Centres Of Excellence
Our Centres of Excellence bring together multidisciplinary teams to deliver precise diagnosis, advanced treatments, and superior outcomes across a wide spectrum of medical specialties.

Related Links
Doctors For Treatment in Similar Locations
Treatments in India for Visitors
Best Hospital Near by for treatment
Related Links
Doctors For Treatment in Similar Locations
Treatments in India for Visitors
- Orthopedics Treatment in Bengaluru for Nigeria
- Orthopedics Treatment in India for Bangladesh
- Orthopedics Treatment in Chennai for Ethiopia
- Orthopedics Treatment in Chennai for Iraq
- Orthopedics Treatment in Mumbai for Iraq
- Orthopedics Treatment in Mumbai for UAE
- Orthopedics Treatment in New Delhi for UAE
- Orthopedics Treatment in Hyderabad for UAE
- Orthopedics Treatment in Gurugram for Nigeria
- Orthopedics Treatment in India for Iraq
- Orthopedics Treatment in New Delhi for Iraq
- Orthopedics Treatment in Pune for Ethiopia
- Orthopedics Treatment in Hyderabad for Iraq
- Orthopedics Treatment in Hyderabad for Bangladesh
- Orthopedics Treatment in Chennai for Nigeria
- Orthopedics Treatment in Gurugram for UAE
- Orthopedics Treatment in Gurugram for Bangladesh
- Orthopedics Treatment in Pune for Bangladesh
- Orthopedics Treatment in Hyderabad for Ethiopia
- Orthopedics Treatment in Gurugram for Ethiopia
- Orthopedics Treatment in Bengaluru for Ethiopia
- Orthopedics Treatment in New Delhi for Ethiopia
- Orthopedics Treatment in Mumbai for Ethiopia
- Orthopedics Treatment in Pune for Nigeria
- Orthopedics Treatment in Hyderabad for Nigeria
- Orthopedics Treatment in New Delhi for Nigeria
- Orthopedics Treatment in Pune for Iraq
- Orthopedics Treatment in Pune for UAE
- Orthopedics Treatment in Bengaluru for UAE
- Orthopedics Treatment in Chennai for UAE
- Orthopedics Treatment in India for UAE
- Orthopedics Treatment in Chennai for Bangladesh
- Orthopedics Treatment in New Delhi for Bangladesh
- Orthopedics Treatment in Mumbai for Bangladesh
- Orthopedics Treatment in Bengaluru for Bangladesh
- Orthopedics Treatment in India for Ethiopia
- Orthopedics Treatment in Gurugram for Iraq
Best Hospital Near by for treatment
Related Links
- Orthopedics cost in New Delhi
- Orthopedics cost in Mumbai
- Orthopedics cost in Haryana
- Orthopedics cost in Hyderabad
- Orthopedics cost in Bengaluru
- Orthopedics cost in Chennai
- Orthopedics Success Rate in Bengaluru
- Orthopedics cost in Pune
- Orthopedics Success Rate in Pune
- Orthopedics Success Rate in New Delhi
- Orthopedics Success Rate in Mumbai
Related Treatments

Trauma / Fracture Fixation (ORIF)
Treatment Price
$3000.00 USDORIF aims to anatomically restore fractured bone segments, providing stability and allowing for early mobilization. This minimizes complications like non-union, malunion, and prolonged immobilization, facilitating a faster return to daily activities. DivinHeal partners with leading orthopedic centers specializing in advanced fracture management.
ORIF aims to anatomically restore fractured bone segments, providing stability and allowing for early mobilization. This minimizes complications like non-union, malunion, and prolonged immobilization, facilitating a faster return to daily activities. DivinHeal partners with leading orthopedic centers specializing in advanced fracture management.
Treatment Overview
ORIF aims to anatomically restore fractured bone segments, providing stability and allowing for early mobilization. This minimizes complications like non-union, malunion, and prolonged immobilization, facilitating a faster return to daily activities. DivinHeal partners with leading orthopedic centers specializing in advanced fracture management.
Procedures
Open Reduction Internal Fixation (ORIF) begins with the patient under general anesthesia. The surgeon makes an incision over the fracture site to expose the broken bone. The bone fragments are then carefully manipulated and realigned (open reduction) to their anatomical position. Once accurately reduced, orthopedic implants such as metal plates, screws, wires, or intramedullary rods are used to hold the fragments securely in place (internal fixation). X-rays or fluoroscopy may be used during the procedure to confirm correct alignment and implant placement. After successful fixation, the wound is thoroughly irrigated, and the incision is closed layer by layer.
Benefits
<h2>Benefits of Trauma / Fracture Fixation (ORIF)</h2><ul><li><h3>Accurate Anatomical Reduction</h3><p>ORIF allows the surgeon to visualize the fracture site directly and precisely realign the bone fragments, restoring the bone's original anatomy. This is crucial for optimal function, especially in fractures involving joints.</p></li><li><h3>Stable Fixation</h3><p>Internal fixation devices provide strong, rigid support to the fractured bone, holding the fragments securely in place during the healing process. This stability minimizes movement at the fracture site, promoting faster and more reliable bone union.</p></li><li><h3>Early Mobilization and Rehabilitation</h3><p>Due to the stable fixation, patients can often begin early movement and weight-bearing (if appropriate for the fracture) sooner than with non-surgical treatments. This early rehabilitation helps prevent joint stiffness, muscle atrophy, and promotes a quicker return to daily activities.</p></li><li><h3>Reduced Risk of Complications</h3><p>By preventing malunion (healing in an incorrect position) or non-union (failure to heal), ORIF reduces the likelihood of long-term pain, deformity, and functional limitations that can arise from improperly healed fractures.</p></li><li><h3>Improved Long-Term Functional Outcomes</h3><p>The precise reduction and stable fixation offered by ORIF significantly enhance the chances of regaining full or near-full function of the affected limb, leading to a better quality of life post-injury.</p></li></ul>
Recovery Information
<h2>Recovery and Rehabilitation After Trauma / Fracture Fixation (ORIF)</h2><p>Recovery from Trauma / Fracture Fixation (ORIF) is a structured process tailored to the specific fracture location, severity, and the individual's overall health. While initial healing often takes several weeks, full functional recovery can extend over several months.</p><h3>Immediate Post-Operative Period (Days 1-7)</h3><ul><li><strong>Hospital Stay:</strong> Typically 3-7 days, focusing on pain management, wound care, and monitoring for complications.</li><li><strong>Immobilization:</strong> The limb may be splinted or casted initially for protection, even with internal fixation.</li><li><strong>Early Mobilization:</strong> Gentle, guided exercises may begin almost immediately for adjacent joints to prevent stiffness, as advised by your surgeon or physical therapist.</li></ul><h3>Intermediate Recovery (Weeks 2-12)</h3><ul><li><strong>Physical Therapy:</strong> A critical component of recovery. A personalized rehabilitation program will focus on regaining range of motion, strength, and reducing swelling.</li><li><strong>Weight-Bearing Restrictions:</strong> Depending on the fracture, partial or non-weight-bearing may be required for several weeks or months.</li><li><strong>Wound Care:</strong> Incision sites will continue to heal, and stitches/staples are typically removed within 2-3 weeks.</li><li><strong>Pain Management:</strong> Gradual reduction of pain medication as healing progresses.</li></ul><h3>Long-Term Rehabilitation (Months 3-12+)</h3><ul><li><strong>Progressive Strengthening:</strong> Exercises to rebuild muscle strength and endurance.</li><li><strong>Functional Training:</strong> Activities to improve balance, coordination, and prepare for daily tasks and recreational activities.</li><li><strong>Return to Activities:</strong> Gradual return to sports or strenuous activities, under the guidance of the surgeon and physical therapist.</li><li><strong>Bone Healing Monitoring:</strong> X-rays will be taken periodically to confirm bone union. In some cases, the implants may be removed after healing, though often they remain permanently.</li></ul><h3>Important Recovery Tips:</h3><ul><li><strong>Follow Instructions:</strong> Adhere strictly to your surgeon's and physical therapist's guidelines regarding weight-bearing, exercises, and activity restrictions.</li><li><strong>Pain Management:</strong> Take prescribed medications as directed and communicate any uncontrolled pain.</li><li><strong>Nutrition:</strong> A healthy diet rich in protein, calcium, and Vitamin D supports bone healing.</li><li><strong>Patience:</strong> Recovery is a marathon, not a sprint. Be patient with your body and celebrate small victories.</li><li><strong>Emotional Support:</strong> Dealing with a fracture and surgery can be challenging. Seek support from family, friends, or counseling if needed.</li></ul><p>DivinHeal ensures you have access to excellent post-operative care and rehabilitation services, supporting your journey back to full health and mobility.</p>

Spinal Fusion (Cervical/Lumbar)
Treatment Price
$8000.00 USDComprehensive Spinal Fusion (Cervical/Lumbar) Treatment
Stabilizing Your Spine, Restoring Your Life
Spinal Fusion (Cervical/Lumbar) is a highly effective surgical intervention aimed at stabilizing sections of the spine that are causing pain, instability, or neurological symptoms. This procedure involves joining two or more vertebrae into a single, solid bone using bone grafts and often internal fixation devices like screws, rods, or plates. The primary goals are to eliminate painful motion, correct deformities, and decompress nerves.
At DivinHeal, we ensure access to world-class neurosurgeons and orthopedic spine specialists who utilize advanced techniques, including minimally invasive approaches, to provide optimal outcomes. We prioritize patient safety, precise diagnosis, and personalized treatment plans for conditions such as degenerative disc disease, spondylolisthesis, spinal stenosis, fractures, and scoliosis.
Comprehensive Spinal Fusion (Cervical/Lumbar) Treatment
Stabilizing Your Spine, Restoring Your Life
Spinal Fusion (Cervical/Lumbar) is a highly effective surgical intervention aimed at stabilizing sections of the spine that are causing pain, instability, or neurological symptoms. This procedure involves joining two or more vertebrae into a single, solid bone using bone grafts and often internal fixation devices like screws, rods, or plates. The primary goals are to eliminate painful motion, correct deformities, and decompress nerves.
At DivinHeal, we ensure access to world-class neurosurgeons and orthopedic spine specialists who utilize advanced techniques, including minimally invasive approaches, to provide optimal outcomes. We prioritize patient safety, precise diagnosis, and personalized treatment plans for conditions such as degenerative disc disease, spondylolisthesis, spinal stenosis, fractures, and scoliosis.
