Centres Of Excellence
Our Centres of Excellence bring together multidisciplinary teams to deliver precise diagnosis, advanced treatments, and superior outcomes across a wide spectrum of medical specialties.

Related Links
Doctors For Treatment in Similar Locations
Best Hospital Near by for treatment
Other Treatments Nearby
Treatments in India for Visitors
Doctors For Treatment in Similar Locations
Best Hospital Near by for treatment
Related Links
- ENT cost in Hyderabad
- ENT cost in India
- ENT cost in Mumbai
- ENT cost in New Delhi
- ENT cost in Pune
- ENT Success Rate in Bengaluru
- ENT Success Rate in Chennai
- ENT Success Rate in Haryana
- ENT Success Rate in Hyderabad
- ENT Success Rate in India
- ENT Success Rate in Mumbai
- ENT Success Rate in New Delhi
- ENT Success Rate in Pune
Other Treatments Nearby
Treatments in India for Visitors
- ENT Treatment in Bengaluru for Nigeria
- ENT Treatment in Bengaluru for UAE
- ENT Treatment in Chennai for Bangladesh
- ENT Treatment in Chennai for Ethiopia
- ENT Treatment in Chennai for Iraq
- ENT Treatment in Chennai for Nigeria
- ENT Treatment in Chennai for UAE
- ENT Treatment in Gurugram for Bangladesh
- ENT Treatment in Gurugram for Ethiopia
- ENT Treatment in Gurugram for Iraq
- ENT Treatment in Gurugram for Nigeria
- ENT Treatment in Gurugram for UAE
- ENT Treatment in Hyderabad for Bangladesh
- ENT Treatment in Hyderabad for Ethiopia
- ENT Treatment in Hyderabad for Iraq
- ENT Treatment in Hyderabad for Nigeria
- ENT Treatment in Hyderabad for UAE
- ENT Treatment in India for Bangladesh
- ENT Treatment in India for Ethiopia
- ENT Treatment in India for Iraq
- ENT Treatment in India for Nigeria
- ENT Treatment in India for UAE
- ENT Treatment in Mumbai for Bangladesh
- ENT Treatment in Mumbai for Ethiopia
- ENT Treatment in Mumbai for Iraq
- ENT Treatment in Mumbai for Nigeria
- ENT Treatment in Mumbai for UAE
- ENT Treatment in New Delhi for Bangladesh
- ENT Treatment in New Delhi for Ethiopia
- ENT Treatment in New Delhi for Iraq
- ENT Treatment in New Delhi for Nigeria
- ENT Treatment in New Delhi for UAE
- ENT Treatment in Pune for Bangladesh
- ENT Treatment in Pune for Ethiopia
- ENT Treatment in Pune for Iraq
- ENT Treatment in Pune for Nigeria
- ENT Treatment in Pune for UAE
Related Treatments
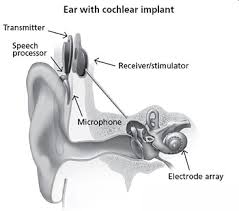
Cochlear Implant Surgery
Treatment Price
$15000.00 USDOverview of Cochlear Implant Surgery
Restoring the Gift of Sound
Cochlear Implant Surgery is a sophisticated medical intervention aimed at providing a sense of sound to individuals who cannot benefit from traditional hearing aids. The primary goal is to improve speech perception and environmental sound awareness, significantly enhancing the patient's quality of life and communication abilities. This intricate procedure involves implanting an internal device beneath the skin behind the ear, with an electrode array threaded into the cochlea, and an external sound processor worn on the ear. DivinHeal ensures access to cutting-edge technology and experienced surgical teams for optimal outcomes.
Overview of Cochlear Implant Surgery
Restoring the Gift of Sound
Cochlear Implant Surgery is a sophisticated medical intervention aimed at providing a sense of sound to individuals who cannot benefit from traditional hearing aids. The primary goal is to improve speech perception and environmental sound awareness, significantly enhancing the patient's quality of life and communication abilities. This intricate procedure involves implanting an internal device beneath the skin behind the ear, with an electrode array threaded into the cochlea, and an external sound processor worn on the ear. DivinHeal ensures access to cutting-edge technology and experienced surgical teams for optimal outcomes.
Treatment Overview
<h2>Overview of Cochlear Implant Surgery</h2><h3>Restoring the Gift of Sound</h3><p>Cochlear Implant Surgery is a sophisticated medical intervention aimed at providing a sense of sound to individuals who cannot benefit from traditional hearing aids. The primary goal is to improve speech perception and environmental sound awareness, significantly enhancing the patient's quality of life and communication abilities. This intricate procedure involves implanting an internal device beneath the skin behind the ear, with an electrode array threaded into the cochlea, and an external sound processor worn on the ear. DivinHeal ensures access to cutting-edge technology and experienced surgical teams for optimal outcomes.</p>
Procedures
Cochlear Implant Surgery is typically performed under general anesthesia. The surgeon makes an incision behind the ear, creating a small pocket under the skin to hold the internal receiver-stimulator. A small opening is then made in the mastoid bone to access the middle ear. Through this opening, the electrode array is carefully threaded into the cochlea. Once the internal device is secured, the incision is closed. The entire procedure usually takes 2-4 hours. After the surgery, the patient typically stays in the hospital for 1-3 days for observation.
