Centres Of Excellence
Our Centres of Excellence bring together multidisciplinary teams to deliver precise diagnosis, advanced treatments, and superior outcomes across a wide spectrum of medical specialties.

Related Links
Doctors For Treatment in Similar Locations
Best Hospital Near by for treatment
Other Treatments Nearby
Treatments in India for Visitors
Doctors For Treatment in Similar Locations
Best Hospital Near by for treatment
Related Links
- Urology cost in Hyderabad
- Urology cost in India
- Urology cost in Mumbai
- Urology cost in New Delhi
- Urology cost in Pune
- Urology Success Rate in Bengaluru
- Urology Success Rate in Chennai
- Urology Success Rate in Haryana
- Urology Success Rate in Hyderabad
- Urology Success Rate in India
- Urology Success Rate in Mumbai
- Urology Success Rate in New Delhi
- Urology Success Rate in Pune
Other Treatments Nearby
Treatments in India for Visitors
- Urology Treatment in Bengaluru for Nigeria
- Urology Treatment in Bengaluru for UAE
- Urology Treatment in Chennai for Bangladesh
- Urology Treatment in Chennai for Ethiopia
- Urology Treatment in Chennai for Iraq
- Urology Treatment in Chennai for Nigeria
- Urology Treatment in Chennai for UAE
- Urology Treatment in Gurugram for Bangladesh
- Urology Treatment in Gurugram for Ethiopia
- Urology Treatment in Gurugram for Iraq
- Urology Treatment in Gurugram for Nigeria
- Urology Treatment in Gurugram for UAE
- Urology Treatment in Hyderabad for Bangladesh
- Urology Treatment in Hyderabad for Ethiopia
- Urology Treatment in Hyderabad for Iraq
- Urology Treatment in Hyderabad for Nigeria
- Urology Treatment in Hyderabad for UAE
- Urology Treatment in India for Bangladesh
- Urology Treatment in India for Ethiopia
- Urology Treatment in India for Iraq
- Urology Treatment in India for Nigeria
- Urology Treatment in India for UAE
- Urology Treatment in Mumbai for Bangladesh
- Urology Treatment in Mumbai for Ethiopia
- Urology Treatment in Mumbai for Iraq
- Urology Treatment in Mumbai for Nigeria
- Urology Treatment in Mumbai for UAE
- Urology Treatment in New Delhi for Bangladesh
- Urology Treatment in New Delhi for Ethiopia
- Urology Treatment in New Delhi for Iraq
- Urology Treatment in New Delhi for Nigeria
- Urology Treatment in New Delhi for UAE
- Urology Treatment in Pune for Bangladesh
- Urology Treatment in Pune for Ethiopia
- Urology Treatment in Pune for Iraq
- Urology Treatment in Pune for Nigeria
- Urology Treatment in Pune for UAE
Related Treatments