Treatment Overview
<h2>Comprehensive Spinal Fusion (Cervical/Lumbar) Treatment</h2><h3>Stabilizing Your Spine, Restoring Your Life</h3><p>Spinal Fusion (Cervical/Lumbar) is a highly effective surgical intervention aimed at stabilizing sections of the spine that are causing pain, instability, or neurological symptoms. This procedure involves joining two or more vertebrae into a single, solid bone using bone grafts and often internal fixation devices like screws, rods, or plates. The primary goals are to eliminate painful motion, correct deformities, and decompress nerves.</p><p>At DivinHeal, we ensure access to world-class neurosurgeons and orthopedic spine specialists who utilize advanced techniques, including minimally invasive approaches, to provide optimal outcomes. We prioritize patient safety, precise diagnosis, and personalized treatment plans for conditions such as degenerative disc disease, spondylolisthesis, spinal stenosis, fractures, and scoliosis.</p>
Procedures
Spinal Fusion (Cervical/Lumbar) is a complex surgical procedure performed under general anesthesia. The specific steps vary based on the approach (anterior, posterior, or lateral) and the level of the spine (cervical or lumbar). Generally, the procedure involves: 1. Incision: An incision is made in the neck or back, depending on the surgical approach. 2. Decompression: Any structures compressing the nerves, such as herniated discs or bone spurs, are removed (e.g., discectomy or laminectomy). 3. Vertebral Preparation: The surfaces of the vertebrae to be fused are prepared, typically by roughening them to promote bone growth. 4. Bone Graft Placement: A bone graft (autograft, allograft, or synthetic) is placed between the vertebrae in the space created by disc removal or along the side of the vertebrae. 5. Instrumentation: Metal implants like screws, rods, or plates are often used to stabilize the spine internally while the bone graft heals and fuses. 6. Wound Closure: The incision is carefully closed in layers. The goal is for the bone graft to grow and merge the adjacent vertebrae into a single, solid bone over several months.
Benefits
<h2>Benefits of Spinal Fusion (Cervical/Lumbar)</h2><h3>Restoring Stability and Enhancing Quality of Life</h3><ul><li><strong>Significant Pain Relief:</strong> Effectively eliminates pain caused by unstable vertebrae, nerve compression, or degenerative disc disease.</li><li><strong>Spinal Stability:</strong> Provides long-term stability to the affected segment of the spine, preventing further movement and deterioration.</li><li><strong>Correction of Deformities:</strong> Can correct spinal deformities like scoliosis or kyphosis, improving posture and overall spinal alignment.</li><li><strong>Improved Neurological Function:</strong> By decompressing pinched nerves, it can alleviate symptoms like numbness, weakness, or tingling in the limbs.</li><li><strong>Enhanced Mobility & Function:</strong> While motion is restricted at the fused segment, overall functional mobility often improves due to pain reduction.</li><li><strong>Prevention of Further Damage:</strong> Protects the spinal cord and nerves from potential future injury or compression.</li></ul>
Recovery Information
<h2>Spinal Fusion (Cervical/Lumbar) Recovery Time and Tips</h2><h3>A Smooth Path to Healing and Wellness</h3><p>Recovery from Spinal Fusion (Cervical/Lumbar) is a gradual process, typically involving several phases. The initial hospital stay ranges from 3-7 days, where pain management and early mobilization are key. Most patients can expect to return to light activities within 4-6 weeks, but full fusion and complete recovery can take 6 months to a year or even longer.</p><h3>Key Recovery Milestones:</h3><ul><li><strong>First 2-4 Weeks:</strong> Focus on rest, gentle walking, and managing pain. Avoid bending, twisting, and lifting.</li><li><strong>4-12 Weeks:</strong> Gradual increase in activity under guidance. Commencement of physical therapy to strengthen core muscles and improve flexibility.</li><li><strong>3-6 Months:</strong> Continued physical therapy and rehabilitation. Most strenuous activities are still restricted.</li><li><strong>6-12 Months & Beyond:</strong> Gradual return to most normal activities, with ongoing focus on maintaining spinal health through exercise and posture.</li></ul><h3>Recovery Tips:</h3><ul><li><strong>Adhere to Restrictions:</strong> Strictly follow your surgeon’s guidelines regarding lifting, bending, and twisting.</li><li><strong>Physical Therapy:</strong> Engage diligently in your prescribed physical therapy program to regain strength and mobility.</li><li><strong>Pain Management:</strong> Effectively manage pain with prescribed medications and non-pharmacological methods.</li><li><strong>Maintain Good Posture:</strong> Be mindful of your posture to protect your healing spine.</li><li><strong>Nutrition & Hydration:</strong> Support bone healing and overall recovery with a healthy diet and adequate hydration.</li><li><strong>Emotional Support:</strong> Connect with support groups or counseling if needed; recovery can be challenging.</li></ul><p>DivinHeal's care coordinators will provide continuous support and resources throughout your Spinal Fusion (Cervical/Lumbar) recovery, ensuring you have a clear roadmap to regaining your health and independence.</p>

Total Knee Replacement (TKR)
Treatment Price
$6000.00 USDTotal Knee Replacement (TKR) Overview
The primary goal of Total Knee Replacement (TKR) is to alleviate chronic knee pain, often caused by severe osteoarthritis, rheumatoid arthritis, or post-traumatic arthritis, and to restore joint function. During the procedure, the damaged cartilage and bone surfaces of the thigh bone (femur) and shin bone (tibia) are removed and replaced with prosthetic components. The kneecap (patella) may also be resurfaced. Modern TKR techniques focus on precise implant placement, often utilizing advanced imaging and navigation systems, to ensure optimal alignment and long-term durability. DivinHeal connects patients with leading orthopedic surgeons and state-of-the-art facilities specializing in successful TKR outcomes.
Total Knee Replacement (TKR) Overview
The primary goal of Total Knee Replacement (TKR) is to alleviate chronic knee pain, often caused by severe osteoarthritis, rheumatoid arthritis, or post-traumatic arthritis, and to restore joint function. During the procedure, the damaged cartilage and bone surfaces of the thigh bone (femur) and shin bone (tibia) are removed and replaced with prosthetic components. The kneecap (patella) may also be resurfaced. Modern TKR techniques focus on precise implant placement, often utilizing advanced imaging and navigation systems, to ensure optimal alignment and long-term durability. DivinHeal connects patients with leading orthopedic surgeons and state-of-the-art facilities specializing in successful TKR outcomes.
Treatment Overview
<h2>Total Knee Replacement (TKR) Overview</h2><p>The primary goal of Total Knee Replacement (TKR) is to alleviate chronic knee pain, often caused by severe osteoarthritis, rheumatoid arthritis, or post-traumatic arthritis, and to restore joint function. During the procedure, the damaged cartilage and bone surfaces of the thigh bone (femur) and shin bone (tibia) are removed and replaced with prosthetic components. The kneecap (patella) may also be resurfaced. Modern TKR techniques focus on precise implant placement, often utilizing advanced imaging and navigation systems, to ensure optimal alignment and long-term durability. DivinHeal connects patients with leading orthopedic surgeons and state-of-the-art facilities specializing in successful TKR outcomes.</p>
Procedures
Total Knee Replacement (TKR) surgery typically takes 1-2 hours. It is usually performed under general anesthesia or a spinal anesthetic with sedation. The surgeon makes an incision over the front of the knee. The damaged bone and cartilage from the end of the femur (thigh bone) are precisely removed. The end of the tibia (shin bone) is also prepared, removing damaged bone and cartilage. Metal components are then cemented or pressed onto the prepared bone surfaces of the femur and tibia. A high-grade plastic spacer is inserted between the metal components to create a smooth gliding surface. The back of the kneecap (patella) may also be resurfaced with a plastic component. The soft tissues surrounding the knee are then carefully balanced, and the incision is closed with sutures or staples. A drain may be inserted to remove excess fluid, and a sterile dressing is applied.
Benefits
<h2>Benefits of Total Knee Replacement (TKR)</h2><p>Undergoing Total Knee Replacement (TKR) can significantly improve a patient's quality of life. The primary benefits include:</p><ul><li><h3>Significant Pain Relief:</h3><p>TKR is highly effective in eliminating or dramatically reducing chronic knee pain that has not responded to other treatments, allowing patients to resume normal activities.</p></li><li><h3>Improved Mobility and Function:</h3><p>The procedure restores the smooth movement of the knee joint, improving range of motion and making activities like walking, climbing stairs, and standing much easier.</p></li><li><h3>Correction of Deformity:</h3><p>TKR can correct knee deformities, such as bow-legs or knock-knees, which often develop due to severe arthritis, leading to improved leg alignment.</p></li><li><h3>Enhanced Quality of Life:</h3><p>With reduced pain and improved mobility, patients can return to many recreational and social activities, enjoying greater independence and an overall better quality of life.</p></li><li><h3>Long-lasting Results:</h3><p>Modern knee implants are designed to last 15-20 years or even longer for many patients, offering a durable solution to chronic knee problems. The Total Knee Replacement (TKR) success rate is exceptionally high.</p></li></ul><p>DivinHeal connects you with top orthopedic specialists committed to achieving these life-changing outcomes for every patient seeking Total Knee Replacement (TKR) treatment.</p>
Recovery Information
<h2>Total Knee Replacement (TKR) Recovery Time and Tips</h2><p>Recovery from Total Knee Replacement (TKR) is a progressive process that typically involves several phases. While individual recovery times vary, a general timeline can be expected:</p><ul><li><h3>Immediate Post-operative (First Few Days):</h3><p>Patients usually stay in the hospital for 2-4 days. Pain management is crucial, and physical therapy begins almost immediately, often within 24 hours, focusing on gentle range-of-motion exercises and standing/walking with assistance.</p></li><li><h3>Early Recovery (First 3-6 Weeks):</h3><p>Most patients are discharged home with continued physical therapy, either outpatient or home-based. Walking with a cane or crutches is common, gradually transitioning to unassisted walking. The focus is on regaining strength, flexibility, and independence in daily activities.</p></li><li><h3>Mid-term Recovery (3-6 Months):</h3><p>Significant improvements in strength and endurance are seen. Most patients can resume light activities, drive, and return to work (if not physically demanding). Swelling gradually reduces, and the full benefits of the surgery become more apparent.</p></li><li><h3>Long-term Recovery (Up to 12 Months and Beyond):</h3><p>While most pain relief and functional improvement occur within the first 6 months, full strength and maximum recovery can continue for up to a year. Adherence to a home exercise program and lifestyle modifications are key for long-term success and implant longevity.</p></li></ul><h3>Key Recovery Tips:</h3><ul><li><strong>Adhere to Physical Therapy:</strong> This is the most critical component of recovery.</li><li><strong>Pain Management:</strong> Follow your doctor's instructions for pain medication.</li><li><strong>Activity Modification:</strong> Avoid high-impact activities; focus on low-impact exercises like walking, swimming, or cycling.</li><li><strong>Home Modifications:</strong> Ensure a safe environment at home (e.g., grab bars, raised toilet seats).</li><li><strong>Nutrition & Hydration:</strong> Support healing with a healthy diet.</li><li><strong>Follow-up Appointments:</strong> Attend all scheduled check-ups with your surgeon.</li></ul><p>DivinHeal provides comprehensive guidance and connects you with rehabilitation specialists to optimize your Total Knee Replacement (TKR) recovery time and tips, ensuring a smooth and successful return to an active life.</p>
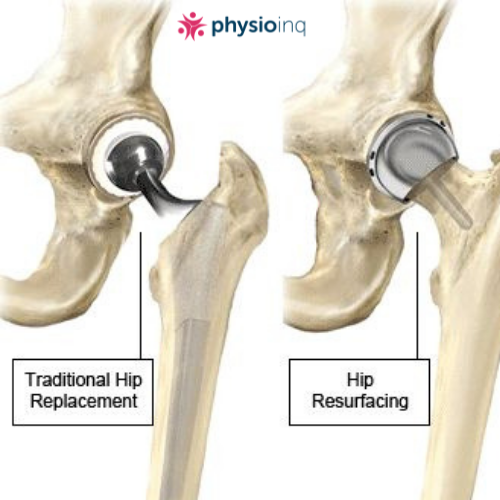
Hip Resurfacing
Treatment Price
$8500.00 USDThe goal of Hip Resurfacing is to relieve severe hip pain, restore joint function, and enable a return to an active lifestyle by meticulously reshaping and capping the hip joint's surfaces. This bone-sparing procedure maintains more of the patient's original anatomy, offering potential benefits for future revision surgeries and allowing a greater range of motion.
