to prevent infection. Bowel habits will gradually normalize, though changes in frequency or consistency are common. A high-fiber, easily digestible diet is often recommended. Fatigue is common and rest is important. Follow-up appointments with the surgeon are scheduled to monitor healing.</p></li><li><h3>Intermediate Recovery (1-3 Months Post-Surgery)</h3><p>Most patients can gradually return to light activities and work, depending on their recovery pace and the demands of their job. Full energy levels may take several weeks to months to return. If chemotherapy is required, it often begins during this period. Physical therapy or rehabilitation may be recommended to regain strength and mobility. Dietary adjustments for long-term comfort may be explored with a nutritionist.</p></li><li><h3>Long-Term Recovery and Surveillance</h3><p>Full recovery can take 3-6 months or longer. Regular follow-up with your oncologist and surgeon is essential, including blood tests (e.g., CEA levels), colonoscopies, and imaging scans, to monitor for any signs of recurrence. Emotional support and counseling can be beneficial throughout the recovery process. DivinHeal's care coordinators provide ongoing assistance for all follow-up care and lifestyle adjustments.</p></li></ul>

PET-CT Guided Cancer Staging Package
Treatment Price
$800.00 USDThe PET-CT Guided Cancer Staging Package provides a comprehensive assessment of cancer location, size, and metabolic activity. This advanced imaging technique helps oncologists accurately stage cancer, detect metastases, assess treatment response, and identify cancer recurrence, ensuring a personalized and effective treatment strategy. It integrates state-of-the-art technology with expert radiological interpretation.
The PET-CT Guided Cancer Staging Package provides a comprehensive assessment of cancer location, size, and metabolic activity. This advanced imaging technique helps oncologists accurately stage cancer, detect metastases, assess treatment response, and identify cancer recurrence, ensuring a personalized and effective treatment strategy. It integrates state-of-the-art technology with expert radiological interpretation.
Treatment Overview
The PET-CT Guided Cancer Staging Package provides a comprehensive assessment of cancer location, size, and metabolic activity. This advanced imaging technique helps oncologists accurately stage cancer, detect metastases, assess treatment response, and identify cancer recurrence, ensuring a personalized and effective treatment strategy. It integrates state-of-the-art technology with expert radiological interpretation.
Procedures
The PET-CT Guided Cancer Staging Package involves several steps. First, the patient receives an intravenous injection of a small amount of radioactive tracer, typically fluorodeoxyglucose (FDG). This tracer travels through the bloodstream and accumulates in cells with high metabolic activity, such as cancer cells. After a resting period (usually 60-90 minutes) to allow the tracer to distribute, the patient lies on a comfortable table that slides into the PET-CT scanner. The scanner then captures both PET and CT images sequentially, which are then combined to create highly detailed, 3D images. The entire scanning process usually takes 20-45 minutes. The images are then reviewed by a specialist physician who prepares a comprehensive report.
Benefits
<h2>Benefits of PET-CT Guided Cancer Staging</h2><ul><li><h3>Enhanced Accuracy</h3><p>Combines metabolic (PET) and anatomical (CT) imaging for superior precision in detecting cancer cells and their exact location, even small lesions.</p></li><li><h3>Comprehensive Staging</h3><p>Provides a whole-body scan, allowing for the detection of primary tumors, lymph node involvement, and distant metastases in a single examination.</p></li><li><h3>Optimal Treatment Planning</h3><p>Critical for guiding oncologists in determining the most effective treatment strategy, whether it's surgery, chemotherapy, radiation, or targeted therapies.</p></li><li><h3>Monitoring Treatment Response</h3><p>Can assess how well a patient is responding to ongoing cancer treatment by detecting changes in metabolic activity of tumor cells.</p></li><li><h3>Recurrence Detection</h3><p>Highly effective in identifying cancer recurrence early, often before it's visible on other imaging modalities.</p></li><li><h3>Non-Invasive Procedure</h3><p>A safe, generally well-tolerated outpatient procedure with minimal risks.</p></li></ul>
Recovery Information
<h2>Recovery and What to Expect After PET-CT Staging</h2><p>Recovery from a PET-CT Guided Cancer Staging Package is minimal, as it is a non-invasive diagnostic procedure. Patients can typically resume their normal activities immediately after the scan. You will be advised to drink plenty of fluids to help flush the radioactive tracer from your system.</p><ul><li><h3>Immediate Post-Scan</h3><p>No downtime is required. You may feel a slight residue from the tracer, which dissipates quickly.</p></li><li><h3>Results & Follow-up</h3><p>Radiologists and nuclear medicine specialists will interpret your scans, and a detailed report will be generated, usually within 24-48 hours. DivinHeal's care coordinators will facilitate sharing these results with your oncologist and scheduling follow-up consultations to discuss the staging and next steps in your cancer treatment journey.</p></li><li><h3>Emotional Support</h3><p>Receiving a cancer staging report can be emotionally challenging. DivinHeal provides resources and support networks to help patients and their families navigate this period with empathy and understanding.</p></li></ul>

head and neck cancer surgery
Treatment Price
$5000.00 USDHead and neck cancer surgery aims to completely remove cancerous tissue while preserving function and appearance as much as possible. This complex procedure often requires a multidisciplinary team approach, combining surgical excision with reconstructive techniques. DivinHeal connects you to world-class oncology centers specializing in advanced head and neck cancer treatments, ensuring optimal outcomes and comprehensive care.
Head and neck cancer surgery aims to completely remove cancerous tissue while preserving function and appearance as much as possible. This complex procedure often requires a multidisciplinary team approach, combining surgical excision with reconstructive techniques. DivinHeal connects you to world-class oncology centers specializing in advanced head and neck cancer treatments, ensuring optimal outcomes and comprehensive care.
Treatment Overview
Head and neck cancer surgery aims to completely remove cancerous tissue while preserving function and appearance as much as possible. This complex procedure often requires a multidisciplinary team approach, combining surgical excision with reconstructive techniques. DivinHeal connects you to world-class oncology centers specializing in advanced head and neck cancer treatments, ensuring optimal outcomes and comprehensive care.
Procedures
Head and neck cancer surgery is a complex procedure performed under general anesthesia. The specific steps vary widely based on the tumor's location, size, and type. Typically, an incision is made near the tumor site or in the neck. The surgeon carefully removes the cancerous tissue, ensuring clear margins (no cancer cells at the edges of the removed tissue). Lymph nodes in the neck may also be removed (neck dissection) if there is a risk of spread. For larger tumors, reconstructive surgery may follow immediately, using tissue flaps from other parts of the body (e.g., forearm, leg, chest) to repair the defect, restore function, and improve cosmetic outcomes. Drains are often placed to remove excess fluid, and the incisions are closed with sutures or staples.
Benefits
<h2>Benefits of Head and Neck Cancer Surgery</h2><ul><li><h3>Effective Tumor Removal</h3><p>Surgery offers the best chance for complete removal of localized tumors, especially in early stages.</p></li><li><h3>Improved Prognosis</h3><p>Timely and effective surgery significantly improves survival rates and overall prognosis for many head and neck cancers.</p></li><li><h3>Minimizing Spread</h3><p>Removal of the primary tumor and involved lymph nodes helps prevent the cancer from spreading to other parts of the body.</p></li><li><h3>Preservation of Function</h3><p>Advanced surgical techniques, often combined with reconstructive surgery, aim to preserve vital functions like speech, swallowing, and breathing, and maintain aesthetic appearance.</p></li><li><h3>Reduced Pain and Symptoms</h3><p>Removing the tumor can alleviate pain, difficulty swallowing, breathing issues, and other symptoms caused by the cancer.</p></li><li><h3>Diagnostic Accuracy</h3><p>Pathological examination of the removed tissue provides crucial information about the cancer type, stage, and margin status, guiding further treatment.</p></li></ul>
Recovery Information
<h2>Head and Neck Cancer Surgery Recovery Time and Tips</h2><p>Recovery from head and neck cancer surgery varies significantly depending on the extent of the surgery, the need for reconstruction, and individual patient factors. Generally, the initial hospital stay can range from 3-14 days. Full recovery, including healing of surgical sites, regaining speech and swallowing function, and managing any related therapies, can take several weeks to several months.</p><h3>Key Aspects of Recovery:</h3><ul><li><h3>Pain Management</h3><p>You will receive medication to manage post-operative pain. It's important to communicate your pain levels to your medical team.</p></li><li><h3>Wound Care</h3><p>Careful attention to surgical incisions, including drains and dressings, is crucial to prevent infection and promote healing.</p></li><li><h3>Nutritional Support</h3><p>Difficulty swallowing is common. You may require a feeding tube (nasogastric or gastrostomy) temporarily or for a longer period to ensure adequate nutrition.</p></li><li><h3>Speech and Swallowing Therapy</h3><p>Speech-language pathologists are vital in helping patients regain speech and swallowing abilities through specialized exercises and techniques.</p></li><li><h3>Physical Therapy</h3><p>Exercises may be recommended to improve neck and shoulder mobility, especially after neck dissection.</p></li><li><h3>Emotional and Psychological Support</h3><p>Coping with a head and neck cancer diagnosis and the changes after surgery can be challenging. Counseling and support groups are highly beneficial.</p></li><li><h3>Follow-up Appointments</h3><p>Regular follow-ups with your oncology team are essential to monitor healing, manage side effects, and detect any signs of recurrence.</p></li></ul><h3>Recovery Tips:</h3><ul><li>Follow all post-operative instructions diligently.</li><li>Maintain a soft or liquid diet as advised, ensuring adequate hydration.</li><li>Perform recommended exercises for speech, swallowing, and neck mobility.</li><li>Avoid smoking and alcohol, as these can impede healing and increase recurrence risk.</li><li>Seek support from family, friends, and support groups.</li><li>Be patient with yourself; recovery is a process that takes time.</li></ul>

mastectomy surgery
Treatment Price
$5500.00 USDMastectomy: Goals and Techniques
Mastectomy surgery aims to eradicate cancerous cells from the breast tissue, preventing the spread of the disease. Depending on the cancer's stage, size, and location, as well as patient preferences, different techniques may be employed. These range from total (simple) mastectomy, which removes the entire breast, to modified radical mastectomy, which also includes some lymph nodes. DivinHeal connects you with expert surgeons who utilize advanced techniques for optimal oncological outcomes and offer reconstructive options.
Mastectomy: Goals and Techniques
Mastectomy surgery aims to eradicate cancerous cells from the breast tissue, preventing the spread of the disease. Depending on the cancer's stage, size, and location, as well as patient preferences, different techniques may be employed. These range from total (simple) mastectomy, which removes the entire breast, to modified radical mastectomy, which also includes some lymph nodes. DivinHeal connects you with expert surgeons who utilize advanced techniques for optimal oncological outcomes and offer reconstructive options.
Treatment Overview
<h2>Mastectomy: Goals and Techniques</h2><p>Mastectomy surgery aims to eradicate cancerous cells from the breast tissue, preventing the spread of the disease. Depending on the cancer's stage, size, and location, as well as patient preferences, different techniques may be employed. These range from total (simple) mastectomy, which removes the entire breast, to modified radical mastectomy, which also includes some lymph nodes. DivinHeal connects you with expert surgeons who utilize advanced techniques for optimal oncological outcomes and offer reconstructive options.</p>
Procedures
Mastectomy surgery is performed under general anesthesia. The surgeon makes an incision to remove the breast tissue. The extent of removal depends on the type of mastectomy: a total mastectomy removes the entire breast tissue, nipple, and areola; a skin-sparing mastectomy preserves most of the skin envelope for reconstruction; and a nipple-sparing mastectomy also preserves the nipple-areola complex. If axillary lymph node dissection is indicated, lymph nodes in the armpit are also removed through the same or a separate incision. After tissue removal, drains are typically placed to collect fluid, and the incision is closed with sutures. Breast reconstruction, if chosen, may be performed immediately or as a separate procedure later.
Benefits
<h2>Benefits of Mastectomy Surgery</h2><ul><li><h3>High Efficacy in Cancer Removal</h3><p>Mastectomy provides a highly effective method for removing cancerous breast tissue, significantly reducing the risk of local recurrence, especially for extensive or multi-focal cancers.</p></li><li><h3>Reduced Recurrence Risk</h3><p>For many patients, especially those with aggressive cancers or large tumors, mastectomy offers a lower risk of cancer returning in the treated breast compared to breast-conserving surgery.</p></li><li><h3>Definitive Treatment</h3><p>It can be a definitive treatment for early-stage breast cancer, sometimes eliminating the need for subsequent radiation therapy.</p></li><li><h3>Peace of Mind</h3><p>For some women at high genetic risk of breast cancer, prophylactic mastectomy can offer significant psychological relief by drastically reducing their lifetime risk.</p></li><li><h3>Comprehensive Care Options</h3><p>Mastectomy can be followed by various reconstructive options, allowing patients to regain body image confidence.</p></li></ul>
Recovery Information
<h2>Mastectomy Surgery Recovery: What to Expect</h2><p>Recovery from mastectomy surgery varies among individuals but generally involves several phases:</p><ul><li><h3>Immediate Post-Operative Care (Hospital Stay)</h3><p>Expect drainage tubes to remove excess fluid, pain management, and early mobilization. The hospital stay is typically 1-3 days.</p></li><li><h3>First Few Weeks (Home Recovery)</h3><p>Pain and discomfort are managed with medication. Restrictions on arm movement are common to allow for healing. Drains are usually removed within 1-2 weeks. Swelling and bruising are normal.</p></li><li><h3>Weeks 3-6 (Gradual Return to Activity)</h3><p>Light activities can gradually be resumed. Physical therapy exercises are crucial to restore arm and shoulder mobility and prevent lymphedema. Emotional support is vital during this period.</p></li><li><h3>Long-Term Recovery and Rehabilitation</h3><p>Full recovery can take several months. Ongoing physical therapy, scar care, and monitoring for lymphedema are important. Emotional counseling and support groups can aid psychological adjustment. DivinHeal's network includes specialists for comprehensive rehabilitation.</p></li></ul><p>It is crucial to follow your surgeon's post-operative instructions carefully for optimal healing and to minimize complications.</p>