Cystoscopy & TURBT (Bladder Tumor Resection)
Treatment Price
$3500.00 USDOverview of Cystoscopy & TURBT
Cystoscopy & TURBT serves a dual purpose: it's a diagnostic tool allowing direct visualization of the bladder for any abnormalities, and a therapeutic intervention to remove bladder tumors. This procedure is the cornerstone for managing non-muscle invasive bladder cancer (NMIBC), aiming to achieve complete tumor resection, accurate staging, and prevent recurrence. It's often followed by intravesical therapy.
Overview of Cystoscopy & TURBT
Cystoscopy & TURBT serves a dual purpose: it's a diagnostic tool allowing direct visualization of the bladder for any abnormalities, and a therapeutic intervention to remove bladder tumors. This procedure is the cornerstone for managing non-muscle invasive bladder cancer (NMIBC), aiming to achieve complete tumor resection, accurate staging, and prevent recurrence. It's often followed by intravesical therapy.
Treatment Overview
<h2>Overview of Cystoscopy & TURBT</h2><p>Cystoscopy & TURBT serves a dual purpose: it's a diagnostic tool allowing direct visualization of the bladder for any abnormalities, and a therapeutic intervention to remove bladder tumors. This procedure is the cornerstone for managing non-muscle invasive bladder cancer (NMIBC), aiming to achieve complete tumor resection, accurate staging, and prevent recurrence. It's often followed by intravesical therapy.</p>
Procedures
Cystoscopy & TURBT is performed under general or spinal anesthesia. The patient is placed in the lithotomy position. The surgeon inserts a cystoscope, a thin, lighted tube with a camera, through the urethra into the bladder. The bladder is then filled with a sterile solution to allow for clear visualization of the entire bladder lining. Any suspicious growths, lesions, or tumors are identified. Using specialized instruments passed through the cystoscope, the tumor is carefully resected (cut away) from the bladder wall in layers. This ensures that a sufficient amount of tissue is obtained for pathological analysis, including muscle tissue if needed for staging. After resection, any bleeding vessels are cauterized to prevent hemorrhage. The resected tissue fragments are then removed from the bladder, and the bladder is irrigated. In some cases, a single dose of chemotherapy (e.g., Mitomycin C) may be instilled into the bladder immediately after TURBT to reduce the risk of recurrence. A urinary catheter may be left in place temporarily to drain urine and irrigate the bladder.
Benefits
<h2>Benefits of Cystoscopy & TURBT</h2><ul><li><h3>Accurate Diagnosis & Staging</h3><p>TURBT allows for direct visualization and removal of bladder tumors, providing crucial tissue samples for accurate pathological diagnosis, grading, and staging of bladder cancer. This precision is fundamental for guiding subsequent treatment decisions.</p></li><li><h3>Therapeutic Removal of Tumors</h3><p>For non-muscle invasive bladder cancer, TURBT is often curative, completely removing the tumor and offering immediate relief from symptoms like hematuria. It's a primary therapeutic intervention.</p></li><li><h3>Minimally Invasive Approach</h3><p>As an endoscopic procedure, TURBT avoids large incisions, leading to less post-operative pain, shorter hospital stays, and quicker recovery compared to open surgery.</p></li><li><h3>Prevention of Progression</h3><p>Timely and complete TURBT, especially when followed by intravesical therapy, significantly reduces the risk of bladder cancer recurrence and progression to more invasive forms.</p></li><li><h3>Improved Quality of Life</h3><p>By effectively treating bladder tumors, patients can experience an improved quality of life, free from the symptoms and anxieties associated with untreated bladder cancer.</p></li></ul>
Recovery Information
<h2>Cystoscopy & TURBT Recovery Time and Tips</h2><p>The <span>Cystoscopy & TURBT (Bladder Tumor Resection) recovery time and tips</span> are crucial for a smooth return to daily activities. Immediately after the procedure, you may experience some discomfort, urgency to urinate, and blood in your urine, which usually subsides within a few days to a week.</p><h3>Expected Recovery Timeline:</h3><ul><li><strong>Hospital Stay:</strong> Typically 1-2 days, allowing for monitoring and initial pain management.</li><li><strong>Catheter Removal:</strong> If a catheter was inserted, it is usually removed within 1-2 days post-procedure.</li><li><strong>Return to Light Activities:</strong> Most patients can resume light activities within 1-2 weeks.</li><li><strong>Full Recovery:</strong> Complete recovery, including resolution of urinary symptoms, may take 3-4 weeks. Strenuous activities and heavy lifting should be avoided for several weeks to prevent bleeding.</li></ul><h3>Recovery Tips:</h3><ul><li><strong>Hydration:</strong> Drink plenty of fluids to flush your bladder and reduce the risk of infection.</li><li><strong>Avoid Strenuous Activity:</strong> Refrain from heavy lifting, vigorous exercise, and straining during bowel movements for at least 2-4 weeks.</li><li><strong>Monitor Urine:</strong> Report any excessive bleeding, fever, chills, or inability to urinate to your doctor immediately.</li><li><strong>Medication:</strong> Take prescribed pain relievers and antibiotics as directed.</li><li><strong>Follow-up:</strong> Adhere strictly to your scheduled follow-up appointments and cystoscopies, which are vital for monitoring for recurrence and long-term management.</li></ul>
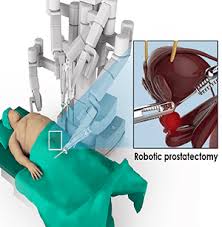
Robotic Prostatectomy
Treatment Price
$7000.00 USDThe primary goal of Robotic Prostatectomy is to surgically remove cancerous prostate tissue while preserving surrounding vital structures like nerves responsible for erectile function and the bladder sphincter for urinary continence. This advanced procedure, often performed using the da Vinci Surgical System, offers a precise approach to prostate cancer treatment, aiming for complete cancer removal with minimal impact on quality of life.
The primary goal of Robotic Prostatectomy is to surgically remove cancerous prostate tissue while preserving surrounding vital structures like nerves responsible for erectile function and the bladder sphincter for urinary continence. This advanced procedure, often performed using the da Vinci Surgical System, offers a precise approach to prostate cancer treatment, aiming for complete cancer removal with minimal impact on quality of life.
Treatment Overview
The primary goal of Robotic Prostatectomy is to surgically remove cancerous prostate tissue while preserving surrounding vital structures like nerves responsible for erectile function and the bladder sphincter for urinary continence. This advanced procedure, often performed using the da Vinci Surgical System, offers a precise approach to prostate cancer treatment, aiming for complete cancer removal with minimal impact on quality of life.
Procedures
Robotic Prostatectomy is performed under general anesthesia. The surgeon makes several small (0.5-1 cm) incisions in the lower abdomen. Through these incisions, ports are inserted for the robotic instruments and a high-definition camera. The surgeon sits at a console a few feet away, controlling the robotic arms that hold the surgical tools. The robotic system provides a magnified, 3D view of the surgical area, allowing for extremely precise dissection. The prostate gland, along with the seminal vesicles, is carefully dissected free from surrounding tissues. Nerve-sparing techniques are employed where appropriate to preserve the neurovascular bundles responsible for erectile function. Lymph nodes may also be removed if indicated by the cancer's aggressiveness or stage. After the prostate is removed, the bladder is reconnected to the urethra, and the small incisions are closed. A urinary catheter is typically left in place for 1-3 weeks to allow for healing of the connection between the bladder and urethra. The entire procedure usually takes 2-4 hours.
Benefits
<h2>Key Benefits of Robotic Prostatectomy</h2><ul><li><h3>Minimally Invasive Approach</h3><p>Compared to traditional open surgery, Robotic Prostatectomy involves several small incisions instead of one large one, leading to less post-operative pain, reduced blood loss, and smaller, less noticeable scars. This translates to a more comfortable and aesthetically pleasing recovery.</p></li><li><h3>Enhanced Surgical Precision</h3><p>The robotic system provides the surgeon with a magnified 3D view and instruments with a greater range of motion than the human wrist. This allows for incredibly precise dissection and suturing, crucial for intricate procedures like nerve-sparing, which is vital for preserving erectile function and urinary continence, significantly improving the Robotic Prostatectomy success rate.</p></li><li><h3>Faster Recovery Time</h3><p>Patients undergoing Robotic Prostatectomy typically experience a shorter hospital stay, quicker return to normal activities, and a faster overall Robotic Prostatectomy recovery time. This is due to less trauma to tissues and reduced surgical stress on the body.</p></li><li><h3>Reduced Risk of Complications</h3><p>The precision and minimally invasive nature of the procedure can lead to a lower risk of certain complications such as infection, blood transfusions, and prolonged pain, enhancing safety and overall patient experience.</p></li><li><h3>Improved Functional Outcomes</h3><p>With careful nerve-sparing techniques facilitated by robotic assistance, there is an increased potential for better preservation of urinary continence and erectile function post-surgery, critical aspects of a patient's quality of life after Robotic Prostatectomy treatment.</p></li><li><h3>Global Affordability and Quality with DivinHeal</h3><p>Through DivinHeal, patients can access these advanced benefits at an affordable Robotic Prostatectomy cost in world-class hospitals in India, ensuring high-quality care without financial burden.</p></li></ul>
Recovery Information
<h2>Robotic Prostatectomy Recovery Time and Tips</h2><ul><li><h3>Immediate Post-Operative Period (Hospital Stay)</h3><p>Patients typically stay in the hospital for 2-5 days following Robotic Prostatectomy. During this time, a urinary catheter will be in place to allow the bladder to heal. Pain management will be provided, and early mobilization (walking) is encouraged to prevent complications like blood clots.</p></li><li><h3>First Few Weeks at Home (Catheter Removal & Initial Healing)</h3><p>The urinary catheter is usually removed 1-3 weeks after surgery. It's common to experience some urinary leakage (incontinence) initially, which gradually improves. Activity should be light, avoiding heavy lifting or strenuous exercise. Focus on hydration and a balanced diet. DivinHeal provides comprehensive support during this crucial phase, offering recovery tips and connecting you with resources for continence management.</p></li><li><h3>Long-Term Recovery & Rehabilitation</h3><p>Full recovery of urinary control and erectile function can take several months to up to two years, varying significantly among individuals. Pelvic floor exercises (Kegels) are highly recommended to aid in regaining continence. Erectile dysfunction can be managed with medication, vacuum devices, or injections, often guided by your specialist. Regular follow-ups are essential to monitor PSA levels and ensure the long-term Robotic Prostatectomy success rate. DivinHeal facilitates these follow-ups with top oncologists for Robotic Prostatectomy.</p></li><li><h3>Emotional and Psychological Support</h3><p>Dealing with cancer and surgical recovery can be emotionally challenging. Support groups, counseling, and open communication with your healthcare team are vital. DivinHeal offers access to resources for emotional well-being throughout your Robotic Prostatectomy treatment journey.</p></li></ul>