Benefits
<h2>Key Benefits of Cochlear Implant Surgery</h2><h3>A Transformative Solution for Hearing Loss</h3><ul><li><strong>Significant Improvement in Hearing:</strong> Patients often experience a dramatic increase in their ability to perceive speech and environmental sounds.</li><li><strong>Enhanced Speech Understanding:</strong> Leads to better comprehension in various listening situations, improving communication.</li><li><strong>Improved Quality of Life:</strong> Greater independence, confidence, and participation in social and professional activities.</li><li><strong>Better Sound Localization:</strong> Many bilateral implant users gain the ability to determine the direction of sound.</li><li><strong>Safety & Efficacy:</strong> A well-established and generally safe procedure with a high 'Cochlear Implant Surgery success rate' for appropriate candidates.</li><li><strong>Access to Education & Employment:</strong> Especially for children, early implantation can significantly improve educational outcomes and future employment prospects.</li></ul>
Recovery Information
<h2>Cochlear Implant Surgery Recovery Time and Tips</h2><h3>A Phased Approach to Auditory Rehabilitation</h3><p>The 'Cochlear Implant Surgery recovery time and tips' involves several stages, beginning immediately after surgery and extending through a period of auditory rehabilitation.</p><ul><li><strong>Immediate Post-Surgery (1-3 days hospital stay):</strong> Patients will experience some discomfort around the incision site, which is managed with pain medication. The bandage is typically removed within a day or two, and patients are usually discharged within 1-3 days.</li><li><strong>Initial Healing (2-4 weeks):</strong> During this period, the incision heals completely, and swelling subsides. Strenuous activities should be avoided. The implant is typically not activated until this healing is complete.</li><li><strong>Activation & Initial Programming:</strong> Approximately 2-4 weeks after surgery, the external sound processor is switched on for the first time. This is a critical moment where sounds are introduced gradually, and the device is programmed by an audiologist.</li><li><strong>Auditory Rehabilitation (Months to Years):</strong> This is the most crucial phase. Patients work with audiologists and speech therapists to 'learn to hear' with the implant. This involves listening exercises, speech therapy, and adapting to new sound perceptions. The brain needs time to interpret the new electrical signals.</li><li><strong>Long-term Care:</strong> Regular follow-up appointments are essential for fine-tuning the processor, monitoring hearing progress, and addressing any concerns. DivinHeal ensures you have access to continuous support for your entire recovery journey.</li></ul>

Septoplasty
Treatment Price
$1500.00 USDSeptoplasty focuses on straightening the nasal septum, which is composed of cartilage and bone. The primary goal is to optimize airflow through the nostrils, providing relief from symptoms caused by a misaligned septum. The procedure is typically performed by an Otolaryngologist (ENT specialist) and is highly effective in improving respiratory function.
Septoplasty focuses on straightening the nasal septum, which is composed of cartilage and bone. The primary goal is to optimize airflow through the nostrils, providing relief from symptoms caused by a misaligned septum. The procedure is typically performed by an Otolaryngologist (ENT specialist) and is highly effective in improving respiratory function.
Treatment Overview
Septoplasty focuses on straightening the nasal septum, which is composed of cartilage and bone. The primary goal is to optimize airflow through the nostrils, providing relief from symptoms caused by a misaligned septum. The procedure is typically performed by an Otolaryngologist (ENT specialist) and is highly effective in improving respiratory function.
Procedures
Septoplasty is usually performed under general anesthesia. The surgeon makes an incision inside the nose, lifts the mucous membrane covering the septum, and then reshapes or removes portions of the cartilage and bone that are causing the deviation. Once the septum is straightened and repositioned, the membrane is laid back down, and the incision is closed with dissolvable sutures. Nasal packing or soft splints may be inserted to support the septum during initial healing.
Benefits
The primary benefits of Septoplasty include significantly improved nasal breathing, reduction or elimination of chronic sinus infections, decreased incidence of nosebleeds, and relief from related headaches. Patients often report better sleep quality, reduced snoring, and an overall enhancement in their quality of life due to unhindered airflow.
Recovery Information
Septoplasty recovery typically involves some initial swelling, bruising, and discomfort for a few days post-surgery. Nasal packing or splints may be used for support, usually removed within a week. Most patients can return to light activities within a few days to a week, with full recovery and resolution of swelling taking several weeks to a few months. Detailed post-operative instructions for care, pain management, and activity restrictions will be provided.
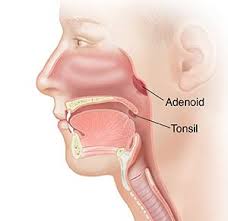
Tonsillectomy & Adenoidectomy
Treatment Price
$1200.00 USDOverview of Tonsillectomy & Adenoidectomy
Tonsillectomy & Adenoidectomy is a routine ENT procedure aimed at improving a patient's quality of life by addressing chronic infections or obstructions caused by these lymphoid tissues. The goals include reducing the frequency of sore throats, resolving sleep-disordered breathing, and enhancing overall respiratory health. Techniques involve various surgical methods, including traditional cold knife dissection, electrocautery, radiofrequency ablation, or microdebrider, all performed under general anesthesia.
Overview of Tonsillectomy & Adenoidectomy
Tonsillectomy & Adenoidectomy is a routine ENT procedure aimed at improving a patient's quality of life by addressing chronic infections or obstructions caused by these lymphoid tissues. The goals include reducing the frequency of sore throats, resolving sleep-disordered breathing, and enhancing overall respiratory health. Techniques involve various surgical methods, including traditional cold knife dissection, electrocautery, radiofrequency ablation, or microdebrider, all performed under general anesthesia.
Treatment Overview
<h2>Overview of Tonsillectomy & Adenoidectomy</h2><p>Tonsillectomy & Adenoidectomy is a routine ENT procedure aimed at improving a patient's quality of life by addressing chronic infections or obstructions caused by these lymphoid tissues. The goals include reducing the frequency of sore throats, resolving sleep-disordered breathing, and enhancing overall respiratory health. Techniques involve various surgical methods, including traditional cold knife dissection, electrocautery, radiofrequency ablation, or microdebrider, all performed under general anesthesia.</p>
Procedures
Tonsillectomy & Adenoidectomy is performed under general anesthesia. The patient is asleep throughout the procedure. The surgeon typically accesses the tonsils through the mouth. There are several techniques for removing the tonsils and adenoids, including: 1. **Cold Knife Dissection:** The surgeon uses a scalpel to remove the tonsils, and then bleeding is controlled with sutures or cautery. The adenoids are often removed using a curette or microdebrider, accessing them through the mouth or nose. 2. **Electrocautery:** Heat is used to remove the tissues and stop bleeding simultaneously. 3. **Radiofrequency Ablation (Coblation):** Uses low-temperature radiofrequency energy to remove tissue and minimize damage to surrounding areas, potentially leading to less post-operative pain. 4. **Microdebrider:** A small, rotating blade is used to shave off the adenoid tissue while suctioning it away. This method is often used for adenoidectomy. The choice of technique depends on the surgeon's preference and the patient's specific condition. After the tissues are removed, any bleeding is carefully controlled. The procedure typically lasts between 30 to 60 minutes, and patients are monitored in a recovery room before being discharged, usually within the same day or after an overnight stay.