breast cancer treatment
Treatment Price
$3000.00 USDOverview of Breast Cancer Treatment
Breast cancer treatment aims to eradicate cancer cells, prevent recurrence, and restore quality of life. The approach is highly personalized, guided by the type, stage, and genetic profile of the cancer. Techniques range from minimally invasive surgeries and advanced radiation protocols to innovative targeted therapies and immunotherapies, all supported by compassionate care and robust rehabilitation programs.
Overview of Breast Cancer Treatment
Breast cancer treatment aims to eradicate cancer cells, prevent recurrence, and restore quality of life. The approach is highly personalized, guided by the type, stage, and genetic profile of the cancer. Techniques range from minimally invasive surgeries and advanced radiation protocols to innovative targeted therapies and immunotherapies, all supported by compassionate care and robust rehabilitation programs.
Treatment Overview
<h2>Overview of Breast Cancer Treatment</h2><p>Breast cancer treatment aims to eradicate cancer cells, prevent recurrence, and restore quality of life. The approach is highly personalized, guided by the type, stage, and genetic profile of the cancer. Techniques range from minimally invasive surgeries and advanced radiation protocols to innovative targeted therapies and immunotherapies, all supported by compassionate care and robust rehabilitation programs.</p>
Procedures
Breast cancer treatment procedures involve a carefully planned sequence of interventions. Surgical options include Lumpectomy (breast-conserving surgery, removing only the tumor and a margin of healthy tissue) and Mastectomy (removal of the entire breast, with options for skin-sparing or nipple-sparing techniques). Lymph node assessment, typically via Sentinel Lymph Node Biopsy, determines if cancer has spread to the lymph nodes. Post-surgical care may involve chemotherapy (using drugs to kill cancer cells), radiation therapy (high-energy rays to destroy residual cancer cells), hormone therapy (blocking hormone action for hormone-sensitive cancers), or targeted therapy (drugs specifically attacking cancer cells with certain genetic markers). Reconstruction surgery can be performed immediately or at a later stage.
Benefits
<h2>Benefits of Modern Breast Cancer Treatment</h2><ul><li><h3>High Success Rates</h3><p>With early detection and advanced therapies, the breast cancer treatment success rate is significantly high, offering excellent long-term survival prospects.</p></li><li><h3>Personalized Care</h3><p>Treatment plans are tailored to individual cancer characteristics, maximizing efficacy and minimizing side effects.</p></li><li><h3>Improved Quality of Life</h3><p>Focus on organ preservation (lumpectomy), reconstructive options, and comprehensive support enhances physical and emotional well-being post-treatment.</p></li><li><h3>Access to Advanced Therapies</h3><p>Including targeted therapy, immunotherapy, and proton therapy, providing cutting-edge solutions for various cancer types.</p></li><li><h3>Emotional and Psychological Support</h3><p>Integrated counseling and support groups are often part of the treatment journey, aiding in mental well-being.</p></li></ul>
Recovery Information
<h2>Breast Cancer Treatment Recovery Time and Tips</h2><p>The breast cancer treatment recovery time varies greatly depending on the type of treatment received (surgery, chemotherapy, radiation) and individual factors. DivinHeal provides comprehensive guidance for a smooth and effective recovery.</p><ul><li><h3>Post-Surgical Recovery</h3><p>Initial recovery from breast cancer treatment surgery (lumpectomy or mastectomy) typically takes 3-6 weeks. During this period, patients may experience pain, swelling, and limited arm mobility. Physical therapy, including gentle exercises, is crucial to restore range of motion and prevent lymphedema.</p></li><li><h3>Chemotherapy and Radiation Recovery</h3><p>Recovery from chemotherapy can involve managing side effects like fatigue, nausea, and hair loss, which may persist for weeks or months after treatment. Radiation therapy can cause skin irritation and fatigue, with recovery taking several weeks post-treatment.</p></li><li><h3>Long-Term Wellness & Support</h3><p>Long-term recovery focuses on surveillance, managing late effects of treatment, and adopting a healthy lifestyle. DivinHeal emphasizes regular follow-ups, nutritional guidance, and access to emotional counseling. Support groups play a vital role in navigating the emotional and psychological aspects of life after breast cancer treatment. Active engagement in physical activity, stress management, and a balanced diet are key breast cancer treatment recovery tips for sustained well-being.</p></li></ul>

breast cancer surgery
Treatment Price
$3500.00 USDOverview of Breast Cancer Surgery Treatment
Breast cancer surgery aims to remove the tumor and surrounding affected tissues. The specific surgical approach, whether breast-conserving (lumpectomy) or breast removal (mastectomy), depends on the cancer's stage, size, and patient preferences. Complementary therapies such as chemotherapy, radiation, hormonal therapy, and targeted therapy are frequently used to eradicate residual cancer cells and prevent recurrence. DivinHeal ensures access to cutting-edge diagnostic tools and personalized treatment plans delivered by experienced oncology teams.
Overview of Breast Cancer Surgery Treatment
Breast cancer surgery aims to remove the tumor and surrounding affected tissues. The specific surgical approach, whether breast-conserving (lumpectomy) or breast removal (mastectomy), depends on the cancer's stage, size, and patient preferences. Complementary therapies such as chemotherapy, radiation, hormonal therapy, and targeted therapy are frequently used to eradicate residual cancer cells and prevent recurrence. DivinHeal ensures access to cutting-edge diagnostic tools and personalized treatment plans delivered by experienced oncology teams.
Treatment Overview
<h2>Overview of Breast Cancer Surgery Treatment</h2><p>Breast cancer surgery aims to remove the tumor and surrounding affected tissues. The specific surgical approach, whether breast-conserving (lumpectomy) or breast removal (mastectomy), depends on the cancer's stage, size, and patient preferences. Complementary therapies such as chemotherapy, radiation, hormonal therapy, and targeted therapy are frequently used to eradicate residual cancer cells and prevent recurrence. DivinHeal ensures access to cutting-edge diagnostic tools and personalized treatment plans delivered by experienced oncology teams.</p>
Procedures
Breast cancer surgery involves removing the tumor and, often, surrounding tissue. The specific procedure depends on the cancer's stage and type: 1. **Lumpectomy (Breast-Conserving Surgery):** The surgeon removes only the tumor and a small amount of healthy tissue around it, leaving most of the breast intact. Lymph node biopsy (sentinel lymph node or axillary dissection) may be performed concurrently. 2. **Mastectomy:** * **Total (Simple) Mastectomy:** The entire breast, including the nipple, areola, and skin, is removed. Lymph nodes are usually not removed. * **Modified Radical Mastectomy:** The entire breast, nipple, areola, and some or all of the underarm lymph nodes are removed. The chest wall muscles are spared. * **Skin-Sparing Mastectomy:** Most of the breast skin is preserved, which can be used for breast reconstruction. * **Nipple-Sparing Mastectomy:** Both the breast skin and the nipple/areola are preserved, allowing for a more natural-looking reconstruction. 3. **Lymph Node Biopsy:** * **Sentinel Lymph Node Biopsy:** One or more sentinel lymph nodes (the first lymph nodes to which cancer cells are most likely to spread) are identified and removed to check for cancer. If negative, no further lymph nodes need removal. * **Axillary Lymph Node Dissection:** If cancer cells are found in the sentinel lymph nodes or if the cancer is advanced, several lymph nodes from the armpit (axilla) are removed.
Benefits
<h2>Benefits of Breast Cancer Surgery Treatment in India with DivinHeal</h2><ul><li><h3>Access to World-Class Oncology Expertise</h3><p>Connect with highly experienced top oncologists for breast cancer and surgeons trained in leading global institutions, ensuring superior surgical outcomes and personalized treatment plans.</p></li><li><h3>Significant Cost Savings</h3><p>Benefit from substantially lower breast cancer treatment cost in India, offering savings of up to 70-80% compared to Western countries, making essential care accessible.</p></li><li><h3>Advanced Medical Technology</h3><p>Treatment in JCI/NABH accredited hospitals equipped with the latest diagnostic tools (3D mammography, MRI, PET-CT) and surgical techniques (oncoplastic surgery, minimally invasive options).</p></li><li><h3>High Success Rates</h3><p>India boasts competitive breast cancer success rate thanks to timely diagnosis, advanced treatment protocols, and skilled medical professionals.</p></li><li><h3>Comprehensive, End-to-End Care Coordination</h3><p>DivinHeal provides seamless support, from initial consultation and visa assistance to airport transfers, accommodation, and post-treatment follow-up, ensuring a stress-free journey.</p></li><li><h3>Reduced Waiting Times</h3><p>Avoid long waiting lists common in many countries, allowing for prompt diagnosis and initiation of critical breast cancer surgery treatment.</p></li><li><h3>Emotional and Cultural Support</h3><p>Our dedicated care coordinators offer language assistance and emotional support, ensuring patients and their families feel comfortable and understood throughout their entire journey.</p></li></ul>
Recovery Information
<h2>Breast Cancer Surgery Recovery Time and Tips</h2><p>The breast cancer recovery time varies depending on the type of surgery, the extent of lymph node involvement, and whether other treatments like chemotherapy or radiation are administered. Generally, surgical recovery involves:</p><ul><li><h3>Immediate Post-Operative Period (1-2 weeks)</h3><p>Patients typically experience pain, swelling, and bruising. Drains may be in place for a few days to a week. Gentle arm exercises are often recommended to prevent stiffness and improve range of motion. Adherence to medication schedules and wound care is crucial.</p></li><li><h3>Short-Term Recovery (3-6 weeks)</h3><p>Most patients can resume light activities within 3-6 weeks after breast cancer surgery. Full return to normal activities, including lifting heavy objects, may take longer. Physical therapy is often recommended to address lymphedema prevention and restore full arm and shoulder mobility. Emotional healing through counseling or support groups is also vital.</p></li><li><h3>Long-Term Wellness & Follow-up</h3><p>Ongoing monitoring with regular follow-ups, mammograms, and other scans is essential to ensure long-term well-being and detect any recurrence early. Lifestyle modifications, including a healthy diet, regular exercise, and avoiding alcohol, play a crucial role in maintaining health after breast cancer treatment. DivinHeal provides guidance on navigating this extended phase, connecting you with support resources and specialists for comprehensive rehabilitation and emotional support.</p></li></ul>

surgical oncology
Treatment Price
$4500.00 USDGoals and Techniques of Surgical Oncology
The primary goals of surgical oncology include:
- Tumor Excision: Complete removal of the cancerous tumor and a margin of healthy tissue to ensure clear margins.
- Staging: Determining the extent of the cancer and if it has spread, guiding further treatment decisions.
- Debulking: Removing as much of a large tumor as possible to improve the effectiveness of other therapies like chemotherapy or radiation.
- Palliative Care: Alleviating symptoms, such as pain or obstruction, to improve a patient's quality of life.
Techniques range from traditional open surgery to minimally invasive laparoscopic, robotic, and endoscopic approaches, depending on the tumor's location and characteristics.
Goals and Techniques of Surgical Oncology
The primary goals of surgical oncology include:
- Tumor Excision: Complete removal of the cancerous tumor and a margin of healthy tissue to ensure clear margins.
- Staging: Determining the extent of the cancer and if it has spread, guiding further treatment decisions.
- Debulking: Removing as much of a large tumor as possible to improve the effectiveness of other therapies like chemotherapy or radiation.
- Palliative Care: Alleviating symptoms, such as pain or obstruction, to improve a patient's quality of life.
Techniques range from traditional open surgery to minimally invasive laparoscopic, robotic, and endoscopic approaches, depending on the tumor's location and characteristics.
Treatment Overview
<h3>Goals and Techniques of Surgical Oncology</h3><p>The primary goals of surgical oncology include:</p><ul><li><strong>Tumor Excision:</strong> Complete removal of the cancerous tumor and a margin of healthy tissue to ensure clear margins.</li><li><strong>Staging:</strong> Determining the extent of the cancer and if it has spread, guiding further treatment decisions.</li><li><strong>Debulking:</strong> Removing as much of a large tumor as possible to improve the effectiveness of other therapies like chemotherapy or radiation.</li><li><strong>Palliative Care:</strong> Alleviating symptoms, such as pain or obstruction, to improve a patient's quality of life.</li></ul><p>Techniques range from traditional open surgery to minimally invasive laparoscopic, robotic, and endoscopic approaches, depending on the tumor's location and characteristics.</p>
Procedures
Surgical oncology typically involves several stages. First, general anesthesia is administered. The surgeon then makes an incision to access the tumor. The cancerous tissue, along with a margin of healthy surrounding tissue and potentially nearby lymph nodes (e.g., sentinel lymph node biopsy or lymphadenectomy), is carefully excised. Specialized techniques like oncoplastic reconstruction or robotic assistance may be employed. After the tumor is removed, the incision is closed with sutures or staples, and drains may be placed to remove excess fluid. The removed tissue is sent for pathological analysis to confirm the diagnosis and assess surgical margins.
Benefits
<h3>Benefits of Choosing Surgical Oncology and DivinHeal</h3><ul><li><strong>Definitive Treatment:</strong> For many cancers, surgical removal is the most effective method for eradicating the disease, especially in early stages.</li><li><strong>Precise Staging:</strong> Surgery allows for accurate pathological assessment of the tumor and surrounding tissues, which is vital for determining the cancer stage and guiding subsequent treatments.</li><li><strong>Symptom Relief:</strong> Surgical procedures can alleviate pain, obstruction, or other distressing symptoms caused by a tumor, significantly improving quality of life.</li><li><strong>Access to Top Oncologists:</strong> DivinHeal connects you with India's leading surgical oncologists, recognized globally for their expertise and experience.</li><li><strong>Advanced Medical Technology:</strong> Benefit from hospitals equipped with state-of-the-art diagnostic and surgical equipment, including robotic surgery systems.</li><li><strong>Significant Cost Savings:</strong> Experience world-class care at a fraction of the cost compared to Western countries, without compromising on quality.</li><li><strong>Seamless Care Coordination:</strong> Our AI-driven platform and dedicated care managers handle every aspect of your journey, from appointment booking to post-recovery support.</li><li><strong>High Success Rates:</strong> India's hospitals boast impressive success rates for complex surgical oncology procedures, matching global standards.</li></ul>
Recovery Information
<h3>Surgical Oncology Recovery Time and Tips</h3><p>Recovery from surgical oncology varies depending on the type of surgery, extent of the cancer, and individual patient factors. Generally, patients can expect:</p><ul><li><strong>Initial Hospital Stay:</strong> Typically 5-10 days for major procedures, where pain management, wound care, and early mobilization are prioritized.</li><li><strong>Acute Recovery (Weeks 1-4):</strong> During this period, rest is crucial. Patients may experience fatigue, discomfort, and limitations in physical activity. Wound healing is a primary focus, and drains or stitches may be removed.</li><li><strong>Intermediate Recovery (Months 1-3):</strong> Gradual return to normal activities. Physical therapy or rehabilitation might be recommended to regain strength, flexibility, and function. Nutritional support is often vital.</li><li><strong>Long-Term Follow-up:</strong> Regular check-ups with your oncology team are essential to monitor recovery, screen for recurrence, and manage any long-term side effects. Emotional and psychological support through counseling can also be highly beneficial.</li></ul><h3>Tips for a Smooth Recovery:</h3><ul><li><strong>Follow Medical Advice:</strong> Adhere strictly to your surgeon's and care team's instructions regarding medications, wound care, and activity levels.</li><li><strong>Prioritize Nutrition:</strong> Maintain a balanced diet rich in protein to aid healing and boost energy.</li><li><strong>Stay Hydrated:</strong> Drink plenty of fluids to support overall recovery.</li><li><strong>Gradual Activity:</strong> Slowly increase your activity as advised by your doctor; avoid strenuous exercise too soon.</li><li><strong>Emotional Support:</strong> Connect with support groups, family, or professional counselors to cope with the emotional challenges of cancer recovery.</li><li><strong>Manage Pain:</strong> Do not hesitate to communicate your pain levels to your medical team to ensure effective management.</li></ul>