Robotic Kidney Transplant
Treatment Price
$15000.00 USDThe primary goal of Robotic Kidney Transplant is to replace a failing kidney with a healthy donor kidney, restoring kidney function and significantly improving a patient's quality of life. This advanced procedure leverages state-of-the-art robotic systems to facilitate meticulous dissection, precise vessel anastomosis, and accurate kidney placement through small incisions, minimizing trauma and optimizing surgical outcomes. DivinHeal connects patients with leading transplant centers globally, specializing in these sophisticated techniques.
The primary goal of Robotic Kidney Transplant is to replace a failing kidney with a healthy donor kidney, restoring kidney function and significantly improving a patient's quality of life. This advanced procedure leverages state-of-the-art robotic systems to facilitate meticulous dissection, precise vessel anastomosis, and accurate kidney placement through small incisions, minimizing trauma and optimizing surgical outcomes. DivinHeal connects patients with leading transplant centers globally, specializing in these sophisticated techniques.
Treatment Overview
The primary goal of Robotic Kidney Transplant is to replace a failing kidney with a healthy donor kidney, restoring kidney function and significantly improving a patient's quality of life. This advanced procedure leverages state-of-the-art robotic systems to facilitate meticulous dissection, precise vessel anastomosis, and accurate kidney placement through small incisions, minimizing trauma and optimizing surgical outcomes. DivinHeal connects patients with leading transplant centers globally, specializing in these sophisticated techniques.
Procedures
The Robotic Kidney Transplant procedure involves several meticulous steps. After general anesthesia, the patient's abdomen is prepared, and several small incisions (usually 8-12 mm) are made. Trocar ports are inserted through these incisions, through which specialized robotic instruments and a high-definition 3D camera are introduced. The surgeon controls the robotic arms from a console, gaining a magnified view and precise manipulation capabilities. The donor kidney, typically from a living or deceased donor, is prepared externally. Internally, the recipient's iliac vessels (artery and vein) are identified and prepared for anastomosis. The donor kidney is then carefully inserted into the abdominal cavity, often through a slightly larger incision (5-7 cm) in the lower abdomen or umbilical area. The robotic arms are then used to meticulously connect the renal artery of the new kidney to the recipient's iliac artery and the renal vein to the iliac vein. Finally, the ureter of the new kidney is connected to the recipient's bladder. Once blood flow is established and the kidney begins to produce urine, the incisions are closed.
Benefits
<h2>Benefits of Robotic Kidney Transplant</h2><ul><li><strong>Minimally Invasive:</strong> Smaller incisions lead to less pain, reduced scarring, and fewer wound-related complications.</li><li><strong>Faster Recovery:</strong> Patients typically experience a shorter hospital stay and a quicker return to daily activities compared to open surgery.</li><li><strong>Enhanced Precision:</strong> Robotic assistance allows surgeons greater dexterity, magnification, and 3D visualization, facilitating more accurate and delicate surgical maneuvers.</li><li><strong>Reduced Blood Loss:</strong> The precision of robotic instruments often results in less intraoperative blood loss.</li><li><strong>Lower Risk of Infection:</strong> Smaller incisions inherently reduce the risk of surgical site infections.</li><li><strong>Improved Quality of Life:</strong> A successful transplant liberates patients from dialysis, restoring kidney function and significantly enhancing their overall well-being and life expectancy.</li><li><strong>Access to Top Specialists:</strong> DivinHeal connects you with leading transplant surgeons globally who specialize in advanced robotic techniques, ensuring the highest quality of care and optimal **Robotic Kidney Transplant success rate**.</li></ul>
Recovery Information
<h2>Robotic Kidney Transplant Recovery Time and Tips</h2><p>The **Robotic Kidney Transplant recovery time** typically involves an initial hospital stay of about 5 to 7 days, during which patients are closely monitored for kidney function and signs of rejection. Post-discharge, the full recovery period can span several weeks to months, requiring careful adherence to medical advice and lifestyle adjustments.</p><h3>Key Recovery Aspects:</h3><ul><li><strong>Medication Adherence:</strong> Lifelong immunosuppressants are crucial to prevent organ rejection. Strict adherence to the medication schedule is paramount.</li><li><strong>Activity Restrictions:</strong> Strenuous activities, heavy lifting, and contact sports are generally restricted for the first few months to allow proper healing and to protect the new kidney.</li><li><strong>Diet and Hydration:</strong> A balanced, kidney-friendly diet and adequate hydration are essential. Dietary restrictions may vary based on individual needs and kidney function.</li><li><strong>Follow-up Appointments:</strong> Regular check-ups with the transplant team are vital for monitoring kidney function, adjusting medications, and detecting any complications early.</li><li><strong>Emotional Support:</strong> Adapting to a new lifestyle and lifelong medication can be challenging. Support groups, counseling, and family support play a significant role in emotional well-being during recovery.</li><li><strong>Infection Prevention:</strong> Due to immunosuppression, patients are at a higher risk of infection. Practicing good hygiene and avoiding crowded places are important tips.</li></ul><p>DivinHeal provides comprehensive guidance and support throughout your **Robotic Kidney Transplant recovery**, ensuring you have access to all necessary resources for a smooth and successful transition back to a healthy life.</p>
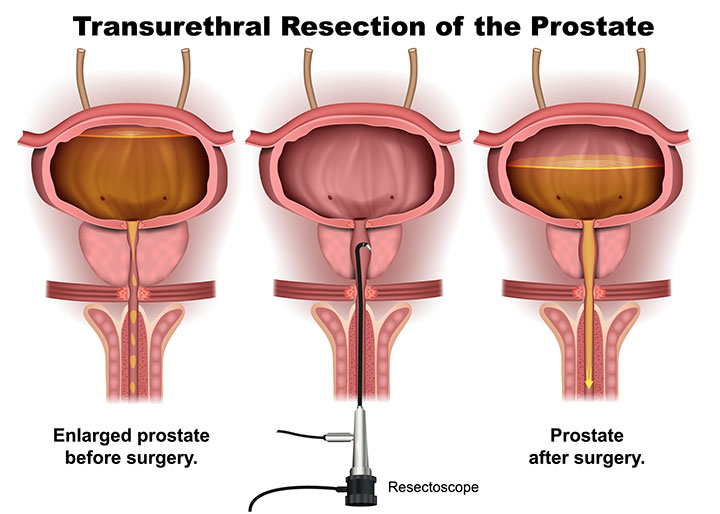
TURP (Transurethral Resection of Prostate)
Treatment Price
$2500.00 USDTURP is considered the 'gold standard' surgical treatment for BPH. The procedure aims to alleviate bothersome lower urinary tract symptoms (LUTS) such as frequent urination, urgency, weak stream, and nocturia, which arise when the enlarged prostate gland compresses the urethra. By resecting obstructing prostate tissue, TURP restores normal urine flow, enhancing bladder emptying and reducing associated complications.
TURP is considered the 'gold standard' surgical treatment for BPH. The procedure aims to alleviate bothersome lower urinary tract symptoms (LUTS) such as frequent urination, urgency, weak stream, and nocturia, which arise when the enlarged prostate gland compresses the urethra. By resecting obstructing prostate tissue, TURP restores normal urine flow, enhancing bladder emptying and reducing associated complications.
Treatment Overview
TURP is considered the 'gold standard' surgical treatment for BPH. The procedure aims to alleviate bothersome lower urinary tract symptoms (LUTS) such as frequent urination, urgency, weak stream, and nocturia, which arise when the enlarged prostate gland compresses the urethra. By resecting obstructing prostate tissue, TURP restores normal urine flow, enhancing bladder emptying and reducing associated complications.
Procedures
Transurethral Resection of the Prostate (TURP) is performed under general or spinal anesthesia. The urologist inserts a resectoscope – a thin, rigid tube with a light, camera, and a cutting tool – through the urethra into the bladder. Guided by the camera, the surgeon uses an electrical loop to carefully remove small pieces of the obstructing prostate tissue, widening the channel for urine flow. During the procedure, a sterile irrigating solution is continuously flushed through the bladder to wash away removed tissue fragments and keep the surgical field clear. Once enough tissue is removed, the resectoscope is withdrawn, and a catheter is inserted into the bladder to drain urine and continuously irrigate the bladder to prevent blood clots for a few days.
Benefits
<ul><li>Significant and lasting relief from bothersome urinary symptoms, improving quality of life.</li><li>Improved urine flow and complete bladder emptying.</li><li>Reduced risk of BPH-related complications such as urinary tract infections, bladder stones, and kidney damage.</li><li>Highly effective in restoring normal urinary function when conservative treatments fail.</li><li>Relatively safe procedure with a long track record of success.</li></ul>
Recovery Information
<h3>TURP Recovery Time and Tips</h3><p>The typical recovery period after TURP can vary, but most men experience significant improvement within 2-6 weeks. Immediately after the procedure, a catheter will be in place for 1-3 days to help with healing and drainage, and patients may notice blood in their urine, which is normal. Hospital stay is usually 1-3 days.</p><h4>Recovery Tips:</h4><ul><li><strong>Rest:</strong> Avoid strenuous activities, heavy lifting, and prolonged standing for several weeks.</li><li><strong>Hydration:</strong> Drink plenty of fluids to help flush the bladder and prevent blood clots.</li><li><strong>Diet:</strong> Maintain a healthy diet to prevent constipation, which can strain the surgical area.</li><li><strong>Medication:</strong> Take prescribed medications for pain and to prevent infection as directed.</li><li><strong>Avoid Irritants:</strong> Limit caffeine, alcohol, and spicy foods, which can irritate the bladder.</li><li><strong>Sexual Activity:</strong> Abstain from sexual activity for 4-6 weeks to allow for complete healing.</li><li><strong>Follow-up:</strong> Adhere to all post-operative appointments with your urologist for monitoring and care.</li></ul><p>While most men experience excellent relief from urinary symptoms, some may experience retrograde ejaculation (semen flows backward into the bladder during orgasm), a common and generally harmless side effect. DivinHeal ensures you receive comprehensive post-operative guidance and follow-up care for a smooth and successful recovery, supporting your long-term prostate health.</p>
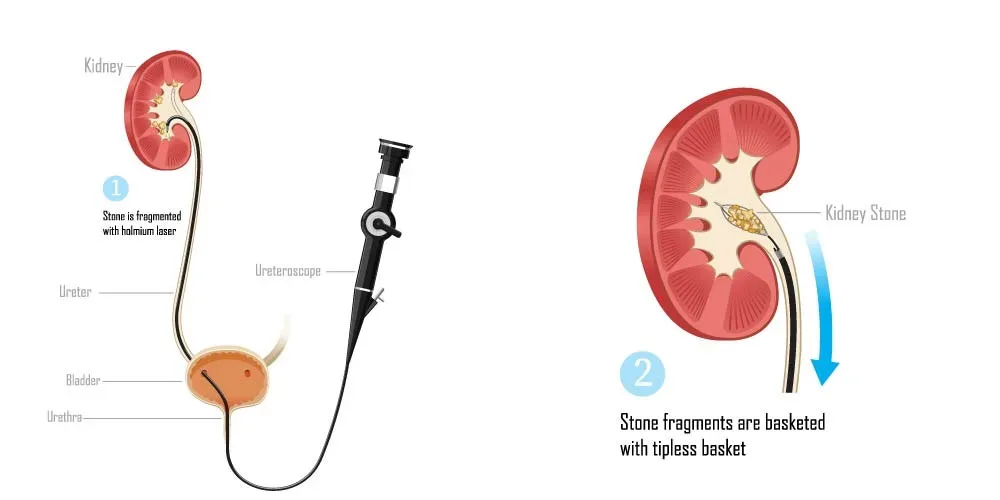
Laser Treatment for Kidney Stones (RIRS)
Treatment Price
$3500.00 USDThe primary goal of Laser Treatment for Kidney Stones (RIRS) is to effectively remove kidney stones located in the kidney or upper ureter using a flexible endoscope passed through the natural urinary opening. A laser is then used to fragment the stones, which are either removed or passed naturally. This advanced technique offers high success rates with reduced hospital stays and is a preferred choice for many due to its precision and safety.
The primary goal of Laser Treatment for Kidney Stones (RIRS) is to effectively remove kidney stones located in the kidney or upper ureter using a flexible endoscope passed through the natural urinary opening. A laser is then used to fragment the stones, which are either removed or passed naturally. This advanced technique offers high success rates with reduced hospital stays and is a preferred choice for many due to its precision and safety.
Treatment Overview
The primary goal of Laser Treatment for Kidney Stones (RIRS) is to effectively remove kidney stones located in the kidney or upper ureter using a flexible endoscope passed through the natural urinary opening. A laser is then used to fragment the stones, which are either removed or passed naturally. This advanced technique offers high success rates with reduced hospital stays and is a preferred choice for many due to its precision and safety.
Procedures
Laser Treatment for Kidney Stones (RIRS) involves several key steps: First, anesthesia (general or spinal) is administered to ensure patient comfort. The urologist then inserts a flexible ureteroscope through the urethra and bladder, carefully navigating it up the ureter to reach the kidney. Once the kidney stone is precisely located using direct visualization, a fine laser fiber (typically a Holmium:YAG laser) is passed through the working channel of the ureteroscope. The laser energy is then used to accurately fragment the stone into tiny pieces. These fragments are either retrieved using a specialized retrieval basket or are left to pass naturally through urine. A temporary ureteral stent may be placed at the end of the procedure to ensure proper drainage and prevent swelling. The procedure typically takes 60-90 minutes, depending on the stone's size and complexity.
Benefits
The benefits of Laser Treatment for Kidney Stones (RIRS) include its minimally invasive nature, leading to quicker recovery and less post-operative pain, fostering hope for a smooth experience. It offers high stone-free rates, even for complex cases or stones in difficult-to-reach locations, ensuring safety and efficacy. Patients experience a significantly reduced hospital stay, often discharged within 24 hours, and can typically resume normal activities much faster than with traditional surgery. It's a safe and effective method for removing kidney stones and preventing future complications, representing quality care.
Recovery Information
Recovery from Laser Treatment for Kidney Stones (RIRS) is generally swift and well-managed. Most patients can return to light activities within 2-3 days and resume normal routines within a week. You might experience some discomfort, blood in the urine, or frequent urination for a few days, which is a normal part of the healing process. A ureteral stent may be placed temporarily to aid healing and urine flow, usually removed after a week or two. DivinHeal provides comprehensive post-procedure guidelines and support to ensure a smooth and comfortable recovery, including advice on hydration, pain management, and follow-up care for your well-being.