Benefits
<h2>Benefits of Tonsillectomy & Adenoidectomy</h2><ul><li><h3>Significant Reduction in Infections</h3><p>Patients experience a dramatic decrease in the frequency and severity of throat and ear infections.</p></li><li><h3>Improved Breathing and Sleep</h3><p>Resolution of obstructive sleep apnea, snoring, and chronic nasal obstruction, leading to better sleep quality and daytime alertness.</p></li><li><h3>Enhanced Quality of Life</h3><p>Fewer sick days, improved academic or work performance, and overall better health and well-being.</p></li><li><h3>Reduced Antibiotic Use</h3><p>Less reliance on antibiotics helps prevent antibiotic resistance and protects gut health.</p></li><li><h3>Better Speech and Swallowing</h3><p>For some, removing enlarged tissues can improve articulation and ease of swallowing.</p></li></ul>
Recovery Information
<h2>Recovery Time and Tips After Tonsillectomy & Adenoidectomy</h2><p>Recovery from Tonsillectomy & Adenoidectomy typically takes about 7 to 14 days, though individual experiences may vary. The most common symptom is a sore throat, which can be managed effectively with pain medication.</p><h3>Immediate Post-operative Period (Days 1-3)</h3><ul><li><strong>Pain Management:</strong> Regular pain medication is crucial. Follow your doctor's prescriptions diligently.</li><li><strong>Hydration:</strong> Drink plenty of fluids (water, clear broths, diluted juices) to prevent dehydration and keep the throat moist. Avoid acidic or very hot beverages.</li><li><strong>Diet:</strong> Start with soft, bland foods like ice cream, yogurt, mashed potatoes, and scrambled eggs. Gradually introduce more solid foods as tolerated.</li><li><strong>Rest:</strong> Prioritize rest to aid healing. Avoid strenuous activities.</li></ul><h3>Later Recovery Period (Days 4-14)</h3><ul><li><strong>Activity:</strong> Gradually increase activity levels, but avoid heavy lifting or vigorous exercise.</li><li><strong>Pain Fluctuations:</strong> Pain might temporarily worsen around days 5-7 as the scabs in the throat begin to come off. This is normal. Continue pain management as needed.</li><li><strong>Return to School/Work:</strong> Most children can return to school after 7-10 days, and adults can resume light work within the same timeframe, provided they feel well enough.</li></ul><h3>Important Recovery Tips:</h3><ul><li><strong>Avoid Irritants:</strong> Steer clear of smoking, secondhand smoke, and spicy, crunchy, or acidic foods.</li><li><strong>Voice Rest:</strong> Try not to yell or clear your throat forcefully.</li><li><strong>Monitor for Complications:</strong> Watch for signs of bleeding (fresh red blood), severe pain not controlled by medication, or fever. Contact your doctor immediately if these occur.</li><li><strong>Follow-up:</strong> Attend all scheduled follow-up appointments with your ENT specialist.</li></ul><p>DivinHeal provides comprehensive post-operative support, ensuring you have access to medical advice and care coordination throughout your recovery journey.</p>
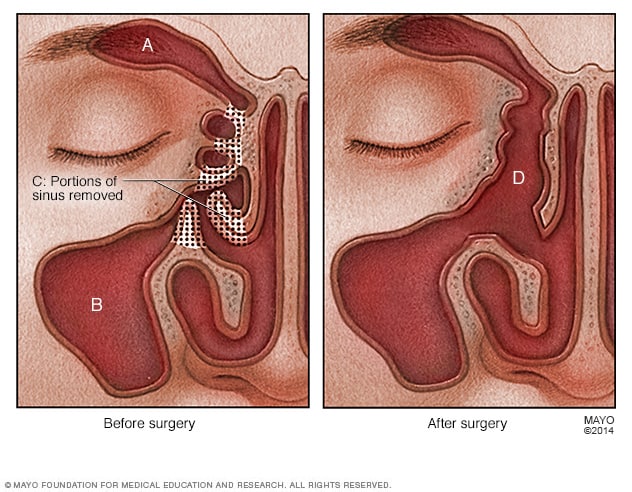
Endoscopic Sinus Surgery (FESS)
Treatment Price
$2500.00 USDFESS is designed to remove blockages in the sinus drainage pathways using a small, lighted tube called an endoscope. This procedure offers precise removal of diseased tissue, polyps, or bone while preserving healthy structures. The primary goal is to alleviate chronic sinus symptoms such as congestion, facial pain, headaches, and impaired smell, offering long-term relief.
FESS is designed to remove blockages in the sinus drainage pathways using a small, lighted tube called an endoscope. This procedure offers precise removal of diseased tissue, polyps, or bone while preserving healthy structures. The primary goal is to alleviate chronic sinus symptoms such as congestion, facial pain, headaches, and impaired smell, offering long-term relief.
Treatment Overview
FESS is designed to remove blockages in the sinus drainage pathways using a small, lighted tube called an endoscope. This procedure offers precise removal of diseased tissue, polyps, or bone while preserving healthy structures. The primary goal is to alleviate chronic sinus symptoms such as congestion, facial pain, headaches, and impaired smell, offering long-term relief.
Procedures
Endoscopic Sinus Surgery (FESS) is performed under general anesthesia. The surgeon inserts a thin, lighted endoscope into the nostril to visualize the sinus openings on a monitor. Specialized micro-instruments are then guided through the nostril alongside the endoscope. The surgeon carefully removes any obstructing tissue, such as nasal polyps, scar tissue, or small amounts of bone, to widen the natural drainage pathways of the sinuses. If necessary, a deviated septum may be corrected (septoplasty) or enlarged turbinates reduced (turbinate reduction) during the same procedure to further improve airflow. No external incisions are made. At the end of the procedure, dissolvable packing or a stent may be placed in the sinuses to aid healing and prevent adhesion formation.