cancer surgery
Treatment Price
$3000.00 USDGoals and Techniques of Cancer Surgery
Primary Goals of Cancer Surgery
- Curative Resection: Complete removal of the tumor and a margin of healthy tissue to eradicate cancer.
- Debulking: Removing as much of the tumor as possible to improve the effectiveness of subsequent treatments like chemotherapy or radiation.
- Palliative Care: Alleviating pain, obstruction, or other symptoms to improve quality of life when a cure is not possible.
Common Surgical Techniques
Modern cancer surgery utilizes various techniques, from traditional open surgery to minimally invasive approaches. DivinHeal connects you with hospitals proficient in advanced methods such as laparoscopic, robotic, and reconstructive surgeries, ensuring precise treatment and faster recovery.
Goals and Techniques of Cancer Surgery
Primary Goals of Cancer Surgery
- Curative Resection: Complete removal of the tumor and a margin of healthy tissue to eradicate cancer.
- Debulking: Removing as much of the tumor as possible to improve the effectiveness of subsequent treatments like chemotherapy or radiation.
- Palliative Care: Alleviating pain, obstruction, or other symptoms to improve quality of life when a cure is not possible.
Common Surgical Techniques
Modern cancer surgery utilizes various techniques, from traditional open surgery to minimally invasive approaches. DivinHeal connects you with hospitals proficient in advanced methods such as laparoscopic, robotic, and reconstructive surgeries, ensuring precise treatment and faster recovery.
Treatment Overview
<h2>Goals and Techniques of Cancer Surgery</h2><h3>Primary Goals of Cancer Surgery</h3><ul><li><strong>Curative Resection:</strong> Complete removal of the tumor and a margin of healthy tissue to eradicate cancer.</li><li><strong>Debulking:</strong> Removing as much of the tumor as possible to improve the effectiveness of subsequent treatments like chemotherapy or radiation.</li><li><strong>Palliative Care:</strong> Alleviating pain, obstruction, or other symptoms to improve quality of life when a cure is not possible.</li></ul><h3>Common Surgical Techniques</h3><p>Modern cancer surgery utilizes various techniques, from traditional open surgery to minimally invasive approaches. DivinHeal connects you with hospitals proficient in advanced methods such as laparoscopic, robotic, and reconstructive surgeries, ensuring precise treatment and faster recovery.</p>
Procedures
Cancer surgery typically involves several stages. First, the surgeon makes an incision to access the tumor. The cancerous tissue, along with a margin of healthy tissue (known as a clear margin) to ensure all cancer cells are removed, is carefully excised. In some cases, nearby lymph nodes may also be removed (lymphadenectomy) to check for cancer spread. After the tumor removal, the surgical site is closed. Depending on the extent of tissue removed, reconstructive surgery might be performed immediately or in a separate procedure. The removed tissue is then sent to pathology for microscopic examination to confirm the diagnosis, type of cancer, and ensure clear margins.
Benefits
<h2>Benefits of Cancer Surgery</h2><p>Cancer surgery offers numerous advantages for patients, often providing the most direct and effective path to overcoming cancer. Key benefits include:</p><ul><li><strong>High Cure Rates:</strong> Especially for early-stage, localized cancers, surgery can completely remove the tumor, leading to a cure.</li><li><strong>Accurate Staging:</strong> Surgical removal allows for precise pathological examination, accurately determining the cancer's type and stage, which guides future treatment decisions.</li><li><strong>Symptom Relief:</strong> Surgery can alleviate pain, remove obstructions, or address other symptoms caused by a tumor, significantly improving quality of life.</li><li><strong>Combination Therapy Effectiveness:</strong> It often works synergistically with chemotherapy, radiation therapy, and targeted therapies, making overall treatment more effective.</li><li><strong>Reconstruction and Restoration:</strong> Modern surgical techniques include options for reconstruction, helping patients regain function and appearance after tumor removal.</li><li><strong>Hope and Peace of Mind:</strong> For many patients, the physical removal of cancer brings immense psychological relief and renewed hope for a cancer-free future.</li></ul><p>DivinHeal connects you with surgical teams dedicated to maximizing these benefits through advanced techniques and compassionate care.</p>
Recovery Information
<h2>Recovery After Cancer Surgery: A Guide to Healing</h2><h3>Expected Recovery Timeline</h3><p>The recovery period following cancer surgery varies greatly depending on the type and extent of the surgery, the patient's overall health, and potential adjunct therapies. Generally, patients can expect:</p><ul><li><strong>Hospital Stay:</strong> Typically 3-7 days, depending on the complexity of the surgery.</li><li><strong>Initial Healing Phase:</strong> The first 2-4 weeks involve managing pain, monitoring incision sites, and gradually increasing activity.</li><li><strong>Full Recovery:</strong> Most patients require 6 weeks to several months for complete physical recovery and to regain their strength and stamina. Full emotional and psychological recovery can be an ongoing process.</li></ul><h3>Tips for a Smooth Recovery</h3><ul><li><strong>Follow Medical Instructions:</strong> Adhere strictly to your surgeon’s advice regarding wound care, medication, and activity restrictions.</li><li><strong>Pain Management:</strong> Don't hesitate to communicate your pain levels to your medical team. Effective pain control is crucial for comfort and mobility.</li><li><strong>Nutrition:</strong> Maintain a healthy, balanced diet to support healing and energy levels.</li><li><strong>Gentle Activity:</strong> Gradually reintroduce light physical activity as advised by your doctor, which can aid circulation and prevent complications.</li><li><strong>Physical Therapy:</strong> For some surgeries, physical therapy is essential to restore strength, flexibility, and range of motion.</li><li><strong>Emotional Support:</strong> Seek support from family, friends, support groups, or professional counselors to cope with the emotional impact of cancer and surgery. DivinHeal's care coordinators can help connect you with relevant resources.</li><li><strong>Follow-up Appointments:</strong> Regular follow-up with your oncology team is vital for monitoring recovery and detecting any potential recurrence early.</li></ul><p>DivinHeal supports your recovery journey with comprehensive care coordination, ensuring you have access to the resources and guidance needed for optimal healing and return to a fulfilling life.</p>

oncology treatment
Treatment Price
$3000.00 USDBreast Cancer Treatment Overview
The primary goal of breast cancer treatment is to eradicate cancerous cells, prevent metastasis, and manage symptoms. This often combines local treatments like surgery and radiation with systemic therapies such as chemotherapy, hormone therapy, and targeted treatments. DivinHeal facilitates access to cutting-edge diagnostic tools and personalized treatment plans, guided by expert oncologists in India, known for their high success rates and patient-centric approach.
Breast Cancer Treatment Overview
The primary goal of breast cancer treatment is to eradicate cancerous cells, prevent metastasis, and manage symptoms. This often combines local treatments like surgery and radiation with systemic therapies such as chemotherapy, hormone therapy, and targeted treatments. DivinHeal facilitates access to cutting-edge diagnostic tools and personalized treatment plans, guided by expert oncologists in India, known for their high success rates and patient-centric approach.
Treatment Overview
<h2>Breast Cancer Treatment Overview</h2><p>The primary goal of breast cancer treatment is to eradicate cancerous cells, prevent metastasis, and manage symptoms. This often combines local treatments like surgery and radiation with systemic therapies such as chemotherapy, hormone therapy, and targeted treatments. DivinHeal facilitates access to cutting-edge diagnostic tools and personalized treatment plans, guided by expert oncologists in India, known for their high success rates and patient-centric approach.</p>
Procedures
Breast cancer treatment involves a tailored sequence of interventions. Surgical procedures, such as lumpectomy (removing the tumor and a margin of healthy tissue) or mastectomy (removing the entire breast), are often the first step, sometimes accompanied by lymph node biopsy (sentinel lymph node biopsy or axillary lymph node dissection) to check for spread. Following surgery, adjuvant therapies are frequently administered. Chemotherapy, utilizing drugs to kill cancer cells throughout the body, may be given before (neoadjuvant) or after (adjuvant) surgery. Radiation therapy uses high-energy X-rays or other particles to destroy cancer cells in a targeted area, often to the breast and/or lymph nodes after lumpectomy or mastectomy. Hormone therapy, like Tamoxifen or aromatase inhibitors, is used for hormone receptor-positive cancers to block or reduce estrogen's effect. Targeted therapy drugs, such as Trastuzumab for HER2-positive cancer, specifically attack cancer cells with particular characteristics. Immunotherapy, a newer approach, boosts the body's immune system to fight cancer cells.
Benefits
<h2>Benefits of Modern Breast Cancer Treatment & Choosing DivinHeal</h2><ul><li><h3>High Success Rates:</h3><p>Advances in diagnostics and treatment protocols have significantly improved breast cancer survival rates, especially with early detection.</p></li><li><h3>Personalized Care:</h3><p>Treatment plans are tailored to the specific type, stage, and molecular characteristics of the cancer, optimizing efficacy.</p></li><li><h3>Improved Quality of Life:</h3><p>Modern therapies aim to minimize side effects and preserve breast appearance (e.g., oncoplastic surgery, breast reconstruction), enhancing patient well-being.</p></li><li><h3>Access to Innovative Therapies:</h3><p>India's leading oncology centers offer cutting-edge treatments including targeted therapy, immunotherapy, and advanced radiation techniques.</p></li><li><h3>Unmatched Affordability:</h3><p>Receive world-class care at a fraction of the cost compared to Western nations, making life-saving treatment accessible.</p></li><li><h3>Expert Oncologists & Multidisciplinary Teams:</h3><p>DivinHeal connects you with India's top oncologists, surgical teams, radiation specialists, and support staff, ensuring comprehensive and coordinated care.</p></li><li><h3>AI-Driven Transparency & Support:</h3><p>Our platform provides clear cost breakdowns, hospital matching, and end-to-end care coordination, from visa assistance to post-treatment follow-up.</p></li><li><h3>Holistic Patient Experience:</h3><p>Beyond medical treatment, we prioritize emotional and psychological support, rehabilitation, and a comfortable, reassuring environment for patients and their families.</p></li></ul>
Recovery Information
<h2>Breast Cancer Treatment Recovery: Timeline and Tips</h2><p>Recovery from breast cancer treatment is a journey that varies based on the type of treatment received (surgery, chemotherapy, radiation) and individual patient factors. DivinHeal provides comprehensive support throughout this crucial phase.</p><h3>Surgical Recovery:</h3><ul><li><strong>Initial Phase (1-2 weeks):</strong> Patients typically remain in the hospital for a few days post-surgery (e.g., lumpectomy or mastectomy). Pain management is a priority. Drains may be in place.</li><li><strong>Mid-Phase (3-6 weeks):</strong> Full recovery from surgery usually takes 3-6 weeks. During this time, gentle arm and shoulder exercises are crucial to prevent stiffness (e.g., "frozen shoulder"). Physical therapy may be recommended.</li><li><strong>Full Healing (Several months):</strong> Scar tissue maturation and complete physical adjustment can take several months.</li></ul><h3>Recovery from Chemotherapy:</h3><ul><li>Side effects like fatigue, nausea, hair loss, and weakened immune system are common. Recovery between cycles and post-treatment involves managing these side effects and allowing the body to regain strength.</li><li>Nutritional support and adequate rest are vital.</li></ul><h3>Recovery from Radiation Therapy:</h3><ul><li>Skin irritation, fatigue, and breast swelling are common side effects. These usually resolve within weeks to months after therapy concludes.</li><li>Proper skin care is essential.</li></ul><h3>Long-Term Wellness and Support:</h3><ul><li><strong>Follow-up Appointments:</strong> Regular check-ups with your oncologist are crucial for monitoring recovery and detecting any recurrence.</li><li><strong>Physical Therapy & Lymphedema Management:</strong> Essential for regaining strength, mobility, and managing potential lymphedema (swelling of the arm).</li><li><strong>Emotional and Psychological Support:</strong> Cancer diagnosis and treatment can be emotionally challenging. Counseling, support groups, and connection with patient communities are highly beneficial.</li><li><strong>Lifestyle Modifications:</strong> Maintaining a healthy diet, regular exercise, and avoiding alcohol can improve long-term outcomes and overall well-being.</li><li><strong>Reconstructive Options:</strong> For patients undergoing mastectomy, breast reconstruction can be an important part of the emotional and physical recovery, often performed immediately or at a later stage.</li></ul><p>DivinHeal's dedicated care coordinators assist with scheduling rehabilitation, connecting you with support networks, and guiding you through every step of your recovery, ensuring a smooth transition back to a healthy life.</p>

cancer treatment
Treatment Price
$4500.00 USDBreast Cancer Treatment Goals & Techniques
The primary goals of breast cancer treatment include removing cancerous tissue, destroying any remaining cancer cells, and reducing the risk of recurrence or metastasis. Treatment strategies often combine surgery, chemotherapy, radiation therapy, hormone therapy, and targeted therapy. DivinHeal facilitates a personalized treatment plan, leveraging AI-driven insights to match you with the best medical facilities and experts in India, renowned for its advanced yet affordable healthcare.
Breast Cancer Treatment Goals & Techniques
The primary goals of breast cancer treatment include removing cancerous tissue, destroying any remaining cancer cells, and reducing the risk of recurrence or metastasis. Treatment strategies often combine surgery, chemotherapy, radiation therapy, hormone therapy, and targeted therapy. DivinHeal facilitates a personalized treatment plan, leveraging AI-driven insights to match you with the best medical facilities and experts in India, renowned for its advanced yet affordable healthcare.
Treatment Overview
<h2>Breast Cancer Treatment Goals & Techniques</h2><p>The primary goals of breast cancer treatment include removing cancerous tissue, destroying any remaining cancer cells, and reducing the risk of recurrence or metastasis. Treatment strategies often combine surgery, chemotherapy, radiation therapy, hormone therapy, and targeted therapy. DivinHeal facilitates a personalized treatment plan, leveraging AI-driven insights to match you with the best medical facilities and experts in India, renowned for its advanced yet affordable healthcare.</p>
Procedures
The specific procedure details for Breast Cancer treatment vary significantly based on the stage and type of cancer. For surgical interventions, common procedures include Lumpectomy (breast-conserving surgery to remove the tumor and a margin of healthy tissue), Mastectomy (removal of the entire breast), and Lymph Node Biopsy (Sentinel Lymph Node Biopsy or Axillary Lymph Node Dissection to check for cancer spread). These surgeries are performed under general anesthesia. Post-surgery, patients may undergo reconstructive surgery. Non-surgical therapies, such as Chemotherapy, involve intravenous or oral administration of anti-cancer drugs, typically in cycles over several months. Radiation Therapy involves external beam radiation directed at the breast area over several weeks. Hormone and Targeted Therapies involve regular medication intake, often for extended periods, as prescribed by the oncologist. The exact protocol is always personalized by a multidisciplinary oncology team.
Benefits
<h2>Benefits of Modern Breast Cancer Treatment</h2><ul><li><h3>High Success Rates</h3><p>Early detection and advanced treatment modalities have significantly improved survival rates and long-term outcomes for breast cancer patients.</p></li><li><h3>Personalized Care</h3><p>Treatments are tailored based on the specific type, stage, and genetic profile of the cancer, optimizing effectiveness and minimizing side effects.</p></li><li><h3>Improved Quality of Life</h3><p>Minimally invasive surgical techniques, targeted therapies, and reconstructive options help preserve body image and promote a better quality of life post-treatment.</p></li><li><h3>Reduced Recurrence Risk</h3><p>Adjuvant therapies like chemotherapy, radiation, and hormone therapy are highly effective in reducing the risk of cancer recurrence.</p></li><li><h3>Access to Innovations</h3><p>DivinHeal connects you with hospitals offering the latest advancements in breast cancer research and treatment, including novel drug therapies and surgical techniques.</p></li></ul>
Recovery Information
<h2>Breast Cancer Treatment Recovery & Rehabilitation</h2><p>Recovery from breast cancer treatment is a multi-faceted process that varies depending on the specific therapies received. Surgical recovery typically involves 3-6 weeks, during which rest, pain management, and gentle exercises are crucial. Chemotherapy and radiation therapy may cause fatigue and other side effects that require time to resolve.</p><h3>Key Aspects of Recovery:</h3><ul><li><strong>Physical Therapy:</strong> Essential for regaining arm and shoulder mobility, especially after surgery and lymph node dissection, to prevent lymphedema.</li><li><strong>Emotional Support:</strong> Counseling, support groups, and psychological services help patients cope with the emotional and mental challenges of a cancer diagnosis and treatment.</li><li><strong>Nutritional Guidance:</strong> A balanced diet is vital for healing and maintaining strength throughout recovery.</li><li><strong>Lifestyle Modifications:</strong> Regular, moderate exercise and avoiding smoking/excessive alcohol can significantly improve long-term health and reduce recurrence risk.</li><li><strong>Follow-up Care:</strong> Regular check-ups, mammograms, and blood tests are critical for monitoring for any signs of recurrence and managing long-term side effects.</li></ul><p>DivinHeal provides comprehensive post-treatment support, including access to rehabilitation specialists, nutritionists, and psychological counselors, ensuring a holistic recovery journey.</p>