HoLEP / Laser Prostate Surgery
Treatment Price
$4000.00 USDOverview of HoLEP / Laser Prostate Surgery
Precision Treatment for Benign Prostatic Hyperplasia (BPH)
HoLEP and other laser prostate surgeries represent a significant advancement in the treatment of Benign Prostatic Hyperplasia (BPH), a common condition affecting men as they age. The primary goal of these procedures is to precisely remove the obstructive prostate tissue that causes bothersome urinary symptoms, thereby restoring normal urine flow and significantly improving quality of life.
Minimally Invasive Techniques for Optimal Outcomes
- HoLEP (Holmium Laser Enucleation of the Prostate): Utilizes a holmium laser to precisely cut and remove excess prostate tissue that obstructs urine flow. The removed tissue is then morcellated and extracted, allowing for pathological examination. HoLEP is known for its ability to treat very large prostates and provides durable results comparable to open surgery, but with the advantages of a minimally invasive approach.
- GreenLight PVP (Photoselective Vaporization of the Prostate): Employs a high-powered laser to vaporize obstructing prostate tissue, creating a wider channel for urine flow. This technique is often favored for its minimal bleeding, making it suitable for patients on anticoagulants.
- ThuLEP (Thulium Laser Enucleation of the Prostate): Similar to HoLEP, ThuLEP uses a thulium laser for precise tissue removal and offers excellent outcomes with rapid recovery.
DivinHeal connects you with top urologists globally, offering these cutting-edge laser surgeries in accredited hospitals, ensuring safety, effectiveness, and a swift return to daily activities.
Overview of HoLEP / Laser Prostate Surgery
Precision Treatment for Benign Prostatic Hyperplasia (BPH)
HoLEP and other laser prostate surgeries represent a significant advancement in the treatment of Benign Prostatic Hyperplasia (BPH), a common condition affecting men as they age. The primary goal of these procedures is to precisely remove the obstructive prostate tissue that causes bothersome urinary symptoms, thereby restoring normal urine flow and significantly improving quality of life.
Minimally Invasive Techniques for Optimal Outcomes
- HoLEP (Holmium Laser Enucleation of the Prostate): Utilizes a holmium laser to precisely cut and remove excess prostate tissue that obstructs urine flow. The removed tissue is then morcellated and extracted, allowing for pathological examination. HoLEP is known for its ability to treat very large prostates and provides durable results comparable to open surgery, but with the advantages of a minimally invasive approach.
- GreenLight PVP (Photoselective Vaporization of the Prostate): Employs a high-powered laser to vaporize obstructing prostate tissue, creating a wider channel for urine flow. This technique is often favored for its minimal bleeding, making it suitable for patients on anticoagulants.
- ThuLEP (Thulium Laser Enucleation of the Prostate): Similar to HoLEP, ThuLEP uses a thulium laser for precise tissue removal and offers excellent outcomes with rapid recovery.
DivinHeal connects you with top urologists globally, offering these cutting-edge laser surgeries in accredited hospitals, ensuring safety, effectiveness, and a swift return to daily activities.
Treatment Overview
<h2>Overview of HoLEP / Laser Prostate Surgery</h2> <h3>Precision Treatment for Benign Prostatic Hyperplasia (BPH)</h3> <p>HoLEP and other laser prostate surgeries represent a significant advancement in the treatment of Benign Prostatic Hyperplasia (BPH), a common condition affecting men as they age. The primary goal of these procedures is to precisely remove the obstructive prostate tissue that causes bothersome urinary symptoms, thereby restoring normal urine flow and significantly improving quality of life.</p> <h3>Minimally Invasive Techniques for Optimal Outcomes</h3> <ul> <li><strong>HoLEP (Holmium Laser Enucleation of the Prostate):</strong> Utilizes a holmium laser to precisely cut and remove excess prostate tissue that obstructs urine flow. The removed tissue is then morcellated and extracted, allowing for pathological examination. HoLEP is known for its ability to treat very large prostates and provides durable results comparable to open surgery, but with the advantages of a minimally invasive approach.</li> <li><strong>GreenLight PVP (Photoselective Vaporization of the Prostate):</strong> Employs a high-powered laser to vaporize obstructing prostate tissue, creating a wider channel for urine flow. This technique is often favored for its minimal bleeding, making it suitable for patients on anticoagulants.</li> <li><strong>ThuLEP (Thulium Laser Enucleation of the Prostate):</strong> Similar to HoLEP, ThuLEP uses a thulium laser for precise tissue removal and offers excellent outcomes with rapid recovery.</li> </ul> <p>DivinHeal connects you with top urologists globally, offering these cutting-edge laser surgeries in accredited hospitals, ensuring safety, effectiveness, and a swift return to daily activities.</p>
Procedures
The HoLEP (Holmium Laser Enucleation of the Prostate) procedure typically involves the following steps: 1. **Anesthesia:** The patient is given general anesthesia or spinal anesthesia to ensure comfort and painlessness during the procedure. 2. **Cystoscopy and Sheath Insertion:** A resectoscope, a thin, telescopic instrument, is inserted into the urethra and advanced to the prostate. A working sheath is then advanced over the scope to create a channel for instruments and irrigation fluid. 3. **Laser Enucleation:** A holmium laser fiber is introduced through the resectoscope. The surgeon uses the laser to precisely cut and separate the enlarged inner prostate tissue (adenoma) from the outer prostatic capsule. This process is called enucleation and effectively removes the obstructive tissue in large, intact pieces. 4. **Tissue Mobilization:** Once the obstructive lobes of the prostate are enucleated, they are pushed into the bladder. 5. **Morcellation:** A morcellator, a specialized device, is then inserted into the bladder to chop the enucleated prostate tissue into small fragments, which are then suctioned out of the bladder and sent for pathological examination. This step is crucial to confirm the benign nature of the tissue and rule out prostate cancer. 6. **Hemostasis and Catheter Insertion:** After all the tissue is removed, the laser is used again to coagulate any bleeding vessels, ensuring minimal blood loss. A urinary catheter is then inserted to drain urine and continuously irrigate the bladder to prevent clot formation and facilitate healing. 7. **Recovery:** The catheter typically remains in place for 1-3 days, after which it is removed, and the patient's ability to urinate is assessed before discharge.
Benefits
<h2>Benefits of HoLEP / Laser Prostate Surgery</h2> <h3>Superior Outcomes and Enhanced Quality of Life for BPH Patients</h3> <p>Choosing HoLEP or other laser prostate surgeries offers a multitude of advantages for men suffering from benign prostatic hyperplasia (BPH). These advanced, minimally invasive techniques are designed to provide highly effective and durable relief from urinary symptoms, significantly improving patients' overall well-being.</p> <ul> <li><strong>Effective Symptom Relief:</strong> Provides immediate and significant improvement in urinary flow, reducing frequency, urgency, and incomplete bladder emptying.</li> <li><strong>Suitable for Any Prostate Size:</strong> HoLEP is particularly advantageous as it can effectively treat even very large prostates, a capability often limited in other minimally invasive procedures.</li> <li><strong>Minimally Invasive:</strong> Performed endoscopically through the urethra, avoiding external incisions, which means less pain and scarring.</li> <li><strong>Reduced Blood Loss:</strong> The laser seals blood vessels as it cuts, leading to significantly less bleeding compared to traditional TURP or open surgery. This makes it a safer option for patients on blood thinners.</li> <li><strong>Shorter Hospital Stay:</strong> Patients typically spend only 1-3 days in the hospital, allowing for a quicker return home.</li> <li><strong>Faster Recovery Time:</strong> The minimally invasive nature contributes to a quicker and more comfortable recovery period, allowing patients to resume normal activities sooner.</li> <li><strong>Durable Long-Term Results:</strong> HoLEP, in particular, offers excellent long-term outcomes with very low rates of re-operation, comparable to open prostatectomy.</li> <li><strong>Tissue for Pathology:</strong> The removed prostate tissue is available for pathological examination, which is crucial for ruling out prostate cancer.</li> <li><strong>Improved Quality of Life:</strong> By alleviating bothersome urinary symptoms, patients experience better sleep, increased activity levels, and a renewed sense of confidence and comfort.</li> <li><strong>Lower Risk of Complications:</strong> Compared to older surgical methods, laser prostate surgeries generally have a lower risk of complications such as TURP syndrome, infection, and prolonged catheterization.</li> </ul> <p>DivinHeal is committed to connecting you with expert urologists and hospitals that leverage these advanced laser technologies, ensuring you receive the highest quality care and achieve the best possible outcomes for your prostate health.</p>
Recovery Information
<h2>Recovery and Life After HoLEP / Laser Prostate Surgery</h2> <h3>A Smooth Path Back to Wellness and Active Living</h3> <p>The recovery process following HoLEP or other laser prostate surgeries is generally faster and more comfortable than traditional prostate procedures due to their minimally invasive nature. DivinHeal provides comprehensive guidance and support to ensure a smooth and effective recovery journey.</p> <ul> <li><strong>Immediate Post-operative Period (Hospital Stay):</strong> <ul> <li><strong>Catheter:</strong> You will typically have a urinary catheter for 1-3 days to help drain the bladder while the urethra heals.</li> <li><strong>Discomfort:</strong> Mild discomfort, bladder spasms, or a sensation of needing to urinate frequently is common and managed with medication.</li> <li><strong>Fluid Intake:</strong> Encouraged to drink plenty of fluids to flush the bladder.</li> <li><strong>Discharge:</strong> You will be discharged once the catheter is removed, you can urinate on your own, and any bleeding is minimal.</li> </ul> </li> <li><strong>First Few Weeks at Home:</strong> <ul> <li><strong>Urinary Symptoms:</strong> It's common to experience some urinary frequency, urgency, or mild burning during urination for several weeks. Intermittent blood in the urine, especially after physical activity, is also normal as the healing process continues.</li> <li><strong>Activity Restrictions:</strong> Avoid strenuous activities, heavy lifting, and prolonged sitting or driving for 2-4 weeks to prevent bleeding and aid healing. Light walking is encouraged.</li> <li><strong>Hydration:</strong> Continue to drink ample fluids to maintain bladder health.</li> <li><strong>Diet:</strong> A normal diet can be resumed, but avoiding caffeine and alcohol in the initial weeks can help reduce bladder irritation.</li> </ul> </li> <li><strong>Long-term Recovery (Months 1-3 and Beyond):</strong> <ul> <li><strong>Full Recovery:</strong> Most patients experience significant improvement in symptoms within 1-3 months. The full benefits of the surgery become apparent as swelling subsides completely.</li> <li><strong>Sexual Function:</strong> While ejaculation patterns may change (retrograde ejaculation is common), erectile function is typically preserved. Discuss any concerns with your urologist.</li> <li><strong>Follow-up:</strong> Regular follow-up appointments with your urologist are essential to monitor your recovery and long-term prostate health. DivinHeal assists in coordinating these appointments.</li> <li><strong>Lifestyle:</strong> Maintain a healthy lifestyle, including a balanced diet and regular exercise, to support overall wellness.</li> </ul> </li> </ul> <p>DivinHeal's post-operative support ensures you have access to medical advice and care coordination throughout your recovery, helping you regain your health and confidence with peace of mind. We emphasize hopeful outcomes and a return to an active, fulfilling life.</p>