Benefits
<h2>Benefits of Endoscopic Sinus Surgery (FESS)</h2><ul><li><h3>Improved Breathing</h3><p>Significantly reduces nasal congestion and improves airflow, leading to easier breathing.</p></li><li><h3>Reduced Sinus Infections</h3><p>By restoring natural drainage, FESS decreases the frequency and severity of chronic and recurrent acute sinusitis.</p></li><li><h3>Relief from Chronic Symptoms</h3><p>Alleviates persistent facial pain, pressure, headaches, and post-nasal drip associated with chronic sinusitis.</p></li><li><h3>Enhanced Sense of Smell and Taste</h3><p>Many patients experience an improvement in their olfactory and gustatory senses.</p></li><li><h3>Minimally Invasive</h3><p>Performed through the nostrils with an endoscope, avoiding external incisions and resulting in less pain, scarring, and a quicker recovery.</p></li><li><h3>Targeted Treatment</h3><p>Allows for precise removal of diseased tissue, polyps, or bone while preserving healthy structures.</p></li><li><h3>Long-term Relief</h3><p>Offers durable solutions for chronic sinus issues unresponsive to medical management.</p></li></ul>
Recovery Information
<h2>Endoscopic Sinus Surgery (FESS) Recovery Time and Tips</h2><p>Recovery after Endoscopic Sinus Surgery (FESS) is generally swift due to its minimally invasive nature. Most patients can return to light activities within a few days, with full recovery typically taking 3 to 6 weeks. Initial discomfort, mild bleeding, and congestion are common. </p><h3>Key Recovery Steps:</h3><ul><li><strong>Pain Management:</strong> Mild pain relievers can manage post-operative discomfort.</li><li><strong>Nasal Care:</strong> Regular saline rinses are crucial to keep the nasal passages clean and moist, preventing crusting.</li><li><strong>Activity Restrictions:</strong> Avoid strenuous activities, heavy lifting, and nose-blowing for at least 1-2 weeks.</li><li><strong>Follow-up Appointments:</strong> Essential for your ENT specialist to clean the sinuses and monitor healing.</li><li><strong>Medication:</strong> Adhere to any prescribed antibiotics or nasal steroids to aid healing and prevent recurrence.</li></ul><p>DivinHeal's dedicated care coordinators provide comprehensive guidance throughout your Endoscopic Sinus Surgery (FESS) recovery, ensuring you have all the information and support needed for a smooth and effective healing process.</p>

Tympanoplasty (Eardrum Repair)
Treatment Price
$2000.00 USDTympanoplasty Overview: Restoring Your Hearing Health
Tympanoplasty is a highly effective surgical solution for individuals suffering from a perforated eardrum (tympanic membrane) or damage to the middle ear bones. A healthy eardrum is vital for clear hearing and acts as a protective barrier against infections. When perforated due to injury, infection, or other causes, it can lead to significant hearing loss and chronic ear problems. This procedure meticulously reconstructs the eardrum, often using a tissue graft, and can also address issues with the small bones of hearing, offering renewed auditory function and a better quality of life.
DivinHeal connects you with top ENT specialists and world-class facilities for Tympanoplasty, ensuring safe, high-quality, and affordable eardrum repair solutions.
Tympanoplasty Overview: Restoring Your Hearing Health
Tympanoplasty is a highly effective surgical solution for individuals suffering from a perforated eardrum (tympanic membrane) or damage to the middle ear bones. A healthy eardrum is vital for clear hearing and acts as a protective barrier against infections. When perforated due to injury, infection, or other causes, it can lead to significant hearing loss and chronic ear problems. This procedure meticulously reconstructs the eardrum, often using a tissue graft, and can also address issues with the small bones of hearing, offering renewed auditory function and a better quality of life.
DivinHeal connects you with top ENT specialists and world-class facilities for Tympanoplasty, ensuring safe, high-quality, and affordable eardrum repair solutions.
Treatment Overview
<h2>Tympanoplasty Overview: Restoring Your Hearing Health</h2><p>Tympanoplasty is a highly effective surgical solution for individuals suffering from a perforated eardrum (tympanic membrane) or damage to the middle ear bones. A healthy eardrum is vital for clear hearing and acts as a protective barrier against infections. When perforated due to injury, infection, or other causes, it can lead to significant hearing loss and chronic ear problems. This procedure meticulously reconstructs the eardrum, often using a tissue graft, and can also address issues with the small bones of hearing, offering renewed auditory function and a better quality of life.</p><p>DivinHeal connects you with top ENT specialists and world-class facilities for Tympanoplasty, ensuring safe, high-quality, and affordable eardrum repair solutions.</p>
Procedures
The Tympanoplasty procedure typically begins with the patient under general anesthesia. The surgeon makes an incision, either through the ear canal (transcanal), just above the ear opening (endaural), or behind the ear (postauricular), depending on the size and location of the perforation and the surgeon's preference. A small piece of graft tissue, usually fascia (connective tissue) from the temporalis muscle behind the ear or cartilage from the tragus, is harvested. The surgeon carefully lifts the existing eardrum and uses the graft to patch the perforation. The graft is secured in place, often with absorbable packing material placed in the middle ear space and sometimes in the ear canal. If the ossicles (tiny middle ear bones) are also damaged, they will be repaired or replaced during the same procedure (ossiculoplasty). Finally, the eardrum is repositioned, and the incision is closed with sutures. The procedure usually takes 1-3 hours.