oncologic reconstruction
Treatment Price
$4500.00 USDOverview of Oncologic Reconstruction
Goals and Techniques
- Restoration of Form and Function: The primary goal is to reconstruct defects left by cancer surgery, whether it's breast, head and neck, or extremity reconstruction, to improve patients' physical capabilities.
- Improved Quality of Life: Enhancing physical appearance and functional capabilities helps patients regain confidence, body image, and a return to daily activities.
- Advanced Techniques: Utilizing state-of-the-art techniques such as local flaps, regional flaps, and free tissue transfer (microsurgery) to ensure optimal and durable outcomes.
- Multidisciplinary Approach: Collaborating seamlessly with oncologists, radiation therapists, and other specialists for comprehensive, integrated care throughout the cancer journey.
Overview of Oncologic Reconstruction
Goals and Techniques
- Restoration of Form and Function: The primary goal is to reconstruct defects left by cancer surgery, whether it's breast, head and neck, or extremity reconstruction, to improve patients' physical capabilities.
- Improved Quality of Life: Enhancing physical appearance and functional capabilities helps patients regain confidence, body image, and a return to daily activities.
- Advanced Techniques: Utilizing state-of-the-art techniques such as local flaps, regional flaps, and free tissue transfer (microsurgery) to ensure optimal and durable outcomes.
- Multidisciplinary Approach: Collaborating seamlessly with oncologists, radiation therapists, and other specialists for comprehensive, integrated care throughout the cancer journey.
Treatment Overview
<h2>Overview of Oncologic Reconstruction</h2><h3>Goals and Techniques</h3><ul><li><strong>Restoration of Form and Function:</strong> The primary goal is to reconstruct defects left by cancer surgery, whether it's breast, head and neck, or extremity reconstruction, to improve patients' physical capabilities.</li><li><strong>Improved Quality of Life:</strong> Enhancing physical appearance and functional capabilities helps patients regain confidence, body image, and a return to daily activities.</li><li><strong>Advanced Techniques:</strong> Utilizing state-of-the-art techniques such as local flaps, regional flaps, and free tissue transfer (microsurgery) to ensure optimal and durable outcomes.</li><li><strong>Multidisciplinary Approach:</strong> Collaborating seamlessly with oncologists, radiation therapists, and other specialists for comprehensive, integrated care throughout the cancer journey.</li></ul>
Procedures
Oncologic reconstruction procedures vary significantly based on the defect, requiring highly individualized approaches. However, common steps often include: 1. **Assessment & Planning:** A detailed evaluation of the defect, the patient's overall health, and a thorough discussion of reconstructive options. Advanced imaging (CT, MRI with angiography) is frequently used for precise pre-operative planning, mapping blood vessels, and designing the reconstructive strategy. 2. **Donor Site Selection (for flaps):** If an autologous tissue flap is chosen (e.g., DIEP flap for breast reconstruction, fibula flap for jaw reconstruction), a suitable donor site is identified based on tissue characteristics and minimal donor site morbidity. 3. **Tissue Harvest:** The selected tissue (skin, fat, muscle, and often bone) is carefully harvested, including its precise blood supply, which is critical for free flap transfers. 4. **Defect Preparation:** The area requiring reconstruction is meticulously prepared by the oncology surgeon, ensuring healthy tissue margins and optimizing the recipient site for the new tissue. 5. **Tissue Transfer & Reconnection:** The harvested tissue is moved to the defect. For microvascular free flaps, this involves highly intricate microsurgical techniques to connect the tiny arteries and veins of the flap to recipient vessels at the defect site, re-establishing blood flow. 6. **Shaping & Contouring:** The transferred tissue is meticulously shaped and contoured to restore natural anatomical form and function, often involving significant artistic skill. 7. **Wound Closure:** Both the donor and recipient sites are carefully closed, often with drains to prevent fluid accumulation (seroma). 8. **Post-operative Monitoring:** The reconstructed site, especially free flaps, is closely monitored for blood flow, color, and temperature for several days to ensure flap viability and detect any complications early.
Benefits
<h2>Benefits of Oncologic Reconstruction</h2><p>Undergoing oncologic reconstruction offers profound advantages that significantly enhance a patient's post-cancer quality of life, moving beyond merely addressing the disease to embracing holistic well-being.</p><ul><li><strong>Restoration of Body Image:</strong> Helps patients regain confidence, overcome feelings of disfigurement, and positively impact their psychological state after cancer surgery.</li><li><strong>Improved Physical Function:</strong> Crucially restores mobility, speech, swallowing, continence, and other vital bodily functions, enabling a return to daily activities.</li><li><strong>Enhanced Quality of Life:</strong> Allows patients to re-engage with work, social life, and personal pursuits with greater ease and comfort, fostering a sense of normalcy.</li><li><strong>Reduced Psychological Distress:</strong> Alleviates anxiety, depression, and other emotional challenges associated with body changes after cancer treatment, supporting mental health.</li><li><strong>Customized Solutions:</strong> Tailored reconstructive plans ensure the best possible aesthetic and functional outcomes, designed specifically for individual needs and anatomical requirements.</li><li><strong>Access to Advanced Techniques:</strong> DivinHeal connects you to world-class surgeons skilled in cutting-edge microvascular surgery, advanced flap techniques, implant-based reconstruction, and other innovative options, ensuring a high oncologic reconstruction success rate.</li></ul>
Recovery Information
<h2>Oncologic Reconstruction Recovery Time and Tips</h2><p>Understanding the <strong>oncologic reconstruction recovery time and tips</strong> is crucial for a successful outcome and a smooth transition back to daily life. The duration and specifics of recovery depend largely on the complexity and type of reconstructive surgery performed, as well as individual healing capabilities. While initial healing typically spans a few weeks, full recovery and integration of the reconstructed area can take several months to over a year.</p><h3>Typical Recovery Timeline:</h3><ul><li><strong>Immediate Post-Op (Hospital Stay):</strong> Patients generally stay in the hospital for 5-10 days, particularly for complex microvascular free flap procedures, where close monitoring of blood supply is vital to ensure flap viability.</li><li><strong>Early Recovery (First 3-6 Weeks):</strong> This phase focuses on initial wound healing, pain management, and activity restriction. Swelling, bruising, and discomfort are common. Gentle physical therapy may begin for certain areas.</li><li><strong>Intermediate Recovery (3-6 Months):</strong> Patients gradually increase activity levels and regain strength. Scars begin to mature and soften. Intensive rehabilitation is often essential to restore full function, mobility, and sensation.</li><li><strong>Long-Term Recovery (6 Months - 1 Year+):</strong> Tissues continue to soften and settle, and final aesthetic results become more apparent. Sensation may return slowly over this period. Emotional healing and adaptation to changes in body image are ongoing processes.</li></ul><h4>Essential Recovery Tips for Oncologic Reconstruction:</h4><ul><li><strong>Adhere to Medical Advice:</strong> Strictly follow your surgeon’s instructions for wound care, medication protocols, and activity restrictions to prevent complications and optimize healing.</li><li><strong>Prioritize Rest:</strong> Adequate rest is fundamental for your body to heal and recover energy.</li><li><strong>Nutritional Support:</strong> Maintain a balanced diet rich in protein, vitamins, and minerals. Proper nutrition is vital for tissue repair and overall recovery.</li><li><strong>Physical Therapy & Rehabilitation:</strong> Actively engage in prescribed exercises to restore movement, prevent stiffness, and regain strength in the reconstructed area and donor sites.</li><li><strong>Manage Pain:</strong> Utilize prescribed pain medication as directed to stay comfortable and allow for better rest and mobility.</li><li><strong>Emotional Well-being:</strong> Seek support from family, friends, or professional counselors to process emotional challenges, body image changes, and the journey after cancer treatment.</li><li><strong>Avoid Smoking:</strong> Nicotine severely compromises circulation and healing, significantly increasing the risk of complications like flap failure.</li><li><strong>Gentle Care:</strong> Protect the reconstructed area from trauma, excessive sun exposure, and tight clothing.</li><li><strong>Regular Follow-ups:</strong> Attend all scheduled appointments with your surgical team to monitor progress and address any concerns.</li></ul><p>DivinHeal supports you through every phase, connecting you with rehabilitation specialists and providing ongoing guidance and support for a smooth recovery and optimal long-term results, ensuring you understand your <strong>oncologic reconstruction recovery time and tips</strong>.</p>
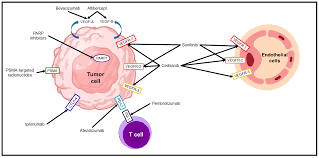
Targeted Molecular Therapy
Treatment Price
$25000.00 USDThis innovative therapy uses drugs designed to target specific molecules crucial for cancer growth and survival, offering a highly effective and often less toxic alternative to traditional chemotherapy.
This innovative therapy uses drugs designed to target specific molecules crucial for cancer growth and survival, offering a highly effective and often less toxic alternative to traditional chemotherapy.
Treatment Overview
<p>This innovative therapy uses drugs designed to target specific molecules crucial for cancer growth and survival, offering a highly effective and often less toxic alternative to traditional chemotherapy.</p>
Procedures
<h3>How procedure is performed</h3><p>Targeted Molecular Therapy is typically administered intravenously as infusions or orally as pills, often in cycles. Treatment begins after extensive diagnostic testing, including genetic profiling of the tumor, to identify specific molecular targets. The chosen targeted drug is then given, precisely interacting with these targets to inhibit cancer cell growth, division, or survival. Regular monitoring, including blood tests and imaging scans, is performed to assess treatment response and manage any potential side effects throughout the course of therapy.</p>
Benefits
<p>Key advantages include greater precision in targeting cancer cells, potentially fewer side effects than conventional chemotherapy, improved survival rates for specific cancers, and a more personalized treatment experience.</p>
Recovery Information
<p>Recovery often involves managing mild to moderate side effects, which are generally less severe than chemotherapy. Patients typically maintain a good quality of life during treatment, with a focus on symptom management and gradual return to daily activities. Targeted Molecular Therapy recovery time and tips are often centered on continuous monitoring and lifestyle adjustments.</p>

cellular therapy cancer
Treatment Price
$30000.00 USDOverview of Cellular Therapy for Cancer
Revolutionizing Cancer Treatment
Cellular therapy involves modifying or enhancing immune cells to precisely target and eliminate cancer. This approach includes CAR T-cell therapy, Tumor-Infiltrating Lymphocyte (TIL) therapy, and Natural Killer (NK) cell therapy, each leveraging distinct mechanisms to fight the disease. The goal is to achieve long-lasting remission with a highly personalized treatment strategy.
Overview of Cellular Therapy for Cancer
Revolutionizing Cancer Treatment
Cellular therapy involves modifying or enhancing immune cells to precisely target and eliminate cancer. This approach includes CAR T-cell therapy, Tumor-Infiltrating Lymphocyte (TIL) therapy, and Natural Killer (NK) cell therapy, each leveraging distinct mechanisms to fight the disease. The goal is to achieve long-lasting remission with a highly personalized treatment strategy.
Treatment Overview
<h2>Overview of Cellular Therapy for Cancer</h2><h3>Revolutionizing Cancer Treatment</h3><p>Cellular therapy involves modifying or enhancing immune cells to precisely target and eliminate cancer. This approach includes CAR T-cell therapy, Tumor-Infiltrating Lymphocyte (TIL) therapy, and Natural Killer (NK) cell therapy, each leveraging distinct mechanisms to fight the disease. The goal is to achieve long-lasting remission with a highly personalized treatment strategy.</p>
Procedures
The core process for cellular therapy for cancer typically involves several key steps: 1. **Patient Selection and Evaluation:** Rigorous assessment of the patient's cancer type, stage, previous treatments, overall health, and suitability for the therapy. 2. **Cell Collection (Leukapheresis):** Blood is drawn from the patient (or a suitable donor) to collect specific immune cells (e.g., T-cells for CAR T-cell therapy) using an apheresis machine, similar to blood donation. 3. **Cell Manufacturing:** The collected cells are sent to a specialized manufacturing facility where they are genetically engineered (e.g., to express CARs) and then expanded into millions or billions of therapeutic cells. This process can take several weeks. 4. **Lymphodepletion Chemotherapy:** Before the modified cells are re-infused, the patient often receives a short course of chemotherapy to reduce existing immune cells, creating a more favorable environment for the infused cells to engraft and expand. 5. **Cell Infusion:** The engineered cellular product is infused intravenously back into the patient, usually in a single session, similar to a blood transfusion. 6. **Post-Infusion Monitoring:** Patients are closely monitored in a specialized hospital setting for several weeks to manage potential acute side effects like Cytokine Release Syndrome (CRS) and neurological toxicities, and to ensure the cells are effectively engrafting and multiplying.
Benefits
<h2>Benefits of Cellular Therapy for Cancer</h2><ul><li><h3>Highly Targeted Approach</h3><p>Cellular therapies are designed to specifically recognize and attack cancer cells, minimizing damage to healthy tissues compared to conventional chemotherapy.</p></li><li><h3>Potential for Durable Remission</h3><p>For eligible patients, especially in certain hematologic malignancies, cellular therapies can lead to long-term, durable remissions, often after other treatments have failed.</p></li><li><h3>Personalized Medicine</h3><p>Many cellular therapies are autologous, meaning they use the patient's own immune cells, making the treatment highly personalized.</p></li><li><h3>Reduced Relapse Risk (in some cases)</h3><p>The persistence of engineered cells in the body can provide ongoing immune surveillance against cancer recurrence.</p></li></ul>
Recovery Information
<h2>Recovery and Life After Cellular Cancer Therapy</h2><h3>Managing Post-Treatment Effects</h3><p>The initial recovery phase after cellular therapy, especially CAR T-cell infusion, requires close medical supervision, typically for 2-4 weeks. Patients are monitored for:</p><ul><li><h4>Cytokine Release Syndrome (CRS)</h4><p>A common side effect that can cause fever, low blood pressure, and organ dysfunction, managed with supportive care and specific medications.</p></li><li><h4>Immune Effector Cell-Associated Neurotoxicity Syndrome (ICANS)</h4><p>Neurological side effects such as confusion, tremors, or seizures, also closely monitored and managed.</p></li><li><h4>Other Side Effects</h4><p>These may include infections, low blood counts (cytopenias), and fatigue.</p></li></ul><h3>Long-Term Wellness</h3><p>Full recovery can take several months. DivinHeal emphasizes a holistic approach to long-term wellness, including:</p><ul><li><h4>Regular Follow-up</h4><p>Essential to monitor for late side effects, relapse, and overall health.</p></li><li><h4>Infection Prevention</h4><p>Guidance on managing immunocompromised states.</p></li><li><h4>Nutritional Support</h4><p>Dietary advice to aid recovery and maintain health.</p></li><li><h4>Emotional and Psychological Counseling</h4><p>Support services to help patients and their families cope with the emotional impact of cancer and intense treatment.</p></li><li><h4>Lifestyle Modifications</h4><p>Recommendations for gentle physical activity and stress reduction to promote healing.</p></li></ul>