The goal of Hip Resurfacing is to relieve severe hip pain, restore joint function, and enable a return to an active lifestyle by meticulously reshaping and capping the hip joint's surfaces. This bone-sparing procedure maintains more of the patient's original anatomy, offering potential benefits for future revision surgeries and allowing a greater range of motion.
Treatment Overview
The goal of Hip Resurfacing is to relieve severe hip pain, restore joint function, and enable a return to an active lifestyle by meticulously reshaping and capping the hip joint's surfaces. This bone-sparing procedure maintains more of the patient's original anatomy, offering potential benefits for future revision surgeries and allowing a greater range of motion.
Procedures
Hip Resurfacing involves making an incision, typically posterior or lateral, to access the hip joint. The femoral head is then dislocated, and the damaged cartilage and a thin layer of bone are precisely reamed and reshaped. A metal or ceramic cap (femoral component) is then cemented or press-fitted onto the reshaped femoral head. Next, the acetabulum (hip socket) is prepared by removing damaged cartilage and reaming it to accept a corresponding metal or ceramic cup (acetabular component), which is then press-fitted or screwed into place. The hip joint is then reduced, and the range of motion and stability are checked before closing the incision.
Benefits
<h2>Benefits of Hip Resurfacing</h2><ul><li><h3>Bone Preservation</h3><p>Unlike total hip replacement, Hip Resurfacing preserves a significant amount of the patient's natural bone, especially in the femoral head and neck. This is advantageous for potential future revision surgeries.</p></li><li><h3>Improved Stability and Range of Motion</h3><p>The larger prosthetic bearing surface of a resurfaced hip mimics the natural joint more closely, potentially offering greater stability, a lower risk of dislocation, and an improved range of motion.</p></li><li><h3>Durability for Active Lifestyles</h3><p>Designed for younger, more active individuals, hip resurfacing allows many patients to return to high-impact activities and sports that might be restricted after a total hip replacement.</p></li><li><h3>Significant Pain Relief</h3><p>Patients experience substantial relief from chronic hip pain caused by arthritis, leading to a dramatic improvement in their quality of life.</p></li><li><h3>Potentially Easier Revision Surgery</h3><p>Should a revision surgery be necessary in the future, the preserved bone stock can make the process less complex than revising a total hip replacement.</p></li></ul>
Recovery Information
<h2>Hip Resurfacing Recovery Time and Tips</h2><ul><li><h3>Immediate Post-Operative Period</h3><p>Patients typically stay in the hospital for 2-4 days following Hip Resurfacing surgery. During this time, pain management is closely monitored, and early mobilization with the aid of crutches or a walker begins.</p></li><li><h3>Early Recovery (2-6 Weeks)</h3><p>Physical therapy starts almost immediately to regain strength, flexibility, and range of motion. Patients will gradually reduce reliance on walking aids. Driving may be resumed after 4-6 weeks, depending on the surgeon's advice and comfort levels.</p></li><li><h3>Mid-Term Recovery (2-3 Months)</h3><p>Intensive physical therapy continues, focusing on strengthening the muscles around the hip. Most patients can return to light daily activities and desk jobs. Swelling and discomfort will progressively diminish.</p></li><li><h3>Full Recovery (3-6 Months and Beyond)</h3><p>Full recovery, including a return to more strenuous activities and sports, can take 3 to 6 months or even longer, depending on individual healing and dedication to rehabilitation. Long-term follow-up and adherence to recommended exercises are crucial for optimal and lasting results. DivinHeal ensures access to comprehensive rehabilitation programs to support your journey back to full activity.</p></li></ul>

Total Hip Replacement (THR)
Treatment Price
$6500.00 USDTotal Hip Replacement treatment involves carefully replacing the worn or damaged parts of the hip joint with artificial implants. The primary goals are pain relief, restoration of hip function, and improved weight-bearing capacity. DivinHeal connects patients with world-class orthopedic surgeons and accredited hospitals, ensuring access to advanced surgical techniques and rehabilitation programs for optimal outcomes.
Total Hip Replacement treatment involves carefully replacing the worn or damaged parts of the hip joint with artificial implants. The primary goals are pain relief, restoration of hip function, and improved weight-bearing capacity. DivinHeal connects patients with world-class orthopedic surgeons and accredited hospitals, ensuring access to advanced surgical techniques and rehabilitation programs for optimal outcomes.
Treatment Overview
Total Hip Replacement treatment involves carefully replacing the worn or damaged parts of the hip joint with artificial implants. The primary goals are pain relief, restoration of hip function, and improved weight-bearing capacity. DivinHeal connects patients with world-class orthopedic surgeons and accredited hospitals, ensuring access to advanced surgical techniques and rehabilitation programs for optimal outcomes.
Procedures
Total Hip Replacement involves making an incision, usually on the side or back of the hip. The surgeon removes the damaged femoral head and reshapes the hip socket. The artificial socket is then implanted into the pelvis. Next, a metal stem is inserted into the top of the thigh bone, and an artificial ball is attached to the stem. The new ball-and-socket components are then joined, forming the new hip joint. The incision is closed with sutures or staples.
Benefits
<h2>Benefits of Total Hip Replacement</h2><ul><li><h3>Significant Pain Relief</h3><p>One of the most profound benefits, alleviating chronic hip pain that often limits daily activities.</p></li><li><h3>Improved Mobility and Range of Motion</h3><p>Restores the ability to walk, bend, and move with greater ease and less stiffness.</p></li><li><h3>Enhanced Quality of Life</h3><p>Allows patients to resume hobbies, social activities, and everyday tasks, leading to greater independence.</p></li><li><h3>Correction of Deformity</h3><p>Can correct leg length discrepancies and improve overall posture and gait.</p></li><li><h3>Long-lasting Results</h3><p>Modern hip implants are designed to last 15-20 years or more, providing durable relief.</p></li><li><h3>Increased Activity Levels</h3><p>Enables participation in light sports and exercise, contributing to overall health and well-being.</p></li></ul>
Recovery Information
<h2>Total Hip Replacement Recovery Time and Tips</h2><p>Recovery from Total Hip Replacement is a gradual process, but most patients experience significant improvement within weeks and full recovery within 3-6 months. The immediate hospital stay is typically 5-7 days, focusing on pain management, wound care, and initiating physical therapy.</p><h3>Key Recovery Milestones:</h3><ul><li><strong>First Few Weeks:</strong> Walking with assistance (walker, crutches), managing pain, and performing prescribed exercises.</li><li><strong>1-3 Months:</strong> Gradual reduction in pain and swelling, improved strength and mobility, often progressing to a cane or walking unassisted. Resumption of light daily activities.</li><li><strong>3-6 Months:</strong> Significant return to normal activities, including driving and some recreational pursuits, with continued adherence to physical therapy.</li></ul><h3>Important Recovery Tips:</h3><ul><li><strong>Adhere to Physical Therapy:</strong> Crucial for regaining strength, flexibility, and proper gait.</li><li><strong>Pain Management:</strong> Follow your doctor's instructions for medication to keep pain at bay.</li><li><strong>Incision Care:</strong> Keep the incision clean and dry to prevent infection.</li><li><strong>Avoid Certain Movements:</strong> Follow specific hip precautions (e.g., avoiding extreme flexion, internal rotation) to prevent dislocation, especially in the early weeks.</li><li><strong>Healthy Lifestyle:</strong> Maintain a balanced diet, stay hydrated, and avoid smoking to promote healing.</li><li><strong>Patience and Positive Outlook:</strong> Recovery takes time; celebrate small victories and stay committed to your rehabilitation plan.</li></ul><p>DivinHeal provides comprehensive support, connecting you with rehabilitation specialists and offering guidance throughout your recovery journey.</p>

Sports Injury Surgery (ACL/PCL/MCL Multi-ligament)
Treatment Price
$7500.00 USDSports Injury Surgery for multi-ligament knee tears focuses on restoring the structural integrity and stability of the knee joint. This typically involves reconstructing the torn ligaments using autografts (tissue from the patient's own body) or allografts (donor tissue). The goal is to alleviate pain, prevent long-term instability and arthritis, and facilitate a safe return to activities, often through minimally invasive arthroscopic techniques.
Sports Injury Surgery for multi-ligament knee tears focuses on restoring the structural integrity and stability of the knee joint. This typically involves reconstructing the torn ligaments using autografts (tissue from the patient's own body) or allografts (donor tissue). The goal is to alleviate pain, prevent long-term instability and arthritis, and facilitate a safe return to activities, often through minimally invasive arthroscopic techniques.