Benefits
<h2>Benefits of Tympanoplasty (Eardrum Repair)</h2><p>Undergoing Tympanoplasty offers numerous significant benefits that can dramatically improve a patient's quality of life:</p><ul><li><h3>Improved Hearing:</h3> The primary goal of the surgery is to close the eardrum perforation and, if necessary, repair the middle ear bones, leading to a significant improvement in hearing ability. Many patients report a complete restoration of their pre-perforation hearing levels.</li><li><h3>Prevention of Recurrent Infections:</h3> By sealing the eardrum, the procedure creates a protective barrier, preventing water, bacteria, and foreign particles from entering the middle ear. This drastically reduces the incidence of chronic or recurrent ear infections.</li><li><h3>Elimination of Ear Discharge:</h3> For those suffering from persistent ear discharge (otorrhea) due to chronic infections, Tympanoplasty often resolves this uncomfortable and unhygienic symptom.</li><li><h3>Enhanced Quality of Life:</h3> With improved hearing, reduced infections, and no more discharge, patients experience a profound enhancement in their overall quality of life, allowing them to participate more fully in social activities and work.</li><li><h3>Reduced Need for Hearing Aids:</h3> For many, successful Tympanoplasty can eliminate or reduce the need for hearing aids, offering a more natural hearing experience.</li><li><h3>Peace of Mind:</h3> Knowing that the eardrum is repaired and protected brings immense peace of mind, alleviating concerns about future complications and hearing deterioration.</li></ul><p>DivinHeal connects you with experienced ENT surgeons who are dedicated to achieving the best possible outcomes for your Tympanoplasty, ensuring you benefit fully from this life-changing procedure.</p>
Recovery Information
<h2>Tympanoplasty Recovery Time and Tips</h2><p>Recovery from Tympanoplasty is a gradual process, but with proper care, most patients experience a successful outcome and significant improvement in hearing. DivinHeal provides comprehensive guidance to ensure a smooth recovery journey.</p><h3>Immediate Post-Operative Period (First Few Days):</h3><ul><li><strong>Hospital Stay:</strong> You will typically stay in the hospital for 1-2 days.</li><li><strong>Ear Packing:</strong> Your ear canal will likely be packed with dressing material, and a bandage may be placed over the ear. This helps the graft heal and reduces swelling.</li><li><strong>Mild Discomfort:</strong> You may experience mild ear pain, popping sensations, or dizziness, which can be managed with prescribed pain medication.</li><li><strong>Hearing Fluctuation:</strong> Hearing may initially be muffled due to packing and swelling, but it will gradually improve.</li></ul><h3>First Few Weeks (2-4 Weeks):</h3><ul><li><strong>Activity Restrictions:</strong></li><ul><li>Avoid strenuous activities, heavy lifting, and bending over.</li><li>Do not blow your nose forcefully. If you must sneeze, do so with your mouth open.</li><li>Protect your ear from water. No swimming, and use a shower cap or cotton ball with petroleum jelly during bathing.</li><li>Avoid air travel or activities involving rapid changes in air pressure.</li></ul><li><strong>Medications:</strong> Continue prescribed antibiotics and pain relievers as directed.</li><li><strong>Follow-up:</strong> Your surgeon will remove packing (if present) and assess healing during follow-up appointments.</li></ul><h3>Long-Term Recovery (Up to 3-6 Months):</h3><ul><li><strong>Hearing Improvement:</strong> Significant hearing improvement often becomes noticeable after 3-6 weeks, with full results potentially taking several months as the middle ear fully heals and swells subside.</li><li><strong>Lifestyle:</strong> Most normal activities can be resumed, but continued caution with ear protection (e.g., in noisy environments or when swimming) is advisable.</li></ul><h3>Recovery Tips from DivinHeal:</h3><ul><li><strong>Follow All Instructions:</strong> Adhere strictly to your surgeon's post-operative care instructions.</li><li><strong>Keep Ear Dry:</strong> This is critical for graft survival and preventing infection.</li><li><strong>Avoid Pressure Changes:</strong> Refrain from activities that create pressure in the ear (e.g., nose blowing, straining, air travel).</li><li><strong>Protect Your Ear:</strong> Avoid loud noises and direct trauma to the ear.</li><li><strong>Attend Follow-ups:</strong> Regular check-ups are essential to monitor healing.</li><li><strong>Stay Positive:</strong> Be patient with the healing process. DivinHeal's care coordinators are always available to assist with any questions or concerns during your recovery.</li></ul>

Stapedectomy / Stapedotomy
Treatment Price
$3500.00 USDThe primary goal of Stapedectomy / Stapedotomy is to significantly improve or restore hearing for individuals suffering from otosclerosis. This microsurgical technique aims to bypass the stiffened stapes bone, allowing sound waves to transmit effectively to the inner ear, thereby enhancing sound perception and quality of life. DivinHeal connects patients with top ENT surgeons and state-of-the-art facilities for optimal outcomes.
The primary goal of Stapedectomy / Stapedotomy is to significantly improve or restore hearing for individuals suffering from otosclerosis. This microsurgical technique aims to bypass the stiffened stapes bone, allowing sound waves to transmit effectively to the inner ear, thereby enhancing sound perception and quality of life. DivinHeal connects patients with top ENT surgeons and state-of-the-art facilities for optimal outcomes.
Treatment Overview
The primary goal of Stapedectomy / Stapedotomy is to significantly improve or restore hearing for individuals suffering from otosclerosis. This microsurgical technique aims to bypass the stiffened stapes bone, allowing sound waves to transmit effectively to the inner ear, thereby enhancing sound perception and quality of life. DivinHeal connects patients with top ENT surgeons and state-of-the-art facilities for optimal outcomes.
Procedures
Stapedectomy / Stapedotomy is a microsurgical procedure performed under general or local anesthesia. The surgeon typically makes an incision inside the ear canal or sometimes behind the ear. Using a surgical microscope for magnification, the surgeon carefully elevates the eardrum to access the middle ear bones. In Stapedectomy, the fixed stapes bone is carefully removed. In Stapedotomy, a small opening is created in the stapes footplate. A tiny prosthetic piston, usually made of Teflon or titanium, is then inserted. One end of the piston is connected to the incus (the middle bone in the chain), and the other end is placed into the opening created in the inner ear, allowing sound vibrations to bypass the fixed stapes and reach the inner ear fluids. The eardrum is then repositioned, and the incision is closed with sutures or packing.