Ureteroscopy (URS) for Stones
Treatment Price
$1500.00 USDUreteroscopy (URS) for Stones aims to remove or break down urinary tract stones that cause pain, obstruction, or infection. This endoscopic procedure involves the insertion of a ureteroscope to directly access the stone. Techniques may include stone retrieval with a basket or fragmentation using a laser (laser lithotripsy). DivinHeal connects you with top urologists and advanced facilities for safe and effective stone management.
Ureteroscopy (URS) for Stones aims to remove or break down urinary tract stones that cause pain, obstruction, or infection. This endoscopic procedure involves the insertion of a ureteroscope to directly access the stone. Techniques may include stone retrieval with a basket or fragmentation using a laser (laser lithotripsy). DivinHeal connects you with top urologists and advanced facilities for safe and effective stone management.
Treatment Overview
Ureteroscopy (URS) for Stones aims to remove or break down urinary tract stones that cause pain, obstruction, or infection. This endoscopic procedure involves the insertion of a ureteroscope to directly access the stone. Techniques may include stone retrieval with a basket or fragmentation using a laser (laser lithotripsy). DivinHeal connects you with top urologists and advanced facilities for safe and effective stone management.
Procedures
Ureteroscopy (URS) for Stones is performed under general or regional anesthesia. The patient is positioned, and the urologist inserts a thin, flexible or rigid ureteroscope through the urethra, bladder, and into the ureter or kidney. The scope provides real-time video images on a monitor. Once the stone is located, various techniques are employed: smaller stones may be grasped and removed with a basket, while larger stones are fragmented using a laser (laser lithotripsy). The fragments are then either retrieved or left to pass naturally. A temporary ureteral stent may be placed at the end of the procedure to keep the ureter open and facilitate drainage, which is typically removed in an outpatient setting a week or two later.
Benefits
<h2>Benefits of Ureteroscopy (URS) for Stones</h2><ul><li><h3>Minimally Invasive</h3><p>URS is an endoscopic procedure, meaning it involves no external incisions, leading to less pain, reduced scarring, and quicker healing compared to traditional open surgery.</p></li><li><h3>High Success Rate</h3><p>Ureteroscopy (URS) for Stones success rate is exceptionally high, often exceeding 90-95%, especially for stones located in the ureter or lower pole of the kidney, ensuring effective stone clearance.</p></li><li><h3>Direct Visualization and Treatment</h3><p>The urologist can directly visualize the stone, allowing for precise fragmentation with laser lithotripsy or direct retrieval, ensuring complete stone removal in many cases.</p></li><li><h3>Suitable for Various Stone Types and Sizes</h3><p>URS is effective for a wide range of stone sizes and compositions, including those resistant to ESWL, making it a versatile treatment option.</p></li><li><h3>Rapid Recovery</h3><p>Most patients experience a relatively quick Ureteroscopy (URS) for Stones recovery time, often returning to normal activities within a few days to a week.</p></li><li><h3>Reduced Hospital Stay</h3><p>URS is often performed as an outpatient procedure or requires only a short overnight hospital stay, contributing to lower Ureteroscopy (URS) for Stones treatment cost.</p></li><li><h3>Safe and Effective</h3><p>With advancements in technology and surgical techniques, URS is a very safe procedure with a low risk of serious complications, providing peace of mind for patients.</p></li></ul>
Recovery Information
<h2>Ureteroscopy (URS) for Stones Recovery Time and Tips</h2><h3>Immediate Post-Procedure</h3><p>After Ureteroscopy (URS) for Stones, you may experience some discomfort, including mild to moderate pain in the back or side, frequent urination, and blood in the urine. These symptoms are normal and typically subside within a few days. A temporary stent may be placed in the ureter to facilitate healing and stone fragment passage, which will be removed by your urologist usually within 1-2 weeks.</p><h3>Recovery Timeline</h3><p><ul><li><strong>Day 1-3:</strong> Rest at home, manage pain with prescribed medication. Drink plenty of fluids to help flush your system.</li><li><strong>Week 1:</strong> Most patients can resume light activities. Avoid strenuous exercise or heavy lifting.</li><li><strong>Week 2-4:</strong> Full Ureteroscopy (URS) for Stones recovery is usually achieved by this point, with the removal of the ureteral stent if one was placed. You can gradually return to all normal activities.</li></ul></p><h3>Recovery Tips for Ureteroscopy (URS) for Stones</h3><p><ul><li><strong>Hydration:</strong> Drink plenty of water (8-10 glasses a day) to help flush out any remaining stone fragments and prevent future stones.</li><li><strong>Medication:</strong> Take pain relievers and antibiotics (if prescribed) as directed by your urologist.</li><li><strong>Activity:</strong> Avoid strenuous physical activity, especially heavy lifting, for at least a week to prevent discomfort or dislodging the stent.</li><li><strong>Diet:</strong> Follow any dietary recommendations given by your doctor, particularly if your stones are related to specific dietary factors.</li><li><strong>Monitor Symptoms:</strong> Watch for signs of infection (fever, chills), severe pain not relieved by medication, or persistent heavy bleeding. Contact your doctor immediately if these occur.</li><li><strong>Follow-up:</strong> Attend all scheduled follow-up appointments, including for stent removal, to ensure proper healing and stone clearance.</li></ul></p>