Treatment Overview
Sports Injury Surgery for multi-ligament knee tears focuses on restoring the structural integrity and stability of the knee joint. This typically involves reconstructing the torn ligaments using autografts (tissue from the patient's own body) or allografts (donor tissue). The goal is to alleviate pain, prevent long-term instability and arthritis, and facilitate a safe return to activities, often through minimally invasive arthroscopic techniques.
Procedures
Sports Injury Surgery for multi-ligament knee reconstruction is typically performed under general anesthesia. The surgeon makes several small incisions around the knee (arthroscopy) to insert a camera and specialized instruments. The damaged ligaments (ACL, PCL, MCL, LCL) are identified and cleared. Graft tissue, either autograft (from the patient's hamstring, patellar tendon, or quadriceps tendon) or allograft (donor tissue), is prepared. Tunnels are precisely drilled into the tibia and femur bones, through which the new graft ligaments are threaded. The grafts are then secured using screws, staples, or other fixation devices, ensuring appropriate tension. Any associated injuries, such as meniscal tears or cartilage damage, are also addressed during the same procedure. After securing the grafts, the incisions are closed, and a sterile dressing is applied.
Benefits
<h2>Benefits of Sports Injury Surgery (ACL/PCL/MCL Multi-ligament)</h2><ul><li><h3>Restored Knee Stability</h3><p>Surgical reconstruction significantly improves the stability of the knee joint, preventing abnormal movement and reducing the risk of further injury.</p></li><li><h3>Reduced Pain and Swelling</h3><p>Effective treatment alleviates chronic pain and inflammation associated with ligament tears, leading to improved comfort.</p></li><li><h3>Improved Mobility and Function</h3><p>Patients regain a full range of motion and functional capabilities, allowing them to participate in daily activities and sports.</p></li><li><h3>Prevention of Long-term Complications</h3><p>Stabilizing the knee reduces the likelihood of developing secondary issues like meniscal tears, cartilage damage, and early-onset osteoarthritis.</p></li><li><h3>Return to Sports and Active Lifestyle</h3><p>For athletes, successful surgery and dedicated rehabilitation offer the best chance to safely return to their pre-injury level of activity and competitive sports.</p></li><li><h3>Enhanced Quality of Life</h3><p>By restoring knee health, the procedure dramatically improves overall quality of life, independence, and psychological well-being.</p></li></ul>
Recovery Information
<h2>Recovery and Rehabilitation After Sports Injury Surgery (ACL/PCL/MCL Multi-ligament)</h2><p>Recovery from multi-ligament knee surgery is a gradual process requiring dedication to a structured rehabilitation program. The initial hospital stay typically lasts 3-7 days, focusing on pain management, wound care, and early mobilization exercises. Post-discharge, the recovery journey generally involves several phases:</p><ul><li><h3>Phase 1: Early Post-operative (Weeks 1-6)</h3><p>Focus on reducing swelling, protecting the surgical repair, gradually restoring knee extension, and gentle weight-bearing as tolerated. Crutches are usually required, and a brace may be used for support.</p></li><li><h3>Phase 2: Intermediate (Weeks 7-16)</h3><p>Progressive strengthening exercises for the quadriceps and hamstrings, improving balance, and increasing range of motion. Stationary cycling and swimming may be introduced.</p></li><li><h3>Phase 3: Advanced Strengthening & Agility (Months 4-9)</h3><p>Introduction of sport-specific drills, agility training, plyometrics, and higher-level strengthening to prepare the knee for dynamic activities.</p></li><li><h3>Phase 4: Return to Sport (Months 9-12+)</h3><p>A gradual, supervised return to full sports activities, only after meeting specific strength, stability, and functional criteria. Full return to competitive sports can take 12-18 months, varying by individual and sport.</p></li></ul><p>Adherence to physical therapy protocols is crucial for optimal outcomes. DivinHeal assists with connecting you to rehabilitation specialists and providing resources for continued recovery support.</p>

Spine Decompression (Discectomy / Laminectomy)
Treatment Price
$3000.00 USDOverview of Spine Decompression Surgery
Spine Decompression surgeries, primarily Discectomy and Laminectomy, aim to alleviate symptoms caused by compressed nerves in the spine. A Discectomy involves removing part of a herniated disc that is pressing on a nerve, while a Laminectomy removes a portion of the vertebral bone (lamina) to create more space within the spinal canal. These procedures are critical for restoring function, reducing pain, and improving quality of life for patients suffering from debilitating spinal conditions.
Overview of Spine Decompression Surgery
Spine Decompression surgeries, primarily Discectomy and Laminectomy, aim to alleviate symptoms caused by compressed nerves in the spine. A Discectomy involves removing part of a herniated disc that is pressing on a nerve, while a Laminectomy removes a portion of the vertebral bone (lamina) to create more space within the spinal canal. These procedures are critical for restoring function, reducing pain, and improving quality of life for patients suffering from debilitating spinal conditions.
Treatment Overview
<h3>Overview of Spine Decompression Surgery</h3><p>Spine Decompression surgeries, primarily Discectomy and Laminectomy, aim to alleviate symptoms caused by compressed nerves in the spine. A Discectomy involves removing part of a herniated disc that is pressing on a nerve, while a Laminectomy removes a portion of the vertebral bone (lamina) to create more space within the spinal canal. These procedures are critical for restoring function, reducing pain, and improving quality of life for patients suffering from debilitating spinal conditions.</p>
Procedures
Spine Decompression procedures are performed under general anesthesia. For a Discectomy, a small incision is made in the back or neck, and specialized instruments are used to access the spine. The surgeon then carefully removes the herniated portion of the disc that is impinging on the nerve root. Often, this can be done using minimally invasive techniques, such as microdiscectomy, involving a smaller incision and less muscle disruption. For a Laminectomy, a larger incision may be necessary to expose the vertebrae. The surgeon removes part or all of the lamina (the bony arch of the vertebra) and any bone spurs or ligaments that are causing compression of the spinal cord or nerve roots. In some cases, spinal fusion may be performed concurrently to stabilize the spine if significant bone removal is required or instability is present.
Benefits
<h3>Benefits of Spine Decompression (Discectomy / Laminectomy)</h3><ul><li><h4>Significant Pain Relief</h4><p>Effectively alleviates chronic back or neck pain, sciatica, and radiating limb pain caused by nerve compression.</p></li><li><h4>Improved Mobility and Function</h4><p>Restores range of motion and enables patients to resume daily activities and physical pursuits.</p></li><li><h4>Prevention of Further Nerve Damage</h4><p>Relieves pressure on the spinal cord and nerves, preventing potential long-term neurological deficits.</p></li><li><h4>Enhanced Quality of Life</h4><p>Frees patients from debilitating pain, allowing them to enjoy a more active and fulfilling life.</p></li><li><h4>High <a href="#section-success-rate">Spine Decompression (Discectomy / Laminectomy) success rate</a></h4><p>These procedures have a high rate of success in resolving symptoms when performed on carefully selected patients.</p></li></ul>
Recovery Information
<h3>Spine Decompression (Discectomy / Laminectomy) Recovery Time and Tips</h3><p>Recovery after Spine Decompression surgery is a crucial period, typically spanning several weeks to months, depending on the individual and the extent of the procedure. Immediately after surgery, patients usually stay in the hospital for 1-3 days. Pain management, guided walking, and gentle movements are initiated early.</p><h4>Key Recovery Aspects:</h4><ul><li><p><strong>Initial Phase (1-2 weeks):</strong> Focus on rest, limited activity, and pain control. Avoid bending, lifting, or twisting.</p></li><li><p><strong>Physical Therapy (2-6 weeks onwards):</strong> A supervised Spine Decompression (Discectomy / Laminectomy) rehabilitation exercises program is vital. This includes strengthening core muscles, improving flexibility, and posture correction.</p></li><li><p><strong>Return to Activities:</strong> Light office work may resume within 2-4 weeks. Strenuous activities and heavy lifting are typically restricted for 3-6 months. Driving can often be resumed after 2-4 weeks, once off strong pain medication and mobility is adequate.</p></li><li><p><strong>Long-term Wellness:</strong> Maintaining a healthy weight, regular exercise, and proper body mechanics are essential for long-term spinal health. DivinHeal's care coordinators provide ongoing support and resources throughout your recovery journey.</p></li></ul>

Shoulder Replacement
Treatment Price
$6500.00 USDOverview of Shoulder Replacement Treatment
Shoulder Replacement surgery aims to restore function and alleviate chronic pain in the shoulder joint. This procedure involves replacing the bone ends and cartilage with smooth, artificial surfaces (prostheses). Depending on the damage, a total shoulder replacement, hemiarthroplasty (half replacement), or a reverse total shoulder replacement may be performed. DivinHeal facilitates access to world-class orthopedic surgeons and state-of-the-art facilities, ensuring a tailored approach for optimal outcomes.
Overview of Shoulder Replacement Treatment
Shoulder Replacement surgery aims to restore function and alleviate chronic pain in the shoulder joint. This procedure involves replacing the bone ends and cartilage with smooth, artificial surfaces (prostheses). Depending on the damage, a total shoulder replacement, hemiarthroplasty (half replacement), or a reverse total shoulder replacement may be performed. DivinHeal facilitates access to world-class orthopedic surgeons and state-of-the-art facilities, ensuring a tailored approach for optimal outcomes.
Treatment Overview
<h2>Overview of Shoulder Replacement Treatment</h2><p>Shoulder Replacement surgery aims to restore function and alleviate chronic pain in the shoulder joint. This procedure involves replacing the bone ends and cartilage with smooth, artificial surfaces (prostheses). Depending on the damage, a total shoulder replacement, hemiarthroplasty (half replacement), or a reverse total shoulder replacement may be performed. DivinHeal facilitates access to world-class orthopedic surgeons and state-of-the-art facilities, ensuring a tailored approach for optimal outcomes.</p>
Procedures
Shoulder Replacement surgery typically involves an incision around the shoulder. The surgeon carefully accesses the shoulder joint, removes the damaged bone and cartilage from the humerus head and/or glenoid socket. For a total shoulder replacement, a metal ball is implanted onto the humerus, and a plastic socket is fitted into the glenoid. In a reverse total shoulder replacement, the ball is fixed to the shoulder blade and the socket to the humerus. Hemiarthroplasty replaces only the humerus head. The components are typically cemented or press-fit into place. After implanting the prostheses, the surgeon tests the new joint's range of motion and stability, then closes the incision.