car t cell therapy
Treatment Price
$70000.00 USDCAR T-Cell (Chimeric Antigen Receptor T-cell) Therapy involves collecting a patient's T-cells, genetically modifying them in a lab to target cancer cells, multiplying them, and then infusing them back into the patient. This personalized approach offers profound hope, especially for patients with refractory blood cancers, by harnessing the body's own defense system with enhanced precision. DivinHeal ensures access to leading oncologists and state-of-the-art infrastructure for optimal outcomes.
CAR T-Cell (Chimeric Antigen Receptor T-cell) Therapy involves collecting a patient's T-cells, genetically modifying them in a lab to target cancer cells, multiplying them, and then infusing them back into the patient. This personalized approach offers profound hope, especially for patients with refractory blood cancers, by harnessing the body's own defense system with enhanced precision. DivinHeal ensures access to leading oncologists and state-of-the-art infrastructure for optimal outcomes.
Treatment Overview
CAR T-Cell (Chimeric Antigen Receptor T-cell) Therapy involves collecting a patient's T-cells, genetically modifying them in a lab to target cancer cells, multiplying them, and then infusing them back into the patient. This personalized approach offers profound hope, especially for patients with refractory blood cancers, by harnessing the body's own defense system with enhanced precision. DivinHeal ensures access to leading oncologists and state-of-the-art infrastructure for optimal outcomes.
Procedures
CAR T-Cell Therapy is a multi-step, complex process: 1. **Patient Evaluation**: Comprehensive assessment to confirm eligibility, including cancer type, stage, previous treatments, and overall health. 2. **Leukapheresis (T-Cell Collection)**: A procedure similar to blood donation, where blood is drawn, T-cells are separated using a specialized machine, and the remaining blood components are returned to the patient. This typically takes 3-6 hours. 3. **T-Cell Manufacturing**: The collected T-cells are sent to a specialized laboratory. Here, they are genetically engineered using a viral vector (often lentivirus or retrovirus) to express a Chimeric Antigen Receptor (CAR) on their surface. This CAR is designed to specifically recognize a unique antigen found on the surface of the patient's cancer cells (e.g., CD19 for B-cell malignancies, BCMA for multiple myeloma). The engineered T-cells are then expanded to millions in culture. This manufacturing process can take 2-6 weeks. 4. **Lymphodepleting Chemotherapy**: Before the CAR T-cell infusion, the patient receives a short course of chemotherapy (e.g., fludarabine and cyclophosphamide). This 'pre-conditioning' chemotherapy reduces the existing immune cell population, creating space and a more favorable environment for the infused CAR T-cells to expand and persist. 5. **CAR T-Cell Infusion**: The manufactured CAR T-cells are infused back into the patient intravenously, similar to a standard blood transfusion. This is typically an outpatient procedure but requires immediate inpatient monitoring. 6. **Post-Infusion Monitoring & Management**: Patients are closely monitored in an inpatient setting for several weeks (typically 14-30 days) for potential side effects, primarily Cytokine Release Syndrome (CRS) and Immune Effector Cell-Associated Neurotoxicity Syndrome (ICANS). These side effects are managed with supportive care and specific medications. 7. **Follow-up**: Regular follow-up appointments, including blood tests and imaging, are crucial for monitoring treatment response, assessing long-term side effects, and immune reconstitution.
Benefits
<h2>Unlocking New Hope: Benefits of CAR T-Cell Therapy</h2><ul><li><h3>High Response Rates in Refractory Cancers</h3><p>CAR T-Cell Therapy has demonstrated remarkable success rates, leading to complete remissions in a significant proportion of patients with previously untreatable or relapsed/refractory blood cancers, offering a new lease on life where other treatments have failed.</p></li><li><h3>Personalized & Highly Targeted Treatment</h3><p>By engineering a patient's own immune cells, the therapy offers a personalized approach that specifically targets and eliminates cancer cells, minimizing systemic toxicity often associated with conventional chemotherapy.</p></li><li><h3>Potential for Long-Term Remission</h3><p>The modified CAR T-cells can persist in the body, providing ongoing immune surveillance against cancer recurrence, potentially leading to durable, long-term remission for eligible patients.</p></li><li><h3>Reduced Need for Chronic Treatment</h3><p>Successful CAR T-Cell Therapy can eliminate the need for continuous, long-term treatments, significantly improving a patient's quality of life and reducing the burden of chronic disease management.</p></li><li><h3>Access to Leading Global Expertise through DivinHeal</h3><p>DivinHeal connects patients to highly experienced hematologist-oncologists and state-of-the-art facilities specializing in CAR T-Cell Therapy, ensuring access to cutting-edge research and clinical excellence.</p></li><li><h3>Significant Cost Savings in India</h3><p>Patients choosing CAR T-Cell Therapy in India through DivinHeal benefit from world-class medical care at a fraction of the cost compared to Western countries, making this life-saving treatment more accessible and affordable without compromising on quality or safety.</p></li></ul>
Recovery Information
<h2>Navigating Recovery After CAR T-Cell Therapy</h2><h3>Initial Post-Infusion Monitoring (1-4 weeks)</h3><ul><li><p>The immediate period after CAR T-cell infusion involves intensive monitoring in the hospital for potential side effects such as Cytokine Release Syndrome (CRS) and neurotoxicity. Patients are typically hospitalized for 14-30 days.</p></li><li><p>Symptoms like fever, low blood pressure, difficulty breathing (CRS), or confusion, seizures, and language disturbance (neurotoxicity) are closely managed with supportive care and specific medications (e.g., tocilizumab for CRS).</p></li><li><p>Immune cell recovery: Blood counts will be closely monitored as the body recovers from lymphodepleting chemotherapy and adjusts to the new CAR T-cells.</p></li></ul><h3>Intermediate Recovery (1-3 months)</h3><ul><li><p>Patients are usually discharged from the hospital but are required to remain near the treatment facility for several weeks (typically 4-8 weeks post-infusion) for frequent outpatient monitoring and follow-up appointments.</p></li><li><p>Fatigue and weakness are common during this phase. Gradual return to light activities is encouraged.</p></li><li><p>Ongoing monitoring for infections is crucial, as the immune system remains compromised. Prophylactic antibiotics and antivirals may be prescribed.</p></li><li><p>Neurological side effects typically resolve within a few weeks, but close observation continues.</p></li></ul><h3>Long-Term Recovery & Follow-up (3 months and beyond)</h3><ul><li><p>Full immune reconstitution can take several months to a year or more. Vaccinations may need to be repeated.</p></li><li><p>Regular follow-up appointments, including blood tests and imaging, are essential to monitor for relapse and long-term side effects.</p></li><li><p>Psychological and emotional support: Patients and families often benefit from counseling and support groups to cope with the emotional impact of cancer and intense therapy.</p></li><li><p>Lifestyle modifications: A healthy diet, moderate exercise, and stress management are vital for overall well-being. DivinHeal’s care coordinators assist in connecting patients with resources for comprehensive post-treatment support, both medically and emotionally, ensuring a holistic recovery journey.</p></li></ul>

monoclonal antibody therapy
Treatment Price
$12000.00 USDThis advanced therapy involves laboratory-produced antibodies designed to mimic the body's natural immune response. They target specific proteins (antigens) found on the surface of cancer cells or other disease-causing cells, blocking their growth, signaling pathways, or marking them for destruction by the immune system. DivinHeal connects patients with leading oncology centers offering precise diagnosis and tailored Monoclonal Antibody Therapy protocols, ensuring access to cutting-edge care.
This advanced therapy involves laboratory-produced antibodies designed to mimic the body's natural immune response. They target specific proteins (antigens) found on the surface of cancer cells or other disease-causing cells, blocking their growth, signaling pathways, or marking them for destruction by the immune system. DivinHeal connects patients with leading oncology centers offering precise diagnosis and tailored Monoclonal Antibody Therapy protocols, ensuring access to cutting-edge care.
Treatment Overview
This advanced therapy involves laboratory-produced antibodies designed to mimic the body's natural immune response. They target specific proteins (antigens) found on the surface of cancer cells or other disease-causing cells, blocking their growth, signaling pathways, or marking them for destruction by the immune system. DivinHeal connects patients with leading oncology centers offering precise diagnosis and tailored Monoclonal Antibody Therapy protocols, ensuring access to cutting-edge care.
Procedures
Monoclonal Antibody Therapy involves receiving the medication intravenously. After confirming the patient's eligibility through extensive diagnostic tests, including molecular profiling to identify specific targets, the therapy is administered via an IV drip, typically in an outpatient oncology clinic or hospital setting. The infusion duration varies depending on the specific antibody and patient tolerance, usually ranging from 30 minutes to several hours. Patients are closely monitored during and immediately after the infusion for any immediate reactions. The treatment is often given in cycles, with planned breaks between infusions, allowing the body to recover and optimizing therapeutic effect. The exact protocol is tailored to the individual patient and their specific condition.
Benefits
Key benefits of Monoclonal Antibody Therapy include highly targeted action leading to fewer systemic side effects compared to traditional chemotherapy, improved survival rates in specific cancer types, enhanced quality of life during treatment, and the ability to treat conditions previously resistant to therapy. This precision medicine approach offers renewed hope for many patients, extending lifespans and improving clinical outcomes. DivinHeal ensures access to these cutting-edge therapies with a focus on patient safety and successful results.
Recovery Information
Recovery from Monoclonal Antibody Therapy primarily involves managing potential side effects, which are generally milder and more specific than those from conventional chemotherapy. Patients typically experience infusion-related reactions (fever, chills, rash), fatigue, nausea, diarrhea, or skin reactions. These are usually manageable with supportive care. Long-term recovery focuses on continued monitoring for disease progression or recurrence, ongoing supportive care, and lifestyle adjustments to maintain overall well-being. DivinHeal provides resources for post-treatment wellness, including nutritional advice, physical therapy referrals, and access to emotional support groups, ensuring a comprehensive path to recovery and improved quality of life.

immunotherapy for cancer
Treatment Price
$5000.00 USDImmunotherapy aims to stimulate or restore the immune system's natural ability to recognize and destroy cancer cells. Techniques involve immune checkpoint inhibitors, CAR T-cell therapy, monoclonal antibodies, and cancer vaccines. These therapies are tailored to specific cancer types and patient profiles, offering a paradigm shift in oncology towards more personalized and durable responses.
Immunotherapy aims to stimulate or restore the immune system's natural ability to recognize and destroy cancer cells. Techniques involve immune checkpoint inhibitors, CAR T-cell therapy, monoclonal antibodies, and cancer vaccines. These therapies are tailored to specific cancer types and patient profiles, offering a paradigm shift in oncology towards more personalized and durable responses.
Treatment Overview
Immunotherapy aims to stimulate or restore the immune system's natural ability to recognize and destroy cancer cells. Techniques involve immune checkpoint inhibitors, CAR T-cell therapy, monoclonal antibodies, and cancer vaccines. These therapies are tailored to specific cancer types and patient profiles, offering a paradigm shift in oncology towards more personalized and durable responses.
Procedures
Immunotherapy for cancer involves a series of carefully planned steps to ensure optimal patient outcomes. 1. **Comprehensive Evaluation:** The process begins with a thorough medical evaluation, including a review of medical history, current cancer stage, tumor biomarkers (such as PD-L1 status, MSI-H/dMMR status, TMB), and overall health. This determines eligibility and the most appropriate type of immunotherapy. 2. **Treatment Planning:** A multidisciplinary team of oncologists, pathologists, and radiologists collaborates to develop a personalized treatment plan, outlining the specific immunotherapy drug, dosage, and schedule (number of cycles and duration). 3. **Drug Administration:** Most immunotherapies are administered intravenously (IV infusion) in an outpatient clinic setting. The duration of each infusion varies by drug, typically ranging from 30 minutes to a few hours. 4. **Cycles of Treatment:** Immunotherapy is usually given in cycles, with periods of treatment followed by periods of rest. These cycles can span several weeks or months, and the total duration of treatment can range from a few months to a couple of years, depending on the response and type of cancer. 5. **Monitoring and Assessment:** Regular blood tests, imaging scans (CT, MRI, PET scans), and physical examinations are performed throughout the treatment to monitor the tumor's response and assess for any side effects or complications, particularly immune-related adverse events (irAEs). 6. **Side Effect Management:** Should side effects occur, medical teams are prepared to manage them promptly with supportive medications, such as corticosteroids, to mitigate inflammation caused by an overactive immune response. 7. **Follow-up Care:** Upon completion of the treatment course, patients enter a follow-up phase with regular check-ups to monitor for long-term efficacy and potential late-onset side effects.
Benefits
<h2>Key Benefits of Immunotherapy for Cancer</h2><ul><li><strong>Targeted Approach:</strong> Immunotherapy specifically targets cancer cells or boosts the immune system, often sparing healthy cells more effectively than traditional chemotherapy.</li><li><strong>Durable Responses:</strong> For many patients, immunotherapy can lead to long-lasting remission and extended survival, offering a durable response even in advanced cancers.</li><li><strong>Effective for Advanced Cancers:</strong> It has shown remarkable success in treating cancers that have spread or are resistant to other treatments.</li><li><strong>Potential for Less Severe Side Effects:</strong> While side effects can occur, they are often different from chemotherapy and can be manageable, focusing on immune-related adverse events.</li><li><strong>Broad Spectrum of Action:</strong> Applicable to various cancer types, with ongoing research expanding its indications.</li><li><strong>Improved Quality of Life:</strong> By offering effective long-term control and potentially fewer debilitating side effects, patients often experience a better quality of life during and after treatment.</li></ul>
Recovery Information
<h2>Immunotherapy for Cancer Recovery Time and Tips</h2><p>The recovery process after immunotherapy for cancer is highly individualized, depending on the specific type of immunotherapy, the cancer being treated, and the patient's overall health. Unlike surgery or intensive chemotherapy, there isn't typically a single, defined 'recovery time' as immunotherapy often involves cycles over several months.</p><h3>What to Expect During and After Treatment:</h3><ul><li><strong>Managing Side Effects:</strong> The most common 'recovery' aspect involves managing immune-related adverse events (irAEs), which can affect various organs (skin, gut, endocrine glands, lungs, liver, kidneys). These are usually managed with corticosteroids or other immunosuppressants. DivinHeal ensures you have access to expert teams for monitoring and prompt management.</li><li><strong>Fatigue:</strong> This is a common side effect of many cancer treatments, including immunotherapy. Adequate rest, gentle exercise, and good nutrition are vital.</li><li><strong>Ongoing Monitoring:</strong> Regular follow-up appointments, blood tests, and imaging scans are crucial to monitor the treatment's effectiveness and detect any new side effects or recurrence.</li><li><strong>Lifestyle Adjustments:</strong> Maintaining a healthy lifestyle, including a balanced diet, regular physical activity as tolerated, and avoiding smoking/excessive alcohol, supports overall recovery and well-being.</li><li><strong>Emotional and Psychological Support:</strong> A cancer diagnosis and treatment can take a toll emotionally. Seeking counseling, joining support groups, or connecting with fellow survivors can be incredibly beneficial for mental and emotional healing. DivinHeal offers resources for comprehensive care, including psychological support.</li></ul><p>Your DivinHeal care coordinator will provide detailed immunotherapy for cancer recovery time and tips tailored to your specific treatment plan, ensuring you feel supported every step of the way.</p>