Benefits
<h2>Benefits of Stapedectomy / Stapedotomy Treatment</h2><ul> <li><h3>Significant Hearing Improvement</h3><p>The primary benefit is a substantial restoration of hearing, often leading to a dramatic improvement in the ability to understand speech and perceive sounds.</p></li> <li><h3>Enhanced Quality of Life</h3><p>Improved hearing can lead to better communication, increased social engagement, and a reduced sense of isolation, significantly boosting overall well-being.</p></li> <li><h3>Permanent Solution for Otosclerosis</h3><p>For many patients, Stapedectomy/Stapedotomy offers a long-lasting or permanent fix for conductive hearing loss caused by otosclerosis, reducing the need for continuous use of hearing aids.</p></li> <li><h3>Minimally Invasive Microsurgery</h3><p>The procedure is a delicate microsurgery, often performed through the ear canal, minimizing visible scarring and recovery time.</p></li> <li><h3>High Success Rates</h3><p>Stapedectomy/Stapedotomy boasts high success rates in restoring functional hearing, especially when performed by experienced ENT surgeons.</p></li></ul>
Recovery Information
<h2>Recovery and Life After Stapedectomy / Stapedotomy</h2><h3>Immediate Post-operative Period (1-3 days)</h3><p>After Stapedectomy / Stapedotomy, patients typically stay in the hospital for 1-2 days. You may experience some dizziness, nausea, and mild ear discomfort, which are managed with prescribed medications. It's crucial to avoid sudden head movements, straining, or blowing your nose forcefully. A small dressing or packing will be in your ear, which an ENT specialist will remove during a follow-up.</p><h3>First Few Weeks (1-4 weeks)</h3><p>During this period, gradual hearing improvement often occurs. Some fluctuations in hearing, muffled sounds, or minor clicking sensations are normal as the ear heals. Avoid heavy lifting, strenuous activities, swimming, or flying. Keep your ear dry and protected. You will have follow-up appointments with your surgeon and an audiologist to monitor healing and hearing progression.</p><h3>Long-Term Recovery (1-3 months and beyond)</h3><p>Full hearing improvement can take several weeks to a few months. Most patients experience significant and stable hearing benefits. Physical therapy is not typically required, but adherence to post-operative instructions is vital. Your audiologist may conduct further hearing tests to assess the final outcome. Maintaining good ear hygiene and having regular check-ups with your ENT specialist are recommended. DivinHeal provides ongoing support and coordinates your long-term follow-up care to ensure sustained well-being and satisfaction.</p>

Sleep Apnea Surgery (UPPP) / Sleep Study
Treatment Price
$3500.00 USDOverview of Sleep Apnea Treatment
Addressing Obstructive Sleep Apnea for Better Health
Obstructive Sleep Apnea (OSA) is a serious condition where breathing repeatedly stops and starts during sleep. DivinHeal offers advanced diagnostic Sleep Studies and effective surgical and non-surgical treatments for OSA, including Uvulopalatopharyngoplasty (UPPP). Our goal is to restore restful sleep, improve oxygenation, and mitigate associated health risks like cardiovascular disease and stroke.
- Diagnosis: In-depth Sleep Study (Polysomnography) to confirm OSA and determine severity.
- Treatment Goals: Widen airways, reduce snoring, eliminate apnea events, and improve sleep quality.
- Techniques: UPPP involves surgical modification of soft palate, uvula, and pharyngeal tissues. Non-surgical options include CPAP therapy and oral appliances.
Overview of Sleep Apnea Treatment
Addressing Obstructive Sleep Apnea for Better Health
Obstructive Sleep Apnea (OSA) is a serious condition where breathing repeatedly stops and starts during sleep. DivinHeal offers advanced diagnostic Sleep Studies and effective surgical and non-surgical treatments for OSA, including Uvulopalatopharyngoplasty (UPPP). Our goal is to restore restful sleep, improve oxygenation, and mitigate associated health risks like cardiovascular disease and stroke.
- Diagnosis: In-depth Sleep Study (Polysomnography) to confirm OSA and determine severity.
- Treatment Goals: Widen airways, reduce snoring, eliminate apnea events, and improve sleep quality.
- Techniques: UPPP involves surgical modification of soft palate, uvula, and pharyngeal tissues. Non-surgical options include CPAP therapy and oral appliances.
Treatment Overview
<h2>Overview of Sleep Apnea Treatment</h2><h3>Addressing Obstructive Sleep Apnea for Better Health</h3><p>Obstructive Sleep Apnea (OSA) is a serious condition where breathing repeatedly stops and starts during sleep. DivinHeal offers advanced diagnostic Sleep Studies and effective surgical and non-surgical treatments for OSA, including Uvulopalatopharyngoplasty (UPPP). Our goal is to restore restful sleep, improve oxygenation, and mitigate associated health risks like cardiovascular disease and stroke.</p><ul><li><b>Diagnosis:</b> In-depth Sleep Study (Polysomnography) to confirm OSA and determine severity.</li><li><b>Treatment Goals:</b> Widen airways, reduce snoring, eliminate apnea events, and improve sleep quality.</li><li><b>Techniques:</b> UPPP involves surgical modification of soft palate, uvula, and pharyngeal tissues. Non-surgical options include CPAP therapy and oral appliances.</li></ul>
Procedures
<h2>Procedure Details: How Sleep Apnea Surgery (UPPP) is Performed</h2><p>Uvulopalatopharyngoplasty (UPPP) is a surgical procedure typically performed under general anesthesia. The steps involved are:</p><h3>1. Anesthesia Administration</h3><p>You will be given general anesthesia to ensure you are fully asleep and pain-free throughout the surgery.</p><h3>2. Oral Examination and Preparation</h3><p>The surgeon will carefully examine the oral cavity and throat to identify the specific areas of obstruction that need to be addressed.</p><h3>3. Tissue Removal and Reshaping</h3><p>The core of the UPPP involves surgically removing or reshaping various tissues in the back of the throat:</p><ul><li><b>Uvula Reduction:</b> The small, dangling tissue at the back of the throat (uvula) may be partially removed or trimmed.</li><li><b>Soft Palate Resection:</b> Excess tissue from the soft palate, the fleshy part at the back of the roof of the mouth, is removed to widen the airway.</li><li><b>Tonsillectomy/Adenoidectomy (if needed):</b> If the tonsils and/or adenoids are enlarged and contribute to the obstruction, they will be removed as part of the procedure.</li><li><b>Pharyngeal Tissue Trimming:</b> Redundant tissue along the pharyngeal arches (the folds on either side of the throat) may also be trimmed.</li></ul><h3>4. Wound Closure</h3><p>The remaining tissues are carefully sutured (stitched) to create a wider, more stable airway. Dissolvable sutures are typically used.</p><h3>5. Post-Operative Monitoring</h3><p>After the surgery, you will be moved to a recovery room for close monitoring as you wake up from anesthesia. Your breathing and vital signs will be continuously checked.</p><h3>Sleep Study (Polysomnography)</h3><p>A sleep study is a non-invasive diagnostic procedure performed either overnight in a sleep lab or at home. Sensors are attached to your body to record brain activity (EEG), eye movements (EOG), muscle activity (EMG), heart rate (ECG), airflow, blood oxygen levels, and breathing effort. This data is then analyzed by a sleep specialist to diagnose sleep disorders like OSA and determine their severity.</p>
Benefits