Benefits
<h2>Benefits of Shoulder Replacement Treatment</h2><ul><li><h3>Significant Pain Relief</h3><p>One of the primary benefits is the dramatic reduction or elimination of chronic shoulder pain that interfered with daily activities and sleep.</p></li><li><h3>Improved Range of Motion</h3><p>Patients typically experience enhanced flexibility and a greater ability to move their arm, making everyday tasks easier.</p></li><li><h3>Restored Shoulder Function</h3><p>The surgery helps restore stability and strength to the shoulder, allowing for better arm use in various activities.</p></li><li><h3>Enhanced Quality of Life</h3><p>With less pain and improved function, patients can enjoy a more active and independent lifestyle, participating in hobbies and activities they once loved.</p></li><li><h3>Long-term Solution</h3><p>Modern shoulder implants are designed to last for many years, offering a durable solution for joint degeneration.</p></li><li><h3>High Success Rate</h3><p>Shoulder Replacement success rate is consistently high, with most patients reporting excellent long-term outcomes.</p></li></ul>
Recovery Information
<h2>Shoulder Replacement Recovery Time and Tips</h2><p>Recovery after Shoulder Replacement treatment typically involves several phases, ranging from immediate post-operative care to long-term rehabilitation.</p><ul><li><h3>Hospital Stay (3-5 Days)</h3><p>Immediately after surgery, you'll stay in the hospital for a few days for pain management and initial mobility exercises. A sling will be used to protect the shoulder.</p></li><li><h3>Early Recovery (0-6 Weeks)</h3><p>During this period, focus is on pain control, wound care, and gentle physical therapy exercises. It's crucial to avoid certain arm movements as directed by your surgeon and physical therapist. Driving is usually not allowed during this phase.</p></li><li><h3>Intermediate Recovery (6-12 Weeks)</h3><p>As pain subsides, physical therapy intensifies to regain strength and a greater range of motion. You'll gradually reduce sling use. Light daily activities may resume.</p></li><li><h3>Advanced Recovery (3-6 Months)</h3><p>This phase involves more rigorous strengthening and functional exercises to improve endurance and return to more demanding activities. Full Shoulder Replacement recovery time can extend up to a year, depending on individual factors and adherence to rehabilitation protocols. Adhering to Shoulder Replacement physiotherapy and recovery exercises is vital for the best outcome.</p></li></ul><p>DivinHeal provides comprehensive support throughout your recovery, including access to expert physical therapists and guidance on lifestyle modifications for optimal long-term results.</p>

Scoliosis Correction Surgery
Treatment Price
$8000.00 USDOverview of Scoliosis Correction Surgery Goals
The primary goal of Scoliosis Correction Surgery is to halt the progression of the spinal curve, correct the existing deformity, and stabilize the spine. This often involves spinal fusion, where vertebrae are fused together with the aid of rods, screws, and bone grafts to create a single, solid bone segment. Newer techniques like Vertebral Body Tethering (VBT) offer growth modulation options for younger patients. DivinHeal connects you with top-tier orthopedic and spine surgeons specializing in advanced scoliosis treatment.
Overview of Scoliosis Correction Surgery Goals
The primary goal of Scoliosis Correction Surgery is to halt the progression of the spinal curve, correct the existing deformity, and stabilize the spine. This often involves spinal fusion, where vertebrae are fused together with the aid of rods, screws, and bone grafts to create a single, solid bone segment. Newer techniques like Vertebral Body Tethering (VBT) offer growth modulation options for younger patients. DivinHeal connects you with top-tier orthopedic and spine surgeons specializing in advanced scoliosis treatment.
Treatment Overview
<h3>Overview of Scoliosis Correction Surgery Goals</h3><p>The primary goal of Scoliosis Correction Surgery is to halt the progression of the spinal curve, correct the existing deformity, and stabilize the spine. This often involves spinal fusion, where vertebrae are fused together with the aid of rods, screws, and bone grafts to create a single, solid bone segment. Newer techniques like Vertebral Body Tethering (VBT) offer growth modulation options for younger patients. DivinHeal connects you with top-tier orthopedic and spine surgeons specializing in advanced scoliosis treatment.</p>
Procedures
Scoliosis Correction Surgery, commonly Posterior Spinal Fusion, involves an incision along the back to expose the spine. Screws, hooks, or wires are precisely placed into the vertebrae. Rods, made of titanium or stainless steel, are then attached to these anchors. The surgeon carefully manipulates the rods to gently straighten and derotate the spine, correcting the curve. Bone graft material (either from the patient or a donor, or synthetic) is placed around the fusion site to promote bone growth between the vertebrae. This process leads to a solid fusion over several months. Advanced techniques include intraoperative neurological monitoring to protect spinal cord function during the procedure.
Benefits
<h3>Benefits of Scoliosis Correction Surgery</h3><ul><li>Significant correction of spinal curvature, improving posture and appearance.</li><li>Prevention of further curve progression.</li><li>Alleviation of chronic back pain and nerve compression symptoms.</li><li>Improved lung function in cases where severe curves compress the lungs.</li><li>Enhanced quality of life and self-esteem.</li><li>Long-term spinal stability.</li></ul>
Recovery Information
<h3>Scoliosis Correction Surgery Recovery Time and Tips</h3><p>Recovery from Scoliosis Correction Surgery typically involves a hospital stay of 5-7 days. Most patients can return to light activities and school within 3-4 weeks. Full recovery and return to strenuous activities, including sports, usually takes 6-12 months as the spinal fusion solidifies. Key recovery tips include:</p><ul><li>Adhering strictly to post-operative instructions, including medication schedules.</li><li>Engaging in prescribed physical therapy to regain strength and flexibility.</li><li>Avoiding heavy lifting, twisting, or bending for several months.</li><li>Maintaining good posture.</li><li>Regular follow-up appointments with your spine surgeon.</li><li>Ensuring adequate rest and nutrition for healing.</li></ul>

Rotator Cuff Repair (Arthroscopy)
Treatment Price
$4500.00 USDThe primary goal of Rotator Cuff Repair (Arthroscopy) is to alleviate chronic shoulder pain, improve range of motion, and restore strength by meticulously reattaching the torn rotator cuff tendons to the humerus bone. This advanced procedure employs arthroscopic techniques, involving several small incisions, a miniature camera for visualization, and specialized instruments, which typically results in less post-operative pain, reduced scarring, and a faster recovery compared to traditional open surgery.
The primary goal of Rotator Cuff Repair (Arthroscopy) is to alleviate chronic shoulder pain, improve range of motion, and restore strength by meticulously reattaching the torn rotator cuff tendons to the humerus bone. This advanced procedure employs arthroscopic techniques, involving several small incisions, a miniature camera for visualization, and specialized instruments, which typically results in less post-operative pain, reduced scarring, and a faster recovery compared to traditional open surgery.
Treatment Overview
The primary goal of Rotator Cuff Repair (Arthroscopy) is to alleviate chronic shoulder pain, improve range of motion, and restore strength by meticulously reattaching the torn rotator cuff tendons to the humerus bone. This advanced procedure employs arthroscopic techniques, involving several small incisions, a miniature camera for visualization, and specialized instruments, which typically results in less post-operative pain, reduced scarring, and a faster recovery compared to traditional open surgery.
Procedures
1. **Anesthesia**: The patient receives general anesthesia to ensure complete comfort throughout the procedure. A regional nerve block may also be administered to provide extended pain relief post-surgery. 2. **Incision Placement**: Several small incisions, typically less than 1 cm each, are made around the shoulder joint. These are known as portal sites. 3. **Arthroscope Insertion**: A thin tube containing a camera (arthroscope) is inserted through one of the incisions. This camera projects magnified, live images of the inside of the joint onto a monitor, guiding the surgeon. 4. **Joint Examination**: The surgeon thoroughly inspects the entire shoulder joint, including the rotator cuff tendons, biceps tendon, labrum, and cartilage, to assess the extent of the damage and identify any associated injuries. 5. **Preparation of the Tendon and Bone**: Any inflamed or damaged tissue (e.g., frayed tendon edges, bone spurs) is carefully removed. The bone where the tendon was torn is gently prepared (roughened) to create a fresh surface, which promotes better healing of the tendon to the bone. 6. **Tendon Reattachment**: Specialized miniature instruments are inserted through the other small incisions. Small, bioabsorbable anchors (which dissolve over time) are inserted into the bone. Sutures attached to these anchors are then passed through the torn tendon, and the tendon is securely reattached to its anatomical position on the humerus. 7. **Closure**: Once the repair is complete and stability is confirmed, the instruments and arthroscope are removed. The small incisions are closed with a stitch or sterile strips, and a sterile dressing is applied. The arm is then typically placed in a sling to protect the repair.
Benefits
<h2>Benefits of Rotator Cuff Repair (Arthroscopy)</h2><ul><li><h3>Minimally Invasive</h3><p>Requires only small incisions, leading to less tissue damage, reduced pain, and minimal scarring compared to open surgery.</p></li><li><h3>Faster Recovery Time</h3><p>Patients typically experience a quicker initial recovery and return to light activities due to the less invasive nature of the procedure.</p></li><li><h3>Reduced Complications</h3><p>Lower risk of infection and blood loss compared to traditional open surgical methods.</p></li><li><h3>Enhanced Visualization</h3><p>The arthroscope provides a magnified, high-definition view of the entire shoulder joint, allowing for a precise and thorough repair.</p></li><li><h3>Effective Pain Relief</h3><p>Significantly alleviates chronic shoulder pain caused by the torn rotator cuff.</p></li><li><h3>Restoration of Function</h3><p>Improves shoulder strength, stability, and range of motion, enabling a return to daily activities and sports.</p></li><li><h3>High Success Rate</h3><p>A proven track record of successful outcomes in restoring shoulder integrity and improving quality of life.</p></li></ul>
Recovery Information
<h2>Recovery and Life After Rotator Cuff Repair (Arthroscopy)</h2><p>Recovery from Rotator Cuff Repair (Arthroscopy) is a progressive process that demands patience and strict adherence to your surgeon's and physical therapist's guidelines. Immediately after surgery, your arm will be immobilized in a sling for approximately 4-6 weeks to protect the healing tendon and allow for initial tissue regeneration. During this phase, passive range-of-motion exercises may begin.</p><p>Physical therapy is a cornerstone of successful recovery, typically commencing shortly after surgery. Initially, therapy focuses on gentle passive and then active-assisted range of motion. Over the subsequent 3-6 months, exercises will gradually progress to active motion, strengthening of the rotator cuff and surrounding muscles, and regaining functional use of the arm. It's crucial to avoid heavy lifting, pushing, or pulling during this period.</p><p>Most patients can resume light daily activities within a few weeks, but a full return to strenuous activities, sports, or demanding overhead work can take anywhere from 6 to 12 months, depending on the size of the tear, individual healing capacity, and consistency with rehabilitation. Pain management, including prescribed medications and ice therapy, will be important during the initial recovery phase. DivinHeal ensures you receive a personalized rehabilitation plan and continuous support to optimize your healing journey and help you regain a pain-free, active lifestyle.</p>

Revision Knee Replacement
Treatment Price
$6500.00 USDOverview of Revision Knee Replacement
Revision Knee Replacement treatment is a sophisticated orthopedic procedure designed to address problems arising from a previously implanted knee prosthesis. The primary goals are:
- Alleviating chronic pain and discomfort.