targeted therapy cancer
Treatment Price
$8000.00 USDTargeted Therapy: Precision Cancer Care
Goals and Techniques
Precision Attack: Targeted therapy focuses on specific molecular targets (e.g., proteins, genes) critical for cancer cell growth, division, and spread. Unlike chemotherapy, which acts broadly, targeted agents are designed to interfere with these specific pathways.
Diverse Mechanisms: Techniques include small-molecule drugs that block intracellular signals and monoclonal antibodies that block receptors on cell surfaces or deliver toxic substances directly to cancer cells.
Personalized Treatment: Treatment decisions are often guided by comprehensive genomic profiling of the tumor, ensuring the therapy is tailored to the individual patient's cancer biology for maximum efficacy.
Targeted Therapy: Precision Cancer Care
Goals and Techniques
Precision Attack: Targeted therapy focuses on specific molecular targets (e.g., proteins, genes) critical for cancer cell growth, division, and spread. Unlike chemotherapy, which acts broadly, targeted agents are designed to interfere with these specific pathways.
Diverse Mechanisms: Techniques include small-molecule drugs that block intracellular signals and monoclonal antibodies that block receptors on cell surfaces or deliver toxic substances directly to cancer cells.
Personalized Treatment: Treatment decisions are often guided by comprehensive genomic profiling of the tumor, ensuring the therapy is tailored to the individual patient's cancer biology for maximum efficacy.
Treatment Overview
<h2>Targeted Therapy: Precision Cancer Care</h2><h3>Goals and Techniques</h3><ul><li><p><strong>Precision Attack:</strong> Targeted therapy focuses on specific molecular targets (e.g., proteins, genes) critical for cancer cell growth, division, and spread. Unlike chemotherapy, which acts broadly, targeted agents are designed to interfere with these specific pathways.</p></li><li><p><strong>Diverse Mechanisms:</strong> Techniques include small-molecule drugs that block intracellular signals and monoclonal antibodies that block receptors on cell surfaces or deliver toxic substances directly to cancer cells.</p></li><li><p><strong>Personalized Treatment:</strong> Treatment decisions are often guided by comprehensive genomic profiling of the tumor, ensuring the therapy is tailored to the individual patient's cancer biology for maximum efficacy.</p></li></ul>
Procedures
Targeted therapy can be administered orally (pills or capsules) or intravenously (injections or infusions). Oral therapies are taken at home, requiring careful adherence to dosage schedules. Intravenous infusions are typically given in an outpatient clinic or hospital setting, often over a period of 30 minutes to a few hours, at regular intervals (e.g., weekly, bi-weekly, or monthly). The specific administration method and schedule depend on the drug, the type of cancer, and the patient's individual treatment plan.
Benefits
<h2>The Distinct Advantages of Targeted Therapy</h2><h3>Hope for Effective and Tolerable Cancer Care</h3><ul><li><p><strong>Precision and Specificity:</strong> Targets cancer cells more precisely, minimizing damage to healthy cells, leading to fewer and often less severe side effects than traditional chemotherapy.</p></li><li><p><strong>Improved Efficacy:</strong> For patients with specific molecular markers, targeted therapy can be significantly more effective, leading to better response rates, longer progression-free survival, and improved overall survival.</p></li><li><p><strong>Enhanced Quality of Life:</strong> Reduced toxicity often allows patients to maintain a better quality of life during treatment, with less fatigue, nausea, and hair loss.</p></li><li><p><strong>New Treatment Options:</strong> Provides life-extending options for patients with advanced cancers that have specific genetic mutations, including those resistant to other forms of therapy.</p></li><li><p><strong>Personalized Medicine:</strong> Tailored to the individual's tumor biology, ensuring a highly personalized and potentially more successful treatment approach.</p></li><li><p><strong>Potential for Combination Therapy:</strong> Can be effectively combined with chemotherapy, radiation, or immunotherapy to enhance overall treatment outcomes.</p></li></ul>
Recovery Information
<h2>Targeted Therapy Cancer Treatment Recovery & Beyond</h2><h3>Navigating Your Path to Wellness</h3><ul><li><p><strong>Managing Side Effects:</strong> While generally milder than chemotherapy, targeted therapies can have specific side effects (e.g., skin rashes, diarrhea, fatigue, hypertension). DivinHeal's network provides expert care for symptom management, ensuring comfort and treatment adherence.</p></li><li><p><strong>Recovery Timeline:</strong> Recovery is highly individual and depends on the specific drug, dosage, and patient's overall health. Many targeted therapies are administered long-term, and recovery focuses on managing chronic side effects and maintaining quality of life rather than a singular "recovery period." Acute side effects from initial cycles might subside within weeks, but some effects can persist.</p></li><li><p><strong>Ongoing Monitoring:</strong> Regular follow-up appointments, imaging, and blood tests are crucial to monitor treatment response, detect recurrence, and manage long-term side effects. DivinHeal facilitates seamless post-treatment care and communication with your medical team.</p></li><li><p><strong>Nutritional & Lifestyle Support:</strong> Adopting a healthy diet, engaging in light exercise, and avoiding harmful habits can significantly aid recovery and overall well-being. Our holistic approach includes guidance on these aspects.</p></li><li><p><strong>Emotional & Psychological Support:</strong> A cancer journey, even with advanced therapies, can be emotionally challenging. Access to counseling, support groups, and psychological services is vital for mental wellness, and DivinHeal connects patients to these resources.</p></li><li><p><strong>Returning to Daily Activities:</strong> Most patients can maintain a relatively normal routine during targeted therapy. The goal is to integrate treatment into daily life while prioritizing self-care and medical advice.</p></li></ul>

CyberKnife Radiosurgery
Treatment Price
$3500.00 USDCyberKnife Radiosurgery aims to precisely target and ablate tumors or lesions using focused beams of radiation. This innovative technology employs a robotically controlled linear accelerator to deliver radiation with sub-millimeter accuracy, adapting to patient and tumor movement in real-time. The primary goals are tumor eradication or control, pain relief, and functional preservation, offering a non-surgical option with typically fewer treatment sessions.
CyberKnife Radiosurgery aims to precisely target and ablate tumors or lesions using focused beams of radiation. This innovative technology employs a robotically controlled linear accelerator to deliver radiation with sub-millimeter accuracy, adapting to patient and tumor movement in real-time. The primary goals are tumor eradication or control, pain relief, and functional preservation, offering a non-surgical option with typically fewer treatment sessions.
Treatment Overview
CyberKnife Radiosurgery aims to precisely target and ablate tumors or lesions using focused beams of radiation. This innovative technology employs a robotically controlled linear accelerator to deliver radiation with sub-millimeter accuracy, adapting to patient and tumor movement in real-time. The primary goals are tumor eradication or control, pain relief, and functional preservation, offering a non-surgical option with typically fewer treatment sessions.
Procedures
CyberKnife Radiosurgery involves several key steps: 1. **Imaging & Planning:** High-resolution CT, MRI, and PET scans are used to precisely map the tumor's location, shape, and size. A radiation oncologist, with a team of medical physicists, then creates a personalized treatment plan, determining the optimal radiation dose and beam angles. 2. **Patient Preparation:** On treatment day, the patient is positioned comfortably on the treatment couch. A custom-made body mold or head frame may be used for immobilization, though not always necessary with CyberKnife's tracking system. 3. **Treatment Delivery:** The robotic arm, holding the linear accelerator, moves around the patient, delivering hundreds of precisely aimed radiation beams. The system continuously monitors the patient's breathing and movement, making real-time adjustments to ensure the radiation precisely targets the tumor, even as it moves. 4. **Monitoring:** A radiation therapist monitors the treatment from an adjacent control room, ensuring patient comfort and safety. Each session typically lasts 30-90 minutes. Patients usually receive 1 to 5 sessions over several days.
Benefits
<h2>Benefits of CyberKnife Radiosurgery</h2><ul><li><h3>Superior Precision and Accuracy</h3><p>The CyberKnife system delivers radiation with sub-millimeter accuracy, ensuring that the radiation dose is precisely targeted to the tumor while sparing surrounding healthy tissues and critical structures. This minimizes side effects and optimizes treatment outcomes.</p></li><li><h3>Non-Invasive Treatment Option</h3><p>As a non-surgical procedure, CyberKnife eliminates the need for incisions, general anesthesia, and associated surgical risks such as infection, blood loss, and prolonged recovery times. It offers a viable alternative for patients who are not candidates for conventional surgery.</p></li><li><h3>Shorter Treatment Duration</h3><p>Most CyberKnife Radiosurgery treatments are completed in 1 to 5 sessions, significantly fewer than traditional radiation therapy which can require 20-40 sessions. This shortens the overall treatment period, allowing patients to return to their daily lives more quickly.</p></li><li><h3>Real-Time Tumor Tracking</h3><p>Equipped with advanced image guidance, CyberKnife continuously tracks tumor and patient movement (including breathing), making real-time adjustments to maintain precision. This is particularly beneficial for tumors that move with respiration, such as those in the lung or liver.</p></li><li><h3>Minimal Discomfort and Quick Recovery</h3><p>Patients typically experience little to no pain during the treatment sessions. The non-invasive nature and precise targeting lead to fewer and milder side effects, facilitating a faster and smoother recovery compared to conventional surgery or radiation.</p></li><li><h3>Expanded Treatment Possibilities</h3><p>CyberKnife can treat a wide range of tumors throughout the body, including complex cases or those in hard-to-reach areas, and can even be used for re-irradiation in previously treated areas, offering hope where other options are limited.</p></li></ul>
Recovery Information
<h2>CyberKnife Radiosurgery Recovery Time and Tips</h2><p>One of the significant advantages of CyberKnife Radiosurgery is its typically rapid and minimal recovery period. As a non-invasive procedure, most patients can resume their normal activities almost immediately after treatment.</p><ul><li><h3>Immediate Post-Treatment</h3><p>Patients usually leave the hospital or clinic shortly after their CyberKnife session. Some may experience mild fatigue, headache, or nausea, depending on the treated area, but these symptoms are generally transient and manageable with medication.</p></li><li><h3>Short-Term Recovery (Days to Weeks)</h3><p>For most patients, there's no specific recovery period requiring hospitalization or extensive rest. Mild fatigue might persist for a few days to weeks. Your care team will provide specific instructions tailored to your condition and the treated area, including managing any minor side effects and scheduling follow-up appointments.</p></li><li><h3>Long-Term Wellness and Follow-up</h3><p>DivinHeal emphasizes comprehensive post-treatment care, including regular follow-up imaging (e.g., MRI, CT scans) to monitor the tumor's response to treatment. Patients are encouraged to maintain a healthy lifestyle, attend all scheduled appointments, and communicate any new symptoms or concerns to their medical team. Emotional support and lifestyle modifications may also be recommended to support overall well-being.</p></li></ul>

Robotic Cancer Surgery
Treatment Price
$8000.00 USDThe primary goal of Robotic Cancer Surgery is the meticulous removal of cancerous tissue while preserving healthy surrounding organs and functions. Utilizing advanced 3D high-definition visualization and highly dexterous, wristed instruments, surgeons can navigate complex anatomical structures with extreme accuracy. This approach is instrumental in improving oncological efficacy, reducing patient trauma, and accelerating post-operative rehabilitation, setting a new standard for surgical excellence in cancer care.
The primary goal of Robotic Cancer Surgery is the meticulous removal of cancerous tissue while preserving healthy surrounding organs and functions. Utilizing advanced 3D high-definition visualization and highly dexterous, wristed instruments, surgeons can navigate complex anatomical structures with extreme accuracy. This approach is instrumental in improving oncological efficacy, reducing patient trauma, and accelerating post-operative rehabilitation, setting a new standard for surgical excellence in cancer care.
Treatment Overview
The primary goal of Robotic Cancer Surgery is the meticulous removal of cancerous tissue while preserving healthy surrounding organs and functions. Utilizing advanced 3D high-definition visualization and highly dexterous, wristed instruments, surgeons can navigate complex anatomical structures with extreme accuracy. This approach is instrumental in improving oncological efficacy, reducing patient trauma, and accelerating post-operative rehabilitation, setting a new standard for surgical excellence in cancer care.
Procedures
The Robotic Cancer Surgery procedure begins with the patient under general anesthesia. Small incisions (0.5-1.5 cm) are made to insert slender instruments and a high-definition 3D camera. The surgical team then docks the robotic system, connecting its arms to these instruments. The surgeon, seated at a console, manipulates the controls, which translate their hand and wrist movements into precise actions of the robotic instruments inside the body. The surgeon observes the magnified, 3D view to accurately dissect, cut, and remove cancerous tissues. Once the tumor is removed, the instruments are withdrawn, and incisions are closed with sutures or staples.
Benefits
Robotic Cancer Surgery offers numerous advantages: enhanced surgical precision, minimal invasiveness with smaller incisions, reduced blood loss, lower risk of complications, shorter hospital stays, faster recovery, less post-operative pain, and excellent cosmetic outcomes. These benefits contribute to a quicker return to normal life and improved quality of life post-surgery.
Recovery Information
Recovery from Robotic Cancer Surgery is generally quicker and less painful than traditional open surgery. Patients typically stay in the hospital for 3-7 days. Full recovery, including resumption of normal activities, can range from 2-6 weeks depending on the type of cancer, individual health, and extent of the surgery. DivinHeal provides personalized post-operative care plans, including pain management, dietary advice, and rehabilitation support, to ensure a smooth and swift return to health.