Urethral Stricture Surgery (Urethroplasty)
Treatment Price
$3500.00 USDUrethroplasty involves surgically removing the scarred, narrowed segment of the urethra and reconnecting the healthy ends (excision and primary anastomosis) or widening the stricture using tissue grafts, often from the patient's buccal mucosa (mouth lining). The primary goal is to create a wide, stable urethral lumen that allows unobstructed urine flow, thereby alleviating symptoms like difficulty urinating, weak stream, frequent UTIs, and bladder discomfort. It is considered the gold standard for long-term stricture repair.
Urethroplasty involves surgically removing the scarred, narrowed segment of the urethra and reconnecting the healthy ends (excision and primary anastomosis) or widening the stricture using tissue grafts, often from the patient's buccal mucosa (mouth lining). The primary goal is to create a wide, stable urethral lumen that allows unobstructed urine flow, thereby alleviating symptoms like difficulty urinating, weak stream, frequent UTIs, and bladder discomfort. It is considered the gold standard for long-term stricture repair.
Treatment Overview
Urethroplasty involves surgically removing the scarred, narrowed segment of the urethra and reconnecting the healthy ends (excision and primary anastomosis) or widening the stricture using tissue grafts, often from the patient's buccal mucosa (mouth lining). The primary goal is to create a wide, stable urethral lumen that allows unobstructed urine flow, thereby alleviating symptoms like difficulty urinating, weak stream, frequent UTIs, and bladder discomfort. It is considered the gold standard for long-term stricture repair.
Procedures
Urethral Stricture Surgery (Urethroplasty) involves several techniques chosen based on the stricture's characteristics. The patient is given general anesthesia. For excision and primary anastomosis, the scarred segment of the urethra is cut out, and the healthy ends are meticulously stitched together. For longer strictures or those unsuitable for excision, augmentation urethroplasty is performed. This involves opening the strictured area longitudinally and grafting healthy tissue (most commonly buccal mucosa from the inside of the cheek) to widen the urethra. Flap urethroplasty uses local skin or tissue flaps to reconstruct the urethra. A urinary catheter is inserted to stent the repaired urethra during healing, and incisions are closed.
Benefits
Urethral Stricture Surgery (Urethroplasty) offers numerous long-term benefits for patients suffering from urethral strictures:<ul><li><strong>Restored Normal Urination:</strong> Eliminates obstruction, allowing for a strong, uninterrupted urine stream.</li><li><strong>Relief from Symptoms:</strong> Alleviates pain, straining, frequent urination, and incomplete bladder emptying.</li><li><strong>Reduced Infection Risk:</strong> Prevents recurrent urinary tract infections and stone formation often associated with strictures.</li><li><strong>Improved Quality of Life:</strong> Enhances comfort, confidence, and overall well-being by resolving chronic urinary issues.</li><li><strong>High Success Rates:</strong> Offers the highest long-term cure rates compared to other stricture treatments.</li><li><strong>Durable Solution:</strong> Provides a permanent fix, reducing the need for repeated temporary procedures.</li></ul>
Recovery Information
<h3>Urethral Stricture Surgery (Urethroplasty) Recovery Time and Tips</h3><p>Recovery after Urethral Stricture Surgery (Urethroplasty) typically involves a period of rest and careful adherence to post-operative instructions to ensure optimal healing and prevent complications. The initial hospital stay usually lasts 2-5 days. A urinary catheter is kept in place for approximately 2-4 weeks, depending on the complexity of the surgery and the surgeon's preference, to allow the urethra to heal.</p><h4>Key Recovery Aspects:</h4><ul><li><strong>Catheter Care:</strong> Patients will learn how to manage and care for the indwelling catheter at home.</li><li><strong>Activity Restrictions:</strong> Avoid heavy lifting, strenuous exercise, and activities that put pressure on the perineum for 4-6 weeks.</li><li><strong>Pain Management:</strong> Mild pain or discomfort is common and can be managed with prescribed medications.</li><li><strong>Hydration:</strong> Maintaining good hydration is crucial to help flush the bladder and prevent infections.</li><li><strong>Diet:</strong> A normal diet can usually be resumed immediately after surgery.</li><li><strong>Follow-up:</strong> Regular follow-up appointments with the urologist are essential. The catheter is typically removed during one of these visits, followed by further monitoring with flow tests or urethrograms to assess healing.</li><li><strong>Return to Work:</strong> Most patients can return to light desk work within 2-3 weeks, with full recovery taking 6-12 weeks.</li></ul><p>Adhering strictly to your surgeon's advice is paramount for a successful recovery and long-term positive outcome.</p>