- Restoring stability and improving the range of motion in the knee.
- Correcting issues such as implant loosening, infection, instability, or severe wear.
- Enhancing the patient's overall quality of life and functional independence.
Key Techniques Involved:
- Implant Removal: Carefully extracting the failed or worn-out components.
- Bone Preparation: Addressing any bone loss with grafts or specialized implants.
- New Implant Insertion: Utilizing specialized revision components, which are often larger and have longer stems for enhanced stability.
- Soft Tissue Balancing: Ensuring proper ligament tension for optimal knee function.
DivinHeal connects you with highly experienced orthopedic surgeons specializing in Revision Knee Replacement, ensuring access to advanced techniques and personalized care for the best possible outcome.
Overview of Revision Knee Replacement
Revision Knee Replacement treatment is a sophisticated orthopedic procedure designed to address problems arising from a previously implanted knee prosthesis. The primary goals are:
- Alleviating chronic pain and discomfort.
- Restoring stability and improving the range of motion in the knee.
- Correcting issues such as implant loosening, infection, instability, or severe wear.
- Enhancing the patient's overall quality of life and functional independence.
Key Techniques Involved:
- Implant Removal: Carefully extracting the failed or worn-out components.
- Bone Preparation: Addressing any bone loss with grafts or specialized implants.
- New Implant Insertion: Utilizing specialized revision components, which are often larger and have longer stems for enhanced stability.
- Soft Tissue Balancing: Ensuring proper ligament tension for optimal knee function.
DivinHeal connects you with highly experienced orthopedic surgeons specializing in Revision Knee Replacement, ensuring access to advanced techniques and personalized care for the best possible outcome.
Treatment Overview
<h2>Overview of Revision Knee Replacement</h2><p><code>Revision Knee Replacement treatment</code> is a sophisticated orthopedic procedure designed to address problems arising from a previously implanted knee prosthesis. The primary goals are:</p><ul><li>Alleviating chronic pain and discomfort.</li><li>Restoring stability and improving the range of motion in the knee.</li><li>Correcting issues such as implant loosening, infection, instability, or severe wear.</li><li>Enhancing the patient's overall quality of life and functional independence.</li></ul><h3>Key Techniques Involved:</h3><ul><li><strong>Implant Removal:</strong> Carefully extracting the failed or worn-out components.</li><li><strong>Bone Preparation:</strong> Addressing any bone loss with grafts or specialized implants.</li><li><strong>New Implant Insertion:</strong> Utilizing specialized revision components, which are often larger and have longer stems for enhanced stability.</li><li><strong>Soft Tissue Balancing:</strong> Ensuring proper ligament tension for optimal knee function.</li></ul><p>DivinHeal connects you with highly experienced orthopedic surgeons specializing in <code>Revision Knee Replacement</code>, ensuring access to advanced techniques and personalized care for the best possible outcome.</p>
Procedures
Revision Knee Replacement is a complex surgical procedure performed under general or spinal anesthesia. The surgeon typically begins by making an incision, often reusing the scar from the initial surgery. The procedure involves: 1. Careful exposure of the knee joint, which may require releasing scar tissue. 2. Identification and systematic removal of the failed or worn-out components of the primary knee replacement. This step requires precision as components can be firmly fixed with cement or bone ingrowth. 3. Assessment of bone quality and quantity. Any bone loss is addressed using bone grafts (either from the patient, a donor, or synthetic material) or specialized metal augments to rebuild the foundational bone. 4. Preparation of the remaining bone for the new revision implants. This often involves reaming and shaping the femoral and tibial canals to accommodate the longer stems characteristic of revision components. 5. Insertion of the new revision prosthetic components, which are often modular, allowing the surgeon to customize the fit and alignment to the patient's specific anatomy and bone defects. These implants typically have longer stems for enhanced stability and fixation. 6. Soft tissue balancing to ensure optimal ligament tension and knee stability throughout the range of motion. 7. Trial reduction to verify proper component placement, stability, and range of motion before final implantation. 8. Secure fixation of the new implants, usually with bone cement. 9. Closure of the surgical incision in layers, and typically, a drain is placed to prevent fluid accumulation. The complexity of the procedure can vary significantly based on the reason for revision and the extent of bone loss or soft tissue damage.
Benefits
<h2>Benefits of Revision Knee Replacement</h2><p>Undergoing <code>Revision Knee Replacement treatment</code> can bring significant improvements to a patient's life, especially when the initial knee replacement has failed. The primary advantages include:</p><ul><li><strong>Significant Pain Relief:</strong> Alleviating the chronic pain and discomfort caused by a failing or problematic knee implant, allowing for a better quality of life.</li><li><strong>Improved Knee Function and Mobility:</strong> Restoring the knee's ability to bend, straighten, and bear weight effectively, which enhances walking, standing, and performing daily activities.</li><li><strong>Enhanced Stability:</strong> Addressing issues of knee instability, preventing the knee from giving way and reducing the risk of falls.</li><li><strong>Correction of Deformity:</strong> Rectifying any existing deformities or malalignment that may have developed due to the failed primary implant.</li><li><strong>Extended Lifespan of the Joint:</strong> Providing a durable solution that can last for many years, delaying or potentially eliminating the need for further surgery.</li><li><strong>Improved Quality of Life:</strong> Empowering patients to return to activities they enjoy, regain independence, and improve their overall well-being.</li></ul><p>DivinHeal partners with surgeons who utilize <code>advanced techniques for Revision Knee Replacement</code> to maximize these benefits for every patient.</p>
Recovery Information
<h2>Revision Knee Replacement Recovery Time and Tips</h2><p>The <code>Revision Knee Replacement recovery time and tips</code> are crucial for achieving optimal outcomes. Recovery is a journey that typically involves several phases, with personalized care plans to ensure comprehensive rehabilitation.</p><h3>Immediate Post-operative Period (Hospital Stay):</h3><ul><li><strong>Duration:</strong> Typically 3-7 days, depending on individual progress and surgical complexity.</li><li><strong>Pain Management:</strong> Managed with medication to ensure comfort and facilitate early mobilization.</li><li><strong>Early Mobilization:</strong> Patients are encouraged to begin gentle movement and standing with assistance, often on the day of surgery or the day after, to prevent complications like blood clots.</li><li><strong>Physical Therapy:</strong> Initiated in the hospital with exercises to improve range of motion and strength.</li></ul><h3>Early Home Recovery (First 6-12 Weeks):</h3><ul><li><strong>Physical Therapy (PT):</strong> This is the cornerstone of recovery. A structured <code>rehabilitation therapy for Revision Knee Replacement</code> program is essential, often several times a week. Exercises focus on strengthening the quadriceps and hamstrings, improving flexibility, and restoring gait.</li><li><strong>Weight-Bearing:</strong> May be limited initially, progressing as tolerated based on surgeon's recommendations and the type of revision.</li><li><strong>Wound Care:</strong> Maintaining incision hygiene and monitoring for signs of infection.</li><li><strong>Activity Restrictions:</strong> Avoiding heavy lifting, twisting, and high-impact activities.</li></ul><h3>Long-term Recovery (3-12 Months and Beyond):</h3><ul><li><strong>Continued PT/Home Exercises:</strong> Maintaining strength and flexibility is vital.</li><li><strong>Gradual Return to Activities:</strong> Most patients can resume light activities, driving, and work within 3 months. Full recovery and return to more strenuous activities can take up to a year or more, especially for complex revisions.</li><li><strong>Lifestyle Modifications:</strong> Maintaining a healthy weight, avoiding falls, and engaging in low-impact exercises are key for the longevity of the implant.</li><li><strong>Follow-up Appointments:</strong> Regular check-ups with your orthopedic surgeon are necessary to monitor the implant and overall knee health.</li></ul><p>DivinHeal supports you through every phase, coordinating access to expert physical therapists and providing resources for a successful and comprehensive recovery from your <code>Revision Knee Replacement treatment</code>.</p>

Revision Hip Replacement
Treatment Price
$8000.00 USDOverview of Revision Hip Replacement
Revision Hip Replacement surgery aims to address the failure of a prior total hip replacement. This procedure involves removing some or all of the original implant components and replacing them with new ones. The goals are to alleviate pain, improve hip function, correct instability, and enhance the overall longevity of the hip joint. Often requiring specialized implants, bone grafting, and meticulous surgical planning, it's a highly individualized treatment focused on restoring optimal mobility and quality of life for patients experiencing complications from their primary hip replacement.
Overview of Revision Hip Replacement
Revision Hip Replacement surgery aims to address the failure of a prior total hip replacement. This procedure involves removing some or all of the original implant components and replacing them with new ones. The goals are to alleviate pain, improve hip function, correct instability, and enhance the overall longevity of the hip joint. Often requiring specialized implants, bone grafting, and meticulous surgical planning, it's a highly individualized treatment focused on restoring optimal mobility and quality of life for patients experiencing complications from their primary hip replacement.