Immunotherapy & CAR-T Cell Therapy
Treatment Price
$40000.00 USDOverview of Immunotherapy & CAR-T Cell Therapy
Immunotherapy is a biological treatment that stimulates or restores the body's natural defense mechanisms to fight cancer. CAR-T (Chimeric Antigen Receptor T-cell) Cell Therapy is a specialized form of immunotherapy where a patient's T-cells are genetically modified in a lab to recognize and attack cancer cells, then reinfused into the patient. These therapies offer new hope for various advanced and refractory cancers.
Goals of Immunotherapy & CAR-T Cell Therapy
- To precisely target and eliminate cancer cells with reduced harm to healthy tissue.
- To achieve long-lasting remission or cure for difficult-to-treat cancers.
- To improve overall survival and quality of life.
- To provide viable options when traditional treatments like chemotherapy and radiation therapy have been ineffective.
Overview of Immunotherapy & CAR-T Cell Therapy
Immunotherapy is a biological treatment that stimulates or restores the body's natural defense mechanisms to fight cancer. CAR-T (Chimeric Antigen Receptor T-cell) Cell Therapy is a specialized form of immunotherapy where a patient's T-cells are genetically modified in a lab to recognize and attack cancer cells, then reinfused into the patient. These therapies offer new hope for various advanced and refractory cancers.
Goals of Immunotherapy & CAR-T Cell Therapy
- To precisely target and eliminate cancer cells with reduced harm to healthy tissue.
- To achieve long-lasting remission or cure for difficult-to-treat cancers.
- To improve overall survival and quality of life.
- To provide viable options when traditional treatments like chemotherapy and radiation therapy have been ineffective.
Treatment Overview
<h2>Overview of Immunotherapy & CAR-T Cell Therapy</h2><p>Immunotherapy is a biological treatment that stimulates or restores the body's natural defense mechanisms to fight cancer. CAR-T (Chimeric Antigen Receptor T-cell) Cell Therapy is a specialized form of immunotherapy where a patient's T-cells are genetically modified in a lab to recognize and attack cancer cells, then reinfused into the patient. These therapies offer new hope for various advanced and refractory cancers.</p><h3>Goals of Immunotherapy & CAR-T Cell Therapy</h3><ul><li>To precisely target and eliminate cancer cells with reduced harm to healthy tissue.</li><li>To achieve long-lasting remission or cure for difficult-to-treat cancers.</li><li>To improve overall survival and quality of life.</li><li>To provide viable options when traditional treatments like chemotherapy and radiation therapy have been ineffective.</li></ul>
Procedures
Immunotherapy & CAR-T Cell Therapy procedures vary significantly based on the specific type. Immunotherapy, such as checkpoint inhibitor therapy, typically involves intravenous (IV) infusions administered in an outpatient setting over several cycles. The duration of each infusion can range from 30 minutes to a few hours, with cycles repeated every 2-4 weeks. For CAR-T Cell Therapy, the process is more complex: first, T-cells are collected from the patient's blood (apheresis). These cells are then sent to a specialized laboratory where they are genetically engineered to express Chimeric Antigen Receptors (CARs) that target specific cancer antigens. The modified CAR-T cells are expanded to large numbers and then frozen. Before reinfusion, the patient usually receives a short course of lymphodepleting chemotherapy to prepare their body. Finally, the patient receives a single IV infusion of their engineered CAR-T cells. Patients are closely monitored in the hospital for several weeks post-infusion for potential side effects.
Benefits
<h2>Benefits of Immunotherapy & CAR-T Cell Therapy</h2><p>These advanced cancer treatments offer significant advantages for patients, particularly in cases where traditional therapies have failed or are not suitable.</p><ul><li><h3>Highly Targeted Treatment:</h3> Immunotherapy and CAR-T cells are designed to specifically recognize and attack cancer cells, minimizing damage to healthy tissues, which can lead to fewer severe side effects compared to conventional chemotherapy and radiation therapy.</li><li><h3>Durable Responses:</h3> Many patients experience long-lasting remission or even complete responses, with the immune system potentially developing 'memory' against cancer, offering long-term protection.</li><li><h3>Effective for Advanced Cancers:</h3> These therapies have shown remarkable success in treating advanced or metastatic cancers that were previously considered untreatable.</li><li><h3>Potential for Cure:</h3> For certain hematological malignancies, CAR-T Cell Therapy offers the potential for a curative outcome, especially in relapsed/refractory settings.</li><li><h3>Personalized Approach:</h3> CAR-T Cell Therapy is a highly personalized treatment, using the patient's own immune cells tailored to their specific cancer.</li><li><h3>Improved Quality of Life:</h3> With potentially fewer debilitating side effects and more effective disease control, patients often experience an improved quality of life during and after treatment.</li></ul>
Recovery Information
<h2>Recovery and Life After Immunotherapy & CAR-T Cell Therapy</h2><p>Recovery from Immunotherapy & CAR-T Cell Therapy varies greatly depending on the specific treatment, the cancer type, and individual patient factors. Understanding the Immunotherapy & CAR-T Cell Therapy recovery time and tips is crucial for optimal outcomes.</p><ul><li><h3>Immediate Post-Treatment:</h3> Patients receiving CAR-T therapy typically require an extended hospital stay (often 2-4 weeks) for close monitoring due to potential acute side effects like Cytokine Release Syndrome (CRS) and neurotoxicity. Immunotherapy infusions usually allow for outpatient administration, with less immediate intensive monitoring.</li><li><h3>Short-Term Recovery (Weeks to Months):</h3> Fatigue is a common side effect of both therapies. Patients may experience flu-like symptoms, skin rashes, or digestive issues. Regular follow-up appointments, blood tests, and imaging are crucial to monitor treatment effectiveness and manage side effects. Physical therapy and nutritional support may be recommended.</li><li><h3>Long-Term Wellness:</h3> While many patients return to their normal activities, ongoing monitoring for late-onset side effects is important. Lifestyle modifications, including a healthy diet, regular exercise, and stress management, contribute to long-term well-being. Emotional counseling and support groups can be invaluable for coping with the psychological aspects of cancer recovery. DivinHeal's post-treatment care extends to connecting patients with resources for continued support and guidance.</li></ul>

Proton Therapy
Treatment Price
$25000.00 USDProton Therapy: Precision Cancer Treatment
Proton Therapy utilizes a beam of protons to precisely target and destroy cancer cells. Unlike traditional photon radiation, protons release most of their energy at a specific depth within the tissue (the Bragg Peak), allowing for a highly conformal dose to the tumor while virtually eliminating radiation beyond the target. This makes it particularly beneficial for tumors located near critical structures or for pediatric cancers, where minimizing radiation exposure to developing tissues is paramount. The goal is to maximize tumor control while significantly reducing short-term and long-term side effects, improving patient outcomes and overall well-being.
Proton Therapy: Precision Cancer Treatment
Proton Therapy utilizes a beam of protons to precisely target and destroy cancer cells. Unlike traditional photon radiation, protons release most of their energy at a specific depth within the tissue (the Bragg Peak), allowing for a highly conformal dose to the tumor while virtually eliminating radiation beyond the target. This makes it particularly beneficial for tumors located near critical structures or for pediatric cancers, where minimizing radiation exposure to developing tissues is paramount. The goal is to maximize tumor control while significantly reducing short-term and long-term side effects, improving patient outcomes and overall well-being.
Treatment Overview
<h2>Proton Therapy: Precision Cancer Treatment</h2><p>Proton Therapy utilizes a beam of protons to precisely target and destroy cancer cells. Unlike traditional photon radiation, protons release most of their energy at a specific depth within the tissue (the Bragg Peak), allowing for a highly conformal dose to the tumor while virtually eliminating radiation beyond the target. This makes it particularly beneficial for tumors located near critical structures or for pediatric cancers, where minimizing radiation exposure to developing tissues is paramount. The goal is to maximize tumor control while significantly reducing short-term and long-term side effects, improving patient outcomes and overall well-being.</p>
Procedures
Proton Therapy involves several precise steps: first, a detailed simulation using imaging (CT, MRI) to create a 3D map of the tumor and surrounding anatomy. Next, a personalized treatment plan is developed by a team of specialists, determining the exact dose, energy, and direction of the proton beams. During each treatment session, the patient is carefully positioned on a treatment couch, often using custom immobilization devices to ensure accuracy. The proton beam is then delivered by a gantry that rotates around the patient, precisely targeting the tumor while sparing healthy tissues. The entire process is monitored by highly trained medical staff, ensuring safety and precision at every step.
Benefits
<h2>Key Benefits of Proton Therapy</h2><ul><li><h3>Superior Precision & Tumor Targeting</h3><p>Proton therapy uses the unique "Bragg Peak" phenomenon to deliver radiation precisely to the tumor, minimizing damage to surrounding healthy tissues and critical organs. This precision is particularly beneficial for complex tumors and those located near sensitive areas.</p></li><li><h3>Reduced Side Effects</h3><p>By sparing healthy tissue, proton therapy often leads to fewer short-term and long-term side effects compared to traditional radiation, improving the patient's quality of life during and after treatment. This includes less nausea, fatigue, and lower risk of secondary cancers.</p></li><li><h3>Ideal for Pediatric Cancers</h3><p>Minimizing radiation exposure is paramount for children, whose growing bodies are more susceptible to radiation-induced damage. Proton therapy significantly reduces the risk of developmental issues, cognitive impairments, and secondary cancers in pediatric patients.</p></li><li><h3>Effective for Tumors Near Critical Structures</h3><p>Proton therapy is highly advantageous for treating tumors of the brain, spinal cord, head and neck, eyes, and prostate, where preserving function of adjacent vital organs is crucial.</p></li><li><h3>Lower Risk of Secondary Cancers</h3><p>The reduced exposure of healthy tissue to radiation translates to a lower lifetime risk of developing secondary cancers, a significant concern with conventional radiation therapy, especially for younger patients.</p></li><li><h3>Potential for Higher Dosing</h3><p>In some cases, the precision of proton therapy allows oncologists to deliver higher, more effective radiation doses to the tumor, potentially increasing the chances of tumor control and long-term survival.</p></li></ul>
Recovery Information
<h2>Recovery and Life After Proton Therapy</h2><h3>Immediate Post-Treatment</h3><p>Proton Therapy is typically an outpatient procedure, meaning you can return home after each session. While the treatment itself is painless, patients may experience mild side effects depending on the treated area. These can include fatigue, skin irritation (redness, dryness, peeling) in the treated field, and localized swelling. Most side effects are temporary and gradually resolve weeks to months after the completion of therapy.</p><h3>Managing Side Effects and Long-Term Wellness</h3><p>DivinHeal's care coordinators and medical team will provide comprehensive guidance on managing any side effects. This includes advice on skin care, nutrition, pain management, and activity levels. Regular follow-up appointments with your radiation oncologist are crucial to monitor your recovery, assess treatment effectiveness, and address any long-term concerns. The long-term recovery process focuses on rehabilitation, psychological support, and lifestyle adjustments to ensure optimal health and well-being. Many patients return to their normal daily activities shortly after completing their course of proton therapy, with the benefit of having experienced fewer severe side effects than with conventional radiation.</p><h3>DivinHeal's Continued Support</h3><p>Our commitment extends beyond your treatment completion. We facilitate access to post-treatment care, including rehabilitation specialists, nutritionists, and support groups, ensuring a holistic recovery journey. Our goal is to empower you to regain your strength and live a full, healthy life after Proton Therapy.</p>

HIPEC (Heated Intraperitoneal Chemotherapy)
Treatment Price
$10000.00 USDHIPEC combines comprehensive cytoreductive surgery (CRS) with regional chemotherapy to treat advanced abdominal cancers. The primary goal is to improve survival rates and reduce recurrence by bathing the peritoneal cavity with heated chemotherapy, enhancing drug penetration and efficacy while minimizing systemic side effects. This aggressive approach is reserved for carefully selected patients with peritoneal metastases.
HIPEC combines comprehensive cytoreductive surgery (CRS) with regional chemotherapy to treat advanced abdominal cancers. The primary goal is to improve survival rates and reduce recurrence by bathing the peritoneal cavity with heated chemotherapy, enhancing drug penetration and efficacy while minimizing systemic side effects. This aggressive approach is reserved for carefully selected patients with peritoneal metastases.
Treatment Overview
HIPEC combines comprehensive cytoreductive surgery (CRS) with regional chemotherapy to treat advanced abdominal cancers. The primary goal is to improve survival rates and reduce recurrence by bathing the peritoneal cavity with heated chemotherapy, enhancing drug penetration and efficacy while minimizing systemic side effects. This aggressive approach is reserved for carefully selected patients with peritoneal metastases.
Procedures
HIPEC treatment involves two main phases performed consecutively in a single operation: Cytoreductive Surgery (CRS) and the administration of Heated Intraperitoneal Chemotherapy (HIPEC). First, the surgical oncology team performs an extensive CRS to meticulously remove all visible cancerous tumors and affected tissues from the abdominal cavity. This may include removing parts of organs such as the colon, spleen, or ovaries, aiming for complete macroscopic disease resection. Once all visible cancer is removed, the HIPEC phase begins. A special perfusion circuit is set up to deliver a heated chemotherapy solution (typically Mitomycin C, Oxaliplatin, or Doxorubicin) directly into the patient's abdominal cavity. The solution, heated to approximately 41-42°C, is circulated for 60-120 minutes, allowing the chemotherapy to penetrate and kill microscopic cancer cells that may remain. After the perfusion period, the chemotherapy solution is drained, and the abdomen is closed. This complex procedure requires highly skilled surgical oncologists and a specialized operating room setup.
Benefits
<h2>Benefits of HIPEC Treatment</h2><ul><li><h3>Improved Survival Rates</h3><p>For carefully selected patients with peritoneal carcinomatosis, HIPEC combined with CRS has demonstrated significantly improved overall and disease-free survival compared to traditional treatments, contributing to a higher HIPEC success rate.</p></li><li><h3>Targeted Chemotherapy Delivery</h3><p>Direct administration of chemotherapy into the abdominal cavity ensures high drug concentrations precisely where the cancer is located, minimizing systemic exposure and its associated side effects.</p></li><li><h3>Enhanced Drug Efficacy with Heat</h3><p>The heated chemotherapy solution not only increases drug penetration but also directly kills cancer cells and makes them more sensitive to the chemotherapy agents.</p></li><li><h3>Reduced Recurrence Risk</h3><p>By effectively targeting microscopic cancer cells, HIPEC aims to reduce the risk of cancer recurrence within the peritoneum.</p></li><li><h3>Localized Treatment Approach</h3><p>Offers a regional therapy option for cancers that have spread locally within the abdomen, providing an alternative or adjunct to systemic treatments.</p></li><li><h3>Access to Advanced Care</h3><p>DivinHeal provides access to best hospitals for HIPEC and top oncologists for HIPEC globally, ensuring patients receive cutting-edge treatment with a focus on quality care and patient safety.</p></li></ul>
Recovery Information
<h2>HIPEC Recovery Time and Tips</h2><p>Recovery from HIPEC treatment is a significant process due to the extensive nature of cytoreductive surgery and the effects of intraperitoneal chemotherapy. Patients can expect a hospital stay of approximately 7-14 days, followed by several weeks to months of recuperation at home. DivinHeal provides comprehensive support throughout this crucial period.</p><ul><li><h3>Immediate Post-operative Care</h3><p>Patients are typically monitored in the Intensive Care Unit (ICU) for the first few days, focusing on pain management, fluid balance, and monitoring for complications. Early mobilization is encouraged.</p></li><li><h3>Hospital Recovery</h3><p>As recovery progresses, patients move to a regular ward. Focus areas include regaining strength, managing discomfort, wound care, and reintroducing oral nutrition. Physical therapy may begin to help with mobility and strength.</p></li><li><h3>Home Recovery (Weeks to Months)</h3><p>Full recovery can take 2-6 months. Key aspects include:</p><ul><li><strong>Nutritional Support:</strong> Maintaining a healthy diet is crucial. Some patients may require temporary feeding tubes or dietary modifications.</li><li><strong>Physical Therapy:</strong> Essential for restoring strength, flexibility, and endurance, aiding in a smoother HIPEC recovery time and tips implementation.</li><li><strong>Emotional and Psychological Support:</strong> Dealing with a major surgery and cancer diagnosis can be challenging. Counseling and support groups are invaluable.</li><li><strong>Activity Restrictions:</strong> Avoiding heavy lifting and strenuous activities for several weeks is important to allow internal healing.</li><li><strong>Follow-up Appointments:</strong> Regular visits with your oncology team are essential to monitor recovery and detect any signs of recurrence.</li></ul><p>DivinHeal's dedicated care coordinators offer continuous guidance, connecting patients with post-treatment support, including rehabilitation services and psychological counseling, ensuring a holistic recovery journey. We aim to provide all the HIPEC recovery time and tips you need for a successful outcome.</p></li></ul>