<h2>Benefits of Sleep Apnea Surgery (UPPP) and Effective Sleep Apnea Treatment</h2><h3>Experience a Healthier, More Restorative Life</h3><ul><li><b>Significant Reduction in OSA Severity:</b> UPPP can dramatically decrease the Apnea-Hypopnea Index (AHI), leading to fewer breathing pauses during sleep.</li><li><b>Elimination or Reduction of Snoring:</b> A major benefit for patients and their partners, improving overall sleep environment.</li><li><b>Improved Sleep Quality:</b> Patients report feeling more rested and energized, leading to better daytime functioning.</li><li><b>Enhanced Quality of Life:</b> Reduced daytime sleepiness, improved concentration, and mood.</li><li><b>Lowered Health Risks:</b> Decreases the risk of OSA-related comorbidities like hypertension, heart disease, stroke, and diabetes.</li><li><b>Alternative to CPAP:</b> Offers a permanent or long-term solution for those who cannot tolerate or prefer not to use CPAP machines.</li><li><b>Better Oxygenation:</b> Improved breathing during sleep leads to healthier blood oxygen levels.</li></ul>
Recovery Information
<h2>Sleep Apnea Surgery (UPPP) Recovery Time and Tips</h2><h3>Your Path to Healing and Better Sleep</h3><p>Recovery from Sleep Apnea Surgery (UPPP) requires patience and adherence to post-operative instructions. While individual recovery times vary, most patients can expect significant improvement within a few weeks.</p><h3>Immediate Post-Operative Period (1-2 weeks)</h3><ul><li><b>Sore Throat and Discomfort:</b> Expect significant throat pain, similar to severe strep throat, which can last for 1-2 weeks. Pain medication will be prescribed.</li><li><b>Diet:</b> A soft diet is crucial initially, progressing to regular foods as tolerated. Avoid spicy, acidic, or crunchy foods.</li><li><b>Swelling:</b> Throat swelling is common and can temporarily worsen snoring or breathing, especially in the first few days.</li><li><b>Activity:</b> Rest is important. Avoid strenuous activities, heavy lifting, and bending over.</li><li><b>Hydration:</b> Drink plenty of fluids to aid healing and keep the throat moist.</li></ul><h3>Intermediate Recovery (2-4 weeks)</h3><ul><li><b>Pain Reduction:</b> Throat pain should significantly subside.</li><li><b>Return to Light Activities:</b> Most patients can return to light work or daily activities, avoiding heavy exertion.</li><li><b>Voice Changes:</b> Your voice may temporarily sound different due to swelling.</li></ul><h3>Long-term Recovery & Follow-up</h3><ul><li><b>Full Healing:</b> Complete tissue healing typically takes 4-6 weeks, though benefits regarding sleep and snoring may be felt sooner.</li><li><b>Follow-up Sleep Study:</b> A post-operative sleep study is often recommended several months after surgery to assess the effectiveness of the UPPP.</li><li><b>Lifestyle Modifications:</b> Maintaining a healthy weight, avoiding alcohol and sedatives before sleep, and consistent sleep hygiene are crucial for long-term success.</li></ul><p>DivinHeal's care coordinators provide comprehensive guidance throughout your recovery, ensuring you have the support needed for optimal healing and sustainable results.</p>

Myringotomy with Grommet
Treatment Price
$800.00 USDThe primary goal of Myringotomy with Grommet treatment is to restore normal hearing function, prevent recurrent middle ear infections, and promote healthy development, especially in young children. The procedure involves a minimally invasive surgical technique under general anesthesia, where a small incision is made in the eardrum to suction out accumulated fluid, followed by the insertion of a temporary grommet. This tube acts as an artificial Eustachian tube, allowing air into the middle ear and preventing fluid buildup.
The primary goal of Myringotomy with Grommet treatment is to restore normal hearing function, prevent recurrent middle ear infections, and promote healthy development, especially in young children. The procedure involves a minimally invasive surgical technique under general anesthesia, where a small incision is made in the eardrum to suction out accumulated fluid, followed by the insertion of a temporary grommet. This tube acts as an artificial Eustachian tube, allowing air into the middle ear and preventing fluid buildup.
Treatment Overview
The primary goal of Myringotomy with Grommet treatment is to restore normal hearing function, prevent recurrent middle ear infections, and promote healthy development, especially in young children. The procedure involves a minimally invasive surgical technique under general anesthesia, where a small incision is made in the eardrum to suction out accumulated fluid, followed by the insertion of a temporary grommet. This tube acts as an artificial Eustachian tube, allowing air into the middle ear and preventing fluid buildup.
Procedures
Myringotomy with Grommet is performed under general anesthesia, usually as a day-case procedure. The surgeon uses a microscope to gain a clear view of the eardrum. A small incision (myringotomy) is made in the eardrum. Any fluid present in the middle ear is then suctioned out. Finally, a tiny, hollow grommet (tympanostomy tube) is carefully inserted into the incision, ensuring it sits securely to maintain ventilation. The incision usually closes around the grommet, holding it in place until it naturally extrudes.
Benefits
<h2>Benefits of Myringotomy with Grommet Treatment</h2><ul><li><strong>Improved Hearing:</strong> The most immediate and significant benefit is the restoration of normal hearing, especially crucial for children's speech and cognitive development.</li><li><strong>Reduced Ear Infections:</strong> Grommets help to ventilate the middle ear, significantly decreasing the frequency and severity of recurrent acute otitis media.</li><li><strong>Better Quality of Life:</strong> Alleviates discomfort, pain, and sleep disturbances associated with chronic ear problems.</li><li><strong>Enhanced Speech and Language Development:</strong> For children, improved hearing directly supports clearer speech and better academic performance.</li><li><strong>Prevention of Long-Term Complications:</strong> Reduces the risk of permanent eardrum damage, middle ear scarring, and other serious complications associated with untreated glue ear.</li></ul>
Recovery Information
<h2>Myringotomy with Grommet Recovery Time and Tips</h2><h3>Immediate Post-Procedure Care</h3><p>Recovery from Myringotomy with Grommet is typically quick, as it is a minor surgical procedure. Patients, especially children, usually recover fully within a day or two. There might be some mild discomfort or dizziness immediately after the surgery, but significant pain is uncommon. Ear drops may be prescribed to prevent infection.</p><h3>Long-Term Recovery and Care</h3><ul><li><strong>Water Precautions:</strong> It is crucial to keep the ears dry to prevent infection while the grommets are in place. This often involves using earplugs or a swim cap during bathing, showering, and swimming.</li><li><strong>Activity:</strong> Most normal activities can be resumed within a few days, but strenuous activities or contact sports might be restricted for a short period.</li><li><strong>Grommet Extrusion:</strong> Grommets usually fall out on their own as the eardrum heals, typically within 6 to 18 months. Regular follow-up appointments with an ENT specialist are essential to monitor the grommets and ensure the ear is healing properly.</li><li><strong>Monitoring Hearing:</strong> Regular hearing tests may be recommended to track progress and ensure the underlying issue has resolved.</li></ul>

Microlaryngeal Surgery (Voice)
Treatment Price
$2000.00 USDMicrolaryngeal Surgery (MLS) is a delicate surgical intervention designed to diagnose and treat lesions affecting the vocal cords, such as polyps, nodules, cysts, granulomas, or early-stage cancers. Utilizing a surgical microscope for enhanced magnification, surgeons achieve exceptional accuracy, enabling the precise removal or modification of tissue while preserving surrounding healthy vocal cord structures. The overarching objective is to improve or restore voice quality, alleviate discomfort, and ensure proper vocal fold vibration, which is fundamental for clear speech and singing. DivinHeal connects patients with leading Otolaryngologists and Laryngologists who specialize in these intricate procedures, ensuring world-class care.