Treatment Overview
<h2>Overview of Revision Hip Replacement</h2><p>Revision Hip Replacement surgery aims to address the failure of a prior total hip replacement. This procedure involves removing some or all of the original implant components and replacing them with new ones. The goals are to alleviate pain, improve hip function, correct instability, and enhance the overall longevity of the hip joint. Often requiring specialized implants, bone grafting, and meticulous surgical planning, it's a highly individualized treatment focused on restoring optimal mobility and quality of life for patients experiencing complications from their primary hip replacement.</p>
Procedures
The Revision Hip Replacement procedure is a complex surgical intervention that typically involves several key steps: 1. **Pre-operative Planning:** Before surgery, detailed imaging (X-rays, CT scans) is performed to assess the extent of bone loss, identify the exact location of failed components, and plan for specialized implants or bone grafting. 2. **Incision and Exposure:** The surgeon makes an incision, often similar to the original one, to access the hip joint. Extensive care is taken to navigate through scar tissue from the previous surgery. 3. **Removal of Old Components:** The existing hip implant components (femoral stem, acetabular cup, and liner) are carefully removed. This can be challenging if components are well-fixed or if significant bone ingrowth has occurred. Specialized instruments are used to extract implants without causing further bone damage. 4. **Debridement and Bone Preparation:** If infection is present, a thorough debridement (cleaning) of the infected tissue is performed. The remaining bone is meticulously prepared, removing any cement, scar tissue, or unhealthy bone. Any bone defects are identified and prepared for grafting. 5. **Bone Grafting (if necessary):** For patients with significant bone loss, bone grafting (using the patient's own bone, donor bone, or synthetic bone substitutes) may be performed to rebuild and strengthen the bone around the hip joint, providing a stable foundation for the new implants. 6. **Insertion of New Implants:** New, often larger or custom-designed, acetabular (socket) and femoral (stem) components are carefully implanted. The new components are fixed using cement, cementless techniques, or a combination, depending on bone quality and surgeon preference. The appropriate head size and liner are then inserted to ensure stability and proper joint mechanics. 7. **Closure:** The surgeon checks the stability and range of motion of the new joint. The muscle layers and skin are then closed with sutures or staples. A drain may be placed to collect excess fluid.
Benefits
<h2>Key Benefits of Revision Hip Replacement</h2><p>Successfully undergoing a <strong>Revision Hip Replacement</strong> can bring transformative benefits, significantly improving the quality of life for patients who have experienced complications with a primary hip replacement. The primary advantages include:</p><ul><li><strong>Significant Pain Relief:</strong> Eliminating the source of pain caused by a loose, infected, or failing implant, allowing for a more comfortable daily existence.</li><li><strong>Restored Mobility and Function:</strong> Improving the range of motion and stability of the hip joint, enabling patients to walk, stand, and perform daily activities with greater ease and confidence.</li><li><strong>Correction of Underlying Issues:</strong> Addressing specific problems like recurrent dislocations, periprosthetic fractures, implant wear, or infection, thereby preventing further complications.</li><li><strong>Enhanced Quality of Life:</strong> Regaining independence, participating in desired activities, and experiencing a substantial improvement in overall well-being and psychological health.</li><li><strong>Increased Implant Longevity:</strong> Modern revision techniques and advanced implants are designed to provide a durable solution, aiming for many more years of functional hip health.</li><li><strong>Improved Stability:</strong> Correcting issues of instability and preventing future dislocations, which can be a debilitating complication of failed primary replacements.</li></ul><p>DivinHeal connects you with expert orthopedic surgeons who are dedicated to achieving the best possible outcomes for your revision hip replacement, focusing on long-term success and patient satisfaction.</p>
Recovery Information
<h2>Revision Hip Replacement Recovery Time and Tips</h2><p>Recovery from <strong>Revision Hip Replacement surgery</strong> is often more involved than a primary hip replacement and requires patience and adherence to medical advice. While individual recovery times vary, here's a general outline:</p><ul><li><h3>Immediate Post-Operative Period (Hospital Stay: 5-7 Days)</h3><p>You'll begin gentle mobilization within 24-48 hours. Pain management is crucial, and physical therapists will guide you through initial exercises to prevent complications like blood clots and muscle stiffness. You'll learn how to safely move in bed, sit, stand, and use walking aids.</p></li><li><h3>Early Recovery (First 6-12 Weeks Post-Discharge)</h3><p>This phase focuses on intense physical therapy. You'll work on strengthening the muscles around your new hip, improving your range of motion, and gradually increasing your mobility. Weight-bearing restrictions may be in place, and you'll continue using crutches or a walker. Driving is typically restricted for several weeks. Adhering to hip precautions (avoiding extreme bending, twisting, or crossing legs) is vital to prevent dislocation.</p></li><li><h3>Long-Term Recovery (3-12 Months)</h3><p>Gradually, you'll transition to more advanced exercises and activities. Most patients can resume light daily activities by 3-6 months. Full recovery, including the ability to return to more demanding activities, can take up to a year or longer, as bone healing and muscle strengthening continue. Consistent engagement in your physical therapy program is key to optimizing outcomes.</p></li></ul><h3>Key Recovery Tips:</h3><ul><li><strong>Follow Physical Therapy Diligently:</strong> This is the most critical component of your recovery.</li><li><strong>Manage Pain Effectively:</strong> Communicate with your medical team to ensure adequate pain control.</li><li><strong>Prevent Infection:</strong> Follow wound care instructions carefully.</li><li><strong>Maintain a Healthy Diet:</strong> Good nutrition supports healing.</li><li><strong>Arrange for Home Support:</strong> Help with daily tasks can be invaluable in the initial weeks.</li><li><strong>Be Patient:</strong> Recovery is a marathon, not a sprint. Celebrate small victories and avoid rushing the process.</li></ul><p>DivinHeal’s comprehensive care coordination extends through your recovery, ensuring you have access to rehabilitation support and guidance for a smooth and successful return to an active life.</p>

Arthroscopic Meniscus Repair / Meniscectomy
Treatment Price
$3000.00 USDOverview of Arthroscopic Meniscus Surgery
Arthroscopic meniscus surgery encompasses two primary approaches: repair and meniscectomy. The goal is to alleviate knee pain, restore stability, and improve mobility caused by a torn meniscus. Using a small camera (arthroscope) and specialized instruments, surgeons can either trim away the damaged meniscus tissue (meniscectomy) or suture the torn edges back together (repair). The choice depends on the tear's location, size, pattern, and the patient's age and activity level.
Overview of Arthroscopic Meniscus Surgery
Arthroscopic meniscus surgery encompasses two primary approaches: repair and meniscectomy. The goal is to alleviate knee pain, restore stability, and improve mobility caused by a torn meniscus. Using a small camera (arthroscope) and specialized instruments, surgeons can either trim away the damaged meniscus tissue (meniscectomy) or suture the torn edges back together (repair). The choice depends on the tear's location, size, pattern, and the patient's age and activity level.
Treatment Overview
<h2>Overview of Arthroscopic Meniscus Surgery</h2><p>Arthroscopic meniscus surgery encompasses two primary approaches: repair and meniscectomy. The goal is to alleviate knee pain, restore stability, and improve mobility caused by a torn meniscus. Using a small camera (arthroscope) and specialized instruments, surgeons can either trim away the damaged meniscus tissue (meniscectomy) or suture the torn edges back together (repair). The choice depends on the tear's location, size, pattern, and the patient's age and activity level.</p>
Procedures
Arthroscopic meniscus surgery is performed under regional or general anesthesia. The surgeon makes two or three small incisions (portals) around the knee joint. An arthroscope, a thin tube with a camera, is inserted through one incision to visualize the inside of the joint on a monitor. Saline solution is continuously pumped into the joint to expand it and improve visibility. Specialized surgical instruments are then inserted through the other incisions. For a meniscectomy, the damaged or torn portion of the meniscus is carefully trimmed and removed. For a meniscus repair, the torn edges are sutured together using various techniques, sometimes involving anchors or all-inside repair devices. Once the procedure is complete, the instruments are removed, and the small incisions are closed with sutures or sterile strips and covered with dressings.