Gamma Knife Radiosurgery
Treatment Price
$3500.00 USDGamma Knife Radiosurgery aims to treat intracranial conditions with extreme precision, minimizing damage to surrounding healthy tissue. It's a non-surgical technique utilizing multiple cobalt-60 sources to deliver a concentrated dose of radiation, often in a single session, leading to high success rates and rapid recovery. DivinHeal connects patients with leading neurosurgery and radiation oncology centers offering this state-of-the-art treatment.
Gamma Knife Radiosurgery aims to treat intracranial conditions with extreme precision, minimizing damage to surrounding healthy tissue. It's a non-surgical technique utilizing multiple cobalt-60 sources to deliver a concentrated dose of radiation, often in a single session, leading to high success rates and rapid recovery. DivinHeal connects patients with leading neurosurgery and radiation oncology centers offering this state-of-the-art treatment.
Treatment Overview
Gamma Knife Radiosurgery aims to treat intracranial conditions with extreme precision, minimizing damage to surrounding healthy tissue. It's a non-surgical technique utilizing multiple cobalt-60 sources to deliver a concentrated dose of radiation, often in a single session, leading to high success rates and rapid recovery. DivinHeal connects patients with leading neurosurgery and radiation oncology centers offering this state-of-the-art treatment.
Procedures
Gamma Knife Radiosurgery involves several precise steps: first, a lightweight stereotactic frame is affixed to the patient's head, serving as a reference point for imaging. Next, high-resolution imaging (MRI, CT, or angiography) is performed to pinpoint the exact location, shape, and size of the target lesion. A multidisciplinary team, including a neurosurgeon, radiation oncologist, and medical physicist, then uses specialized software to plan the precise radiation dose and beam configuration. During the treatment, the patient lies on a couch that slides into the Gamma Knife unit, and the radiation beams are directed with sub-millimeter accuracy to the target. The patient remains awake during the procedure, which can last from minutes to a few hours, depending on the complexity of the case. Once complete, the head frame is removed.
Benefits
<h2>Benefits of Gamma Knife Radiosurgery Treatment</h2><ul><li><h3>Non-Invasive Procedure</h3><p>No incisions, minimal pain, and no general anesthesia required in most cases.</p></li><li><h3>High Precision and Efficacy</h3><p>Delivers highly targeted radiation, protecting healthy brain tissue and achieving excellent clinical outcomes.</p></li><li><h3>Reduced Risks</h3><p>Lower risk of infection, bleeding, and other complications associated with open brain surgery.</p></li><li><h3>Minimal Recovery Time</h3><p>Patients typically go home the same day or the next, with a swift return to normal activities.</p></li><li><h3>Treatment for Inaccessible Lesions</h3><p>Effective for deep-seated or surgically challenging brain lesions.</p></li><li><h3>Single-Session Treatment</h3><p>Often completed in one session, reducing hospital stay and patient inconvenience.</p></li></ul>
Recovery Information
<h2>Gamma Knife Radiosurgery Recovery Time and Tips</h2><h3>Immediate Post-Treatment</h3><p>Most patients experience minimal side effects immediately after Gamma Knife Radiosurgery and can return home the same day. You may feel mild headache, nausea, or fatigue, which typically subside quickly. A brief period of observation is common to ensure comfort before discharge.</p><h3>Long-Term Recovery and Follow-up</h3><p>Full recovery from Gamma Knife Radiosurgery is generally rapid. Patients can usually resume their normal daily activities within 24-48 hours. However, the therapeutic effects of the radiation are gradual, taking weeks, months, or even years for conditions like AVMs to fully resolve. Regular follow-up appointments with your neurosurgeon or radiation oncologist, including imaging scans (MRI), are crucial to monitor the treatment's effectiveness. DivinHeal provides comprehensive support for coordinating these follow-ups, ensuring your long-term wellness.</p><h3>Recovery Tips:</h3><ul><li><strong>Rest:</strong> Allow your body time to heal, even if you feel well.</li><li><strong>Hydration:</strong> Drink plenty of fluids to aid recovery.</li><li><strong>Medication:</strong> Take any prescribed medications for headaches or swelling as directed.</li><li><strong>Avoid Strenuous Activities:</strong> Refrain from heavy lifting or intense exercise for a few days post-procedure.</li><li><strong>Monitor Symptoms:</strong> Report any new or worsening symptoms to your medical team immediately.</li><li><strong>Emotional Support:</strong> Engage in support groups or counseling if needed; DivinHeal can assist in connecting you with resources.</li></ul>

CyberKnife / Stereotactic Radiosurgery (SRS/SBRT)
Treatment Price
$7500.00 USDUnderstanding CyberKnife and Stereotactic Radiosurgery (SRS/SBRT)
CyberKnife and Stereotactic Radiosurgery (SRS/SBRT) are cutting-edge technologies that utilize focused radiation beams to target and destroy abnormal tissue, such as cancerous tumors, benign lesions, or functional disorders. The primary goal is to deliver maximal therapeutic radiation dose to the target while meticulously sparing adjacent healthy organs and critical structures. This non-surgical approach is characterized by its remarkable precision, facilitated by sophisticated image-guidance systems that track tumor movement in real-time, even with patient breathing.
Key Techniques and Goals:
- High Precision: Delivers high doses of radiation with sub-millimeter accuracy to the target.
- Non-Invasive: A non-surgical alternative for many conditions, reducing risks associated with open surgery.
- Fewer Sessions: Often completed in 1 to 5 treatment sessions, unlike conventional radiation which can require dozens.
- Minimized Side Effects: Due to precise targeting, healthy tissue exposure is significantly reduced, leading to fewer complications.
- Real-time Tracking: Advanced systems like CyberKnife can track tumor movement during treatment, adjusting radiation beams dynamically.
Understanding CyberKnife and Stereotactic Radiosurgery (SRS/SBRT)
CyberKnife and Stereotactic Radiosurgery (SRS/SBRT) are cutting-edge technologies that utilize focused radiation beams to target and destroy abnormal tissue, such as cancerous tumors, benign lesions, or functional disorders. The primary goal is to deliver maximal therapeutic radiation dose to the target while meticulously sparing adjacent healthy organs and critical structures. This non-surgical approach is characterized by its remarkable precision, facilitated by sophisticated image-guidance systems that track tumor movement in real-time, even with patient breathing.
Key Techniques and Goals:
- High Precision: Delivers high doses of radiation with sub-millimeter accuracy to the target.
- Non-Invasive: A non-surgical alternative for many conditions, reducing risks associated with open surgery.
- Fewer Sessions: Often completed in 1 to 5 treatment sessions, unlike conventional radiation which can require dozens.
- Minimized Side Effects: Due to precise targeting, healthy tissue exposure is significantly reduced, leading to fewer complications.
- Real-time Tracking: Advanced systems like CyberKnife can track tumor movement during treatment, adjusting radiation beams dynamically.
Treatment Overview
<h3>Understanding CyberKnife and Stereotactic Radiosurgery (SRS/SBRT)</h3><p>CyberKnife and Stereotactic Radiosurgery (SRS/SBRT) are cutting-edge technologies that utilize focused radiation beams to target and destroy abnormal tissue, such as cancerous tumors, benign lesions, or functional disorders. The primary goal is to deliver maximal therapeutic radiation dose to the target while meticulously sparing adjacent healthy organs and critical structures. This non-surgical approach is characterized by its remarkable precision, facilitated by sophisticated image-guidance systems that track tumor movement in real-time, even with patient breathing.</p><h3>Key Techniques and Goals:</h3><ul><li><strong>High Precision:</strong> Delivers high doses of radiation with sub-millimeter accuracy to the target.</li><li><strong>Non-Invasive:</strong> A non-surgical alternative for many conditions, reducing risks associated with open surgery.</li><li><strong>Fewer Sessions:</strong> Often completed in 1 to 5 treatment sessions, unlike conventional radiation which can require dozens.</li><li><strong>Minimized Side Effects:</strong> Due to precise targeting, healthy tissue exposure is significantly reduced, leading to fewer complications.</li><li><strong>Real-time Tracking:</strong> Advanced systems like CyberKnife can track tumor movement during treatment, adjusting radiation beams dynamically.</li></ul>
Procedures
CyberKnife and SRS/SBRT procedures involve several key stages: 1. **Consultation and Diagnosis:** Review of medical history, imaging (MRI, CT, PET), and sometimes biopsy to confirm diagnosis and determine suitability for SRS/SBRT. 2. **Treatment Planning:** Detailed imaging is performed (e.g., high-resolution CT, MRI) to create a precise 3D map of the tumor and surrounding critical structures. A multidisciplinary team (radiation oncologist, medical physicist, dosimetrist) designs a personalized treatment plan, calculating exact radiation doses and beam angles. For some brain SRS, a non-invasive immobilization mask or frame might be fitted. 3. **The Treatment Session(s):** The patient lies comfortably on a treatment couch. For CyberKnife, a robotic arm maneuvers the linear accelerator around the patient, delivering hundreds of precise radiation beams from various angles. For other SRS/SBRT systems, a gantry rotates around the patient. Real-time image guidance systems continuously track the tumor's position, compensating for minor patient movements, including breathing. The procedure is painless and takes 30 minutes to a few hours per session. 4. **Post-Treatment Care:** After the session, the patient can usually go home. Follow-up appointments, often involving imaging, are scheduled to monitor the tumor's response over time.
Benefits
<h3>Benefits of CyberKnife / Stereotactic Radiosurgery (SRS/SBRT)</h3><p>CyberKnife and SRS/SBRT offer numerous advantages, positioning them as preferred treatment options for many patients seeking effective, less invasive care.</p><ul><li><h4><strong>Non-Invasive and Painless:</strong></h4><p>As a non-surgical procedure, there are no incisions, minimal discomfort, and often no need for anesthesia, reducing risks associated with surgery.</p></li><li><h4><strong>Exceptional Precision and Accuracy:</strong></h4><p>Delivers high doses of radiation with sub-millimeter precision, effectively targeting tumors while significantly sparing surrounding healthy tissues and critical organs.</p></li><li><h4><strong>Fewer Treatment Sessions:</strong></h4><p>Unlike conventional radiation therapy that can require weeks of daily treatments, SRS/SBRT is typically completed in 1 to 5 sessions, reducing treatment time and impact on daily life.</p></li><li><h4><strong>Quick Recovery and Return to Normal Activities:</strong></h4><p>Most patients experience minimal side effects and can resume their normal routine almost immediately after treatment, often on the same day.</p></li><li><h4><strong>Effective for Hard-to-Reach Tumors:</strong></h4><p>Ideal for tumors located in sensitive or surgically challenging areas, such as the brain, spine, or near vital organs.</p></li><li><h4><strong>Real-time Tumor Tracking (CyberKnife):</strong></h4><p>The CyberKnife system's ability to track tumor movement in real-time, even with breathing, allows for highly accurate radiation delivery, crucial for moving targets like lung or liver tumors.</p></li><li><h4><strong>Reduced Side Effects:</strong></h4><p>The precise targeting minimizes radiation exposure to healthy tissue, leading to fewer and less severe side effects compared to conventional radiation or chemotherapy.</p></li><li><h4><strong>Outpatient Procedure:</strong></h4><p>Often performed on an outpatient basis, eliminating the need for hospital stays and reducing associated costs and inconvenience.</p></li><li><h4><strong>Versatile Application:</strong></h4><p>Effective for treating a broad spectrum of conditions, including primary and metastatic cancers, benign tumors, and certain functional disorders like trigeminal neuralgia.</p></li></ul>
Recovery Information
<h3>CyberKnife / SRS/SBRT Recovery: What to Expect</h3><p>One of the significant advantages of CyberKnife and Stereotactic Radiosurgery (SRS/SBRT) is the typically short and manageable recovery period, allowing most patients to quickly return to their daily lives.</p><ul><li><h4><strong>Immediate Post-Treatment:</strong></h4><p>Most patients can go home shortly after their SRS/SBRT session. You might experience mild fatigue, headache, or nausea, which are usually temporary and manageable with medication. Any immobilization devices (like a head frame for brain SRS) are removed immediately after the procedure.</p></li><li><h4><strong>Short-Term Recovery (Days to Weeks):</strong></h4><p>Within a few days, most patients report feeling back to their usual selves. It is generally advised to avoid strenuous activities for a week or two, but light activities and work can often be resumed sooner. Any skin irritation in the treated area is rare due to the precision of the treatment.</p></li><li><h4><strong>Managing Potential Side Effects:</strong></h4><p>While minimal, specific side effects can depend on the treated area. For brain SRS, temporary swelling or neurological symptoms might occur but are typically managed with medication. For body SBRT, mild digestive upset or fatigue can sometimes be experienced. Your medical team will provide specific guidance and support.</p></li><li><h4><strong>Long-Term Follow-up:</strong></h4><p>Regular follow-up appointments with your radiation oncologist will be scheduled to monitor your progress. This typically involves imaging scans (MRI, CT, PET) at prescribed intervals to assess the tumor's response to treatment. The full effect of SRS/SBRT can take several months to become evident.</p></li><li><h4><strong>Lifestyle Modifications:</strong></h4><p>Generally, no significant long-term lifestyle changes are required solely due to SRS/SBRT. A healthy lifestyle, including a balanced diet and regular exercise, is always encouraged for overall well-being and to support long-term recovery.</p></li></ul>
Meet Our Doctors
Meet our team of highly qualified and experienced medical professionals dedicated to providing the best healthcare services.

Dodul Mondal
Sr. Consultant
Medical & Haemato Oncology
New Delhi
8+ Years
Experience
Apolo Delhi
Hospital
1500
Fees
Dr. Aditya Gupta
Chairperson - Neurosurgery & CNS Radiosurgery & Co-Chief - Cyberknife Centre
Neurosurgery
New Delhi
32+ Years
Experience
Artemis Hospital
Hospital
1500
Fees

Dr. Alok Gupta
Director
Oncology
New Delhi
26+ Years
Experience
Apolo Delhi
Hospital
1500
Fees

Dr. Alok Srivastava
Principal Consultant
Urology
New Delhi
32+ Years
Experience
Apolo Delhi
Hospital
1500
Fees

Dr. Amita Naithani
Sr. Consultant - Gynae Oncology
Gynaecological Oncology
New Delhi
10+ Years
Experience
Artemis Hospital
Hospital
1500
Fees

Dr. Anil Prasad Bhatt
Principal Consultant
Urology, Uro-Oncology, Renal Transplant
New Delhi
30+ Years
Experience
Apolo Delhi
Hospital
1500
Fees

Dr. Ankit Goel
Consultant - Urology & Renal Transplant
Urology, Renal Transplant, Robotic Surgery
New Delhi
15+ Years
Experience
Artemis Hospital
Hospital
1500
Fees

Dr Anshuman Kumar
Principal Director & Unit Head – Surgical Oncology
Surgical Oncology
New Delhi
19+ Years
Experience
Max Hospital,Gurgaon
Hospital
1500
Fees

Dr. Anshuman Manaswi
Senior Consultant Plastic Surgeon
Plastic Surgery
New Delhi
19+ Years
Experience
Max Hospital,Gurgaon
Hospital
1500
Fees

Dr. Aparna Sinha
Associate Director
Pulmonology
New Delhi
22+ Years
Experience
Apolo Delhi
Hospital
1500
Fees

Dr. Ashish Vashistha
Principal Consultant
Minimal Access, Bariatric & GI Surgery
New Delhi
23+ Years
Experience
Apolo Delhi
Hospital
1500
Fees

Dr. Asit Arora
Senior Director, Head of Department - Urology, Uro-Oncology, Robotics and Renal Transplant
Urology, Uro-Oncology, Robotics and Renal Transplant
New Delhi
25+ Years
Experience
Apolo Delhi
Hospital
1500
Fees

Dr. Avtar Singh Bath
Associate Director - Urology and Renal Transplant
Urology
New Delhi
27+ Years
Experience
Apolo Delhi
Hospital
1500
Fees

Dr. Bachan Singh Barthwal
Principal Director - Laparoscopic & Robotic General Surgery
General Surgery, Laparoscopic / Minimal Access Surgery, Robotic Surgery
New Delhi
37+ Years
Experience
Max Hospital,Gurgaon
Hospital
1500
Fees

Dr. Chandeep Singh
Director
Urology
New Delhi
15+ Years
Experience
Apolo Delhi
Hospital
1500
Fees

Dr. C.P.S. Chauhan
Principal Director & Chief of Medical Oncology
Medical Oncology
New Delhi
30+ Years
Experience
Apolo Delhi
Hospital
1500
Fees

Dr. Deepa Goel
Head Unit II
Pathology
New Delhi
21+ Years
Experience
Artemis Hospital
Hospital
1500
Fees

Dr. Deepak Jha
Chief - Breast Surgery & Sr. Consultant : Surgical Oncology
Breast Surgery, Oncology
New Delhi
15+ Years
Experience
Artemis Hospital
Hospital
1500
Fees

Dr. Deepa Maheshwari
Unit Head
Maternity, Obstetrics & Gynaecology
New Delhi
20+ Years
Experience
Artemis Hospital
Hospital
1500
Fees

Dr. Dheeraj Batheja
Senior Consultant - Ortho Spine Surgery
Orthopaedic Surgery, Spine Surgery
New Delhi
12+ Years
Experience
Artemis Hospital
Hospital
1500
Fees