PCNL (Percutaneous Nephrolithotomy)
Treatment Price
$3000.00 USDOverview of Percutaneous Nephrolithotomy (PCNL)
- PCNL is a primary treatment for large or complex kidney stones (typically >2 cm) that cannot be effectively managed with less invasive methods like ESWL or Ureteroscopy.
- The procedure aims to achieve complete stone clearance, alleviate pain, prevent kidney damage, and restore normal kidney function.
- It is performed by highly skilled urologists using advanced imaging guidance and specialized endoscopic instruments to ensure precision and patient safety.
- DivinHeal connects you with top-tier hospitals and experienced urologists globally, ensuring access to cutting-edge PCNL techniques.
Overview of Percutaneous Nephrolithotomy (PCNL)
- PCNL is a primary treatment for large or complex kidney stones (typically >2 cm) that cannot be effectively managed with less invasive methods like ESWL or Ureteroscopy.
- The procedure aims to achieve complete stone clearance, alleviate pain, prevent kidney damage, and restore normal kidney function.
- It is performed by highly skilled urologists using advanced imaging guidance and specialized endoscopic instruments to ensure precision and patient safety.
- DivinHeal connects you with top-tier hospitals and experienced urologists globally, ensuring access to cutting-edge PCNL techniques.
Treatment Overview
<h3>Overview of Percutaneous Nephrolithotomy (PCNL)</h3><ul><li>PCNL is a primary treatment for large or complex kidney stones (typically >2 cm) that cannot be effectively managed with less invasive methods like ESWL or Ureteroscopy.</li><li>The procedure aims to achieve complete stone clearance, alleviate pain, prevent kidney damage, and restore normal kidney function.</li><li>It is performed by highly skilled urologists using advanced imaging guidance and specialized endoscopic instruments to ensure precision and patient safety.</li><li>DivinHeal connects you with top-tier hospitals and experienced urologists globally, ensuring access to cutting-edge PCNL techniques.</li></ul>
Procedures
Percutaneous Nephrolithotomy (PCNL) is performed under general anesthesia. The patient is typically positioned face down or on their side. A small incision, usually less than 1 cm, is made in the flank (back). Using X-ray or ultrasound guidance, a needle is inserted through this incision into the kidney's collecting system. A guidewire is then passed through the needle, and the tract is dilated to create a working channel. A nephroscope, a specialized viewing instrument, is inserted through this channel into the kidney. The urologist visualizes the stone, then uses a lithotripter (ultrasonic, pneumatic, or laser probe) to break the stone into smaller pieces. These fragments are then removed using forceps or suction. In some cases, a ureteral stent or a nephrostomy tube (a tube draining urine directly from the kidney to an external bag) may be placed temporarily before closing the incision.
Benefits
<h3>Benefits of Percutaneous Nephrolithotomy (PCNL)</h3><ul><li><strong>High Success Rate:</strong> PCNL offers one of the highest stone-free rates for large and complex kidney stones, often in a single procedure.</li><li><strong>Minimally Invasive:</strong> Compared to traditional open surgery, PCNL involves a much smaller incision, leading to less pain and quicker recovery.</li><li><strong>Effective for Large Stones:</strong> It is the gold standard for stones larger than 2 cm, staghorn calculi, and those resistant to other treatments.</li><li><strong>Reduced Hospital Stay:</strong> Patients typically have a shorter hospital stay compared to open surgical alternatives.</li><li><strong>Improved Quality of Life:</strong> Effective stone removal alleviates pain, reduces the risk of infection, and prevents further kidney damage, significantly improving patient well-being.</li><li><strong>Advanced Technology:</strong> Utilizes advanced endoscopic and lithotripsy techniques for precise stone fragmentation and removal.</li></ul>
Recovery Information
<h3>PCNL Recovery Time and Tips</h3><ul><li><strong>Immediate Post-Procedure:</strong> Patients will typically stay in the hospital for 2-4 days. A nephrostomy tube may be placed temporarily to drain urine and monitor the kidney.</li><li><strong>Pain Management:</strong> Mild to moderate pain is common and managed with medication.</li><li><strong>Activity Restrictions:</strong> Avoid strenuous activities, heavy lifting, and intense exercise for 2-4 weeks. Gradual return to normal activities is encouraged.</li><li><strong>Hydration:</strong> Drink plenty of fluids to help flush out any remaining stone fragments and prevent infection.</li><li><strong>Follow-up:</strong> A follow-up appointment with your urologist is essential to check recovery progress and ensure complete stone clearance, often involving imaging studies.</li><li><strong>Long-term Care:</strong> Dietary modifications and medication may be recommended to prevent future stone formation. DivinHeal provides comprehensive support for your PCNL recovery and long-term wellness.</li></ul>