Microlaryngeal Surgery (MLS) is a delicate surgical intervention designed to diagnose and treat lesions affecting the vocal cords, such as polyps, nodules, cysts, granulomas, or early-stage cancers. Utilizing a surgical microscope for enhanced magnification, surgeons achieve exceptional accuracy, enabling the precise removal or modification of tissue while preserving surrounding healthy vocal cord structures. The overarching objective is to improve or restore voice quality, alleviate discomfort, and ensure proper vocal fold vibration, which is fundamental for clear speech and singing. DivinHeal connects patients with leading Otolaryngologists and Laryngologists who specialize in these intricate procedures, ensuring world-class care.
Treatment Overview
Microlaryngeal Surgery (MLS) is a delicate surgical intervention designed to diagnose and treat lesions affecting the vocal cords, such as polyps, nodules, cysts, granulomas, or early-stage cancers. Utilizing a surgical microscope for enhanced magnification, surgeons achieve exceptional accuracy, enabling the precise removal or modification of tissue while preserving surrounding healthy vocal cord structures. The overarching objective is to improve or restore voice quality, alleviate discomfort, and ensure proper vocal fold vibration, which is fundamental for clear speech and singing. DivinHeal connects patients with leading Otolaryngologists and Laryngologists who specialize in these intricate procedures, ensuring world-class care.
Procedures
Microlaryngeal surgery is performed under general anesthesia. The patient is positioned with the head extended, and a rigid laryngoscope is carefully inserted through the mouth to provide a direct view of the vocal cords. The laryngoscope is suspended, leaving both hands of the surgeon free. A surgical microscope is then brought into position, providing highly magnified and illuminated views of the delicate vocal fold structures. Using specialized micro-instruments, such as micro-forceps, micro-scissors, dissectors, or sometimes a laser, the surgeon precisely removes or modifies the identified lesion while meticulously preserving the surrounding healthy tissue. The goal is to excise the pathology with minimal impact on the vocal cord's vibratory function. Once the procedure is complete, the instruments and laryngoscope are carefully removed, and the patient is woken from anesthesia.
Benefits
<h2>Benefits of Microlaryngeal Surgery (Voice)</h2><ul><li><h3>Voice Restoration & Improvement</h3><p>The primary benefit is the significant improvement or complete restoration of voice quality, pitch, and projection, allowing patients to communicate more effectively and comfortably.</p></li><li><h3>Precise Lesion Removal</h3><p>The use of microscopic visualization ensures highly accurate removal or modification of vocal cord lesions while preserving the maximum amount of healthy tissue, crucial for vocal function.</p></li><li><h3>Minimally Invasive Approach</h3><p>As an endoscopic procedure, MLS avoids external incisions, leading to quicker healing, less discomfort, and no visible scarring.</p></li><li><h3>Accurate Diagnosis</h3><p>MLS often includes a biopsy of suspicious lesions, providing definitive histological diagnosis for conditions like early-stage laryngeal cancer.</p></li><li><h3>Enhanced Quality of Life</h3><p>By resolving voice problems, MLS can significantly improve a patient's professional performance, social interactions, and overall mental well-being.</p></li><li><h3>High Success Rate</h3><p>For benign lesions, MLS boasts a high success rate in resolving symptoms and preventing recurrence when combined with proper vocal hygiene and voice therapy.</p></li></ul>
Recovery Information
<h2>Microlaryngeal Surgery (Voice) Recovery Time and Tips</h2><ul><li><h3>Immediate Post-Operative Period (First 1-7 Days)</h3><p>Strict vocal rest is paramount. This means absolutely no talking, whispering, or even clearing your throat for a prescribed period (typically 3-7 days, depending on the extent of surgery). Hydration is key. You may experience mild throat discomfort or a sensation of a lump in the throat, managed with prescribed pain relief.</p></li><li><h3>Gradual Voice Reintroduction (Weeks 1-3)</h3><p>After the strict vocal rest, your surgeon will advise on a gradual reintroduction of voice use. This often involves very short periods of speaking at a normal conversational volume. Whispering should be avoided as it can strain the vocal cords more than gentle speaking. Professional voice therapy typically begins during this phase.</p></li><li><h3>Voice Therapy & Rehabilitation</h3><p>Voice therapy is often a crucial component of <a href="microlaryngeal-surgery-voice-recovery-time-and-tips">Microlaryngeal Surgery (Voice) recovery time and tips</a>, helping patients learn proper vocal hygiene, breath support, and speaking techniques to prevent future issues and optimize vocal outcome.</p></li><li><h3>Full Recovery & Long-term Care (Weeks 4-12+)</h3><p>While some voice improvement is immediate, full vocal recovery can take several weeks to months. Continued voice therapy, avoidance of vocal abuse (shouting, prolonged talking), irritants (smoking, excessive caffeine/alcohol), and managing underlying conditions (e.g., GERD) are vital for long-term vocal health. Regular follow-up with your laryngologist is recommended.</p></li></ul>
Meet Our Doctors
Meet our team of highly qualified and experienced medical professionals dedicated to providing the best healthcare services.

Dr. Amit Kalsotra
Sr. Consultant - Anaesthesia, Critical Care & Pain Management
Anaesthesia, Critical Care, Pain Management
New Delhi
15+ Years
Experience
Artemis Hospital
Hospital
1500
Fees