ESWL (Shock Wave Lithotripsy)
Treatment Price
$1500.00 USDESWL (Shock Wave Lithotripsy) Treatment Overview
Extracorporeal Shock Wave Lithotripsy (ESWL) aims to effectively treat kidney and ureteral stones without surgical incisions. This advanced non-invasive technique uses precisely focused shock waves to fragment stones, minimizing discomfort and facilitating natural passage. DivinHeal connects you with leading urology centers offering state-of-the-art ESWL (Shock Wave Lithotripsy) technology and expert care, prioritizing effective ESWL (Shock Wave Lithotripsy) diagnosis and therapy options.
ESWL (Shock Wave Lithotripsy) Treatment Overview
Extracorporeal Shock Wave Lithotripsy (ESWL) aims to effectively treat kidney and ureteral stones without surgical incisions. This advanced non-invasive technique uses precisely focused shock waves to fragment stones, minimizing discomfort and facilitating natural passage. DivinHeal connects you with leading urology centers offering state-of-the-art ESWL (Shock Wave Lithotripsy) technology and expert care, prioritizing effective ESWL (Shock Wave Lithotripsy) diagnosis and therapy options.
Treatment Overview
<h2>ESWL (Shock Wave Lithotripsy) Treatment Overview</h2><p>Extracorporeal Shock Wave Lithotripsy (ESWL) aims to effectively treat kidney and ureteral stones without surgical incisions. This advanced non-invasive technique uses precisely focused shock waves to fragment stones, minimizing discomfort and facilitating natural passage. DivinHeal connects you with leading urology centers offering state-of-the-art ESWL (Shock Wave Lithotripsy) technology and expert care, prioritizing effective ESWL (Shock Wave Lithotripsy) diagnosis and therapy options.</p>
Procedures
The ESWL (Shock Wave Lithotripsy) procedure begins with the patient lying on a specialized table. Anesthesia (often light sedation or regional block) is administered to ensure comfort. The urologist uses X-ray or ultrasound imaging to precisely locate the kidney or ureteral stone. Once the stone is targeted, a lithotripter machine generates high-energy shock waves. These waves are focused and delivered through a water-filled cushion directly onto the stone. The shock waves repeatedly strike the stone, causing it to fragment into smaller pieces without requiring any incision. The procedure typically lasts 45 to 60 minutes. After the treatment, the patient is monitored for a short period before being discharged, usually the same day.
Benefits
<h2>Benefits of ESWL (Shock Wave Lithotripsy)</h2><ul><li><h3>Non-Invasive Procedure</h3><p>ESWL eliminates the need for surgical incisions, significantly reducing pain, ESWL (Shock Wave Lithotripsy) recovery time, and the risk of complications associated with invasive surgery, enhancing patient safety.</p></li><li><h3>High Success Rate</h3><p>With a high ESWL (Shock Wave Lithotripsy) success rate for appropriately selected stones (often over 85%), many patients achieve complete stone clearance or significant reduction, leading to effective symptom relief and improved quality of life.</p></li><li><h3>Minimal Downtime</h3><p>Patients typically experience a quicker ESWL (Shock Wave Lithotripsy) recovery time, often returning to normal activities within a few days, making it a convenient treatment option for busy individuals.</p></li><li><h3>Reduced Hospital Stay</h3><p>Most ESWL procedures are performed on an outpatient basis, or with a very short hospital stay (typically 1 day), offering greater comfort and convenience and contributing to the procedure's affordability.</p></li><li><h3>Effective Stone Fragmentation</h3><p>The precisely targeted shock waves effectively break down stones into small, passable fragments, alleviating blockages and associated pain, which is crucial for overall patient well-being.</p></li></ul>
Recovery Information
<h2>ESWL (Shock Wave Lithotripsy) Recovery Time and Tips</h2><p>Recovery after ESWL is generally quick and straightforward, allowing most patients to resume light activities within 1-2 days. Full ESWL (Shock Wave Lithotripsy) recovery time may vary depending on the size and number of fragments, typically ranging from a few days to a few weeks as the stone fragments pass.</p><h3>What to Expect During Recovery:</h3><ul><li><strong>Pain Management:</strong> Mild discomfort or colic-like pain is common as stone fragments pass. Pain medication will be prescribed to manage this effectively.</li><li><strong>Blood in Urine:</strong> It's normal to see blood in your urine for a few days post-procedure due to the passage of fragments, which is generally not a cause for concern.</li><li><strong>Hydration:</strong> Drinking plenty of water (2-3 liters per day) is crucial to help flush out the stone fragments and prevent new stone formation, supporting a smooth recovery.</li><li><strong>Straining Urine:</strong> You may be advised to strain your urine to collect fragments for analysis, which helps in preventing future stones.</li><li><strong>Activity:</strong> Avoid strenuous activities for the first few days. Gentle walking is encouraged to aid fragment passage and promote healing.</li></ul><h3>Important Recovery Tips:</h3><ul><li>Adhere strictly to all post-procedure instructions from your urologist for optimal healing.</li><li>Stay well-hydrated to facilitate stone fragment passage.</li><li>Report any fever, severe pain, or difficulty urinating to your doctor immediately, ensuring timely intervention if needed.</li><li>Attend all follow-up appointments to monitor stone clearance and overall progress, confirming the ESWL (Shock Wave Lithotripsy) success rate.</li></ul><p>DivinHeal's dedicated care team provides comprehensive support and guidance throughout your ESWL (Shock Wave Lithotripsy) recovery, ensuring a smooth and safe healing process and addressing any concerns about ESWL (Shock Wave Lithotripsy) recovery time and tips.</p>
Meet Our Doctors
Meet our team of highly qualified and experienced medical professionals dedicated to providing the best healthcare services.

Dr. Abhinandan Mukhopadhyay
Sr. Consultant - Urology & Kidney Transplant Program (Unit I)
Urology, Kidney Transplant, Urological Cancers
Haryana
8+ Years
Experience
Artemis Hospital
Hospital
1500
Fees
Dr. Aditya Gupta
Chairperson - Neurosurgery & CNS Radiosurgery & Co-Chief - Cyberknife Centre
Neurosurgery
New Delhi
32+ Years
Experience
Artemis Hospital
Hospital
1500
Fees

Dr. A. J. Chitkara
Senior Director - Urology, Uro-Oncology, Robotics & Kidney Transplant
Urology
New Delhi
30+ Years
Experience
Apolo Delhi
Hospital
1500
Fees

Dr. Alok Srivastava
Principal Consultant
Urology
New Delhi
32+ Years
Experience
Apolo Delhi
Hospital
1500
Fees

Dr. Amit Kalsotra
Sr. Consultant - Anaesthesia, Critical Care & Pain Management
Anaesthesia, Critical Care, Pain Management
New Delhi
15+ Years
Experience
Artemis Hospital
Hospital
1500
Fees

Dr. Amit K Devra
Senior Director - Urology & Kidney Transplant
Urology, Kidney Transplant
New Delhi
24+ Years
Experience
Apolo Delhi
Hospital
1500
Fees

Dr. Anil Prasad Bhatt
Principal Consultant
Urology, Uro-Oncology, Renal Transplant
New Delhi
30+ Years
Experience
Apolo Delhi
Hospital
1500
Fees

Dr. Anita K. Sharma
Senior Consultant - Obstetrics and Gynaecology
Obstetrics and Gynaecology
New Delhi
24+ Years
Experience
Apolo Delhi
Hospital
1500
Fees

Dr Anshuman Kumar
Principal Director & Unit Head – Surgical Oncology
Surgical Oncology
New Delhi
19+ Years
Experience
Max Hospital,Gurgaon
Hospital
1500
Fees

Dr. Ashutosh Shukla
Senior Consultant
Nephrology
New Delhi
14+ Years
Experience
Apolo Delhi
Hospital
1500
Fees

Dr. Asit Arora
Senior Director, Head of Department - Urology, Uro-Oncology, Robotics and Renal Transplant
Urology, Uro-Oncology, Robotics and Renal Transplant
New Delhi
25+ Years
Experience
Apolo Delhi
Hospital
1500
Fees

Dr. Avtar Singh Bath
Associate Director - Urology and Renal Transplant
Urology
New Delhi
27+ Years
Experience
Apolo Delhi
Hospital
1500
Fees

Dr. Babita Jain
Principal Director & HOD
Paediatrics (Ped)
New Delhi
30+ Years
Experience
Max Hospital,Gurgaon
Hospital
1500
Fees

Dr. Bela Makhija
Principal Director (Obstetrics & Gynaecology) & Head of Unit
Obstetrics & Gynaecology, Gynaecologic Laparoscopy, High-Risk Obstetrics
New Delhi
42+ Years
Experience
Max Hospital,Gurgaon
Hospital
1500
Fees

Dr. Chakraberty
Chief - Emergency
Emergency & Trauma Services
New Delhi
25+ Years
Experience
Artemis Hospital
Hospital
1500
Fees

Dr. Chandeep Singh
Director
Urology
New Delhi
15+ Years
Experience
Apolo Delhi
Hospital
1500
Fees

Dr. Deepak Jha
Chief - Breast Surgery & Sr. Consultant : Surgical Oncology
Breast Surgery, Oncology
New Delhi
15+ Years
Experience
Artemis Hospital
Hospital
1500
Fees

Dr. Ganesh Kumar Mani
Chairman, Cardiac Sciences, Cardiac Surgery (CTVS)
Cardiothoracic and Vascular Surgery (CTVS), Cardiac Sciences
New Delhi
46+ Years
Experience
Max Hospital,Gurgaon
Hospital
1500
Fees

Dr. Gaurav Bansal
Senior Consultant, Urology & Kidney Transplant
Urology
New Delhi
17+ Years
Experience
Apolo Delhi
Hospital
1500
Fees

Dr. Meenal Thakral
Attending Consultant – Geriatric Medicine
Geriatric Medicine, Geriatric Surgery
New Delhi
3+ Years
Experience
Artemis Hospital
Hospital
1500
Fees