Benefits
<h2>Benefits of Arthroscopic Meniscus Repair / Meniscectomy</h2><p>Choosing Arthroscopic Meniscus Repair or Meniscectomy offers numerous advantages for patients suffering from meniscus tears:</p><ul><li><h3>Pain Relief and Improved Function</h3><ul><li>Significantly reduces knee pain and discomfort.</li><li>Restores normal knee movement and stability.</li></ul></li><li><h3>Minimally Invasive Approach</h3><ul><li>Arthroscopy involves small incisions, leading to less tissue damage.</li><li>Faster healing and reduced scarring compared to traditional open surgery.</li></ul></li><li><h3>Quicker Recovery Time</h3><ul><li>Shorter hospital stays, often an outpatient procedure.</li><li>Patients can typically return to daily activities and work sooner (meniscectomy).</li></ul></li><li><h3>Preservation of Knee Health (Repair)</h3><ul><li>Meniscus repair aims to save the natural cartilage, which is crucial for long-term knee health and potentially delays the onset of arthritis.</li></ul></li><li><h3>High Success Rates</h3><ul><li>Both procedures boast high success rates in relieving symptoms and improving quality of life, especially when combined with diligent rehabilitation.</li></ul></li><li><h3>Personalized Treatment</h3><ul><li>The surgical approach is tailored to the specific type and location of the tear, ensuring the most effective outcome for each patient.</li></ul></li></ul>
Recovery Information
<h2>Recovery and Rehabilitation After Arthroscopic Meniscus Surgery</h2><p>Recovery time for Arthroscopic Meniscus Repair / Meniscectomy varies significantly depending on the specific procedure performed (repair vs. meniscectomy), the individual's overall health, and adherence to rehabilitation protocols.</p><ul><li><h3>Immediate Post-operative Period (Days 1-7)</h3><ul><li>You will typically be discharged the same day or the following day.</li><li>Initial focus is on pain management (medication, RICE protocol - Rest, Ice, Compression, Elevation).</li><li>Weight-bearing restrictions may apply, especially after a meniscus repair (crutches for 4-6 weeks). Meniscectomy often allows partial weight-bearing sooner.</li><li>Gentle range-of-motion exercises may begin under therapist guidance.</li></ul></li><li><h3>Early Rehabilitation (Weeks 1-6)</h3><ul><li>Physical therapy is crucial. It focuses on restoring knee range of motion, reducing swelling, and strengthening surrounding muscles.</li><li>A knee brace may be worn for protection, particularly after a repair.</li><li>Avoid twisting or squatting movements.</li></ul></li><li><h3>Advanced Rehabilitation (Weeks 6-12+)</h3><ul><li>Gradual progression to more intense strengthening exercises.</li><li>Introduction of balance and proprioception training.</li><li>For meniscus repair, return to light activities may begin around 3-4 months, with full return to sports 6-9 months, depending on surgeon's advice and tear healing.</li><li>For meniscectomy, return to light activities might be 2-3 months, and sports 4-6 months.</li></ul></li></ul><p>Adhering to your physical therapy program and following your surgeon's instructions are paramount for optimal recovery and long-term success after Arthroscopic Meniscus Repair / Meniscectomy.</p>
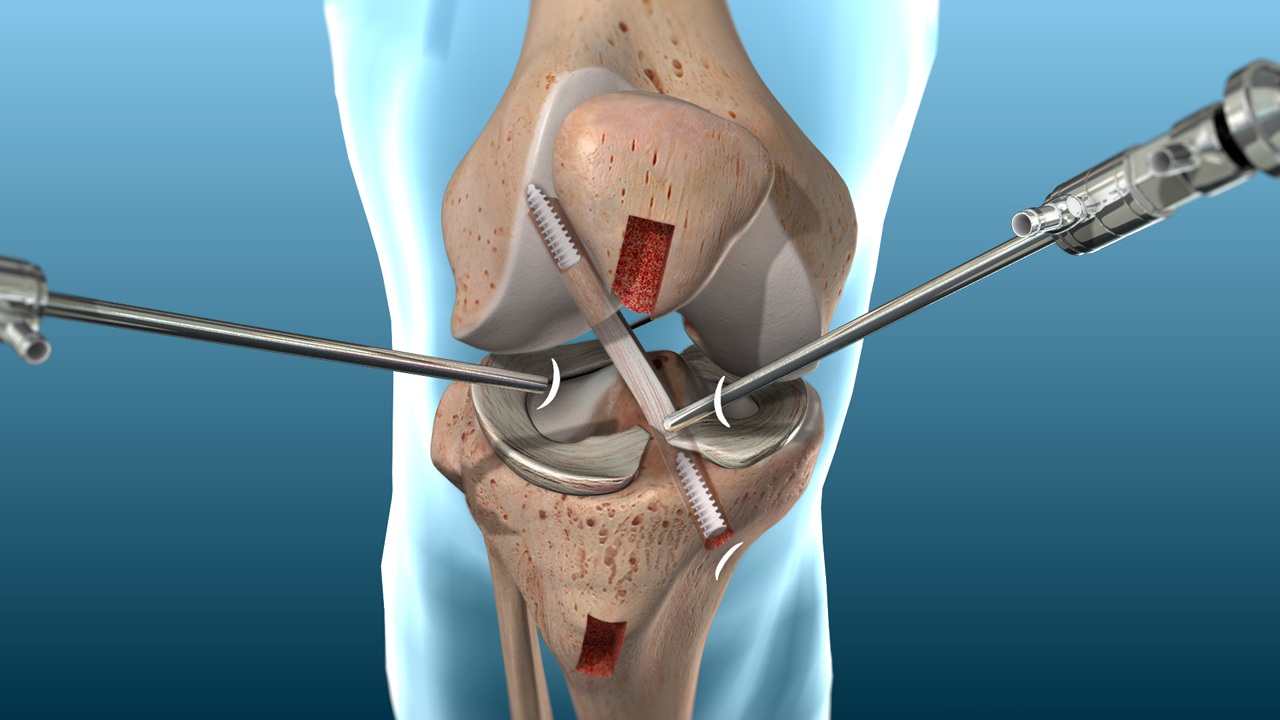
Arthroscopic ACL Reconstruction
Treatment Price
$4000.00 USDThe primary goal of Arthroscopic ACL Reconstruction is to restore stability to the knee joint, reduce pain, and enable patients to return to their desired activity levels, especially sports. The procedure involves making small incisions to insert an arthroscope (a small camera) and surgical instruments. The torn ACL is removed, and a new ligament graft is secured in place using screws or other fixation devices, mimicking the original ACL's function. This advanced technique minimizes recovery time and post-operative discomfort compared to traditional open surgery.
The primary goal of Arthroscopic ACL Reconstruction is to restore stability to the knee joint, reduce pain, and enable patients to return to their desired activity levels, especially sports. The procedure involves making small incisions to insert an arthroscope (a small camera) and surgical instruments. The torn ACL is removed, and a new ligament graft is secured in place using screws or other fixation devices, mimicking the original ACL's function. This advanced technique minimizes recovery time and post-operative discomfort compared to traditional open surgery.
Treatment Overview
<p>The primary goal of Arthroscopic ACL Reconstruction is to restore stability to the knee joint, reduce pain, and enable patients to return to their desired activity levels, especially sports. The procedure involves making small incisions to insert an arthroscope (a small camera) and surgical instruments. The torn ACL is removed, and a new ligament graft is secured in place using screws or other fixation devices, mimicking the original ACL's function. This advanced technique minimizes recovery time and post-operative discomfort compared to traditional open surgery.</p>
Procedures
Arthroscopic ACL reconstruction typically involves these steps: 1. Anesthesia: General or regional anesthesia is administered. 2. Incisions: Several small incisions (portals) are made around the knee. 3. Arthroscopy: An arthroscope (a small camera) is inserted to visualize the knee joint on a monitor. 4. Graft Harvest (if autograft): A portion of the patellar tendon, hamstring tendon, or quadriceps tendon is harvested. If an allograft is used, this step is skipped. 5. Torn ACL Removal: The remnants of the torn ACL are removed. 6. Tunnel Creation: Tunnels are drilled in the tibia and femur bones at the precise locations where the original ACL attached. 7. Graft Passage & Fixation: The prepared graft is threaded through the bone tunnels and secured with fixation devices (e.g., screws, staples, buttons) at both ends. 8. Closure: Incisions are closed with sutures or sterile strips, and a sterile dressing is applied.
Benefits
<p><h3>Key Benefits of Arthroscopic ACL Reconstruction</h3><ul><li><strong>Restored Knee Stability:</strong> Effectively prevents the knee from 'giving way', crucial for daily activities and sports.</li><li><strong>Pain Reduction:</strong> Alleviates chronic pain associated with an unstable knee joint.</li><li><strong>Return to Activity:</strong> Allows patients to safely return to their pre-injury activity levels, including competitive sports.</li><li><strong>Minimally Invasive:</strong> Smaller incisions lead to less scarring, reduced post-operative pain, and a quicker initial recovery.</li><li><strong>Reduced Risk of Future Injuries:</strong> Stabilizing the knee helps protect other structures like the meniscus and cartilage from further damage.</li><li><strong>Improved Quality of Life:</strong> Regaining full knee function significantly enhances overall physical and emotional well-being.</li></ul></p>
Recovery Information
<p><h3>Recovery After Arthroscopic ACL Reconstruction</h3><p>Recovery from Arthroscopic ACL Reconstruction is a gradual process that typically spans 6-9 months, with full return to sports often taking up to a year. It's heavily reliant on a disciplined physical therapy program.</p><ul><li><strong>Initial Phase (Weeks 1-2):</strong> Focus on pain and swelling management, protecting the graft, achieving full knee extension, and gentle flexion. Crutches are used, and bracing may be prescribed.</li><li><strong>Intermediate Phase (Weeks 3-12):</strong> Gradual increase in weight-bearing, strengthening exercises for quadriceps and hamstrings, improving range of motion, and light cardiovascular activities.</li><li><strong>Advanced Phase (Months 3-6):</strong> Introduction of more intense strength training, balance and proprioception exercises, and sport-specific drills.</li><li><strong>Return to Sport Phase (Months 6-9+):</strong> Clearance for full return to sports activities after meeting specific strength, stability, and functional criteria, ensuring the new ligament is mature and robust enough to handle the stresses.</li></ul><p>Adherence to your physical therapist's guidelines and the surgeon's recommendations is paramount for a successful outcome and to prevent re-injury.</p></p>
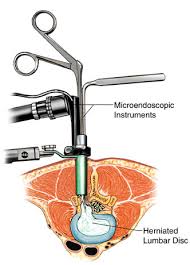
Minimally Invasive Spine Surgery
Treatment Price
$4000.00 USDThe primary goal of Minimally Invasive Spine Surgery is to alleviate chronic back and neck pain, neurological deficits, and instability caused by conditions such as herniated discs, spinal stenosis, and spondylolisthesis. Techniques involve the use of tubular retractors, endoscopes, and microscopes, allowing surgeons to access the spine through tiny openings. This innovative approach minimizes blood loss, lowers infection risk, and significantly shortens hospital stays, accelerating the patient's return to normal activities.
The primary goal of Minimally Invasive Spine Surgery is to alleviate chronic back and neck pain, neurological deficits, and instability caused by conditions such as herniated discs, spinal stenosis, and spondylolisthesis. Techniques involve the use of tubular retractors, endoscopes, and microscopes, allowing surgeons to access the spine through tiny openings. This innovative approach minimizes blood loss, lowers infection risk, and significantly shortens hospital stays, accelerating the patient's return to normal activities.
Treatment Overview
The primary goal of Minimally Invasive Spine Surgery is to alleviate chronic back and neck pain, neurological deficits, and instability caused by conditions such as herniated discs, spinal stenosis, and spondylolisthesis. Techniques involve the use of tubular retractors, endoscopes, and microscopes, allowing surgeons to access the spine through tiny openings. This innovative approach minimizes blood loss, lowers infection risk, and significantly shortens hospital stays, accelerating the patient's return to normal activities.
Procedures
Minimally Invasive Spine Surgery typically begins with the patient under general anesthesia. Small incisions, often less than an inch, are made on the back. A specialized tubular retractor is then inserted through the incision, creating a working channel to the spine while gently pushing muscle tissue aside rather than cutting it. A small camera (endoscope) or microscope is inserted through the tube, providing magnified, high-definition views of the surgical area on a monitor. Specialized long, thin instruments are then passed through the tube to perform the required procedure, such as removing a herniated disc, decompressing nerves, or fusing vertebrae. Once the objective is achieved, the instruments and retractor are removed, and the small incision is closed with sutures or surgical tape.
Benefits
<h2>Benefits of Minimally Invasive Spine Surgery</h2><ul><li><h3>Reduced Pain</h3><p>Smaller incisions and less muscle disruption lead to significantly less post-operative pain.</p></li><li><h3>Faster Recovery Time</h3><p>Patients typically experience a quicker return to normal activities and shorter hospital stays.</p></li><li><h3>Lower Infection Risk</h3><p>Minimal tissue exposure during surgery reduces the chance of post-operative infections.</p></li><li><h3>Less Blood Loss</h3><p>Smaller incisions minimize surgical bleeding, often avoiding the need for transfusions.</p></li><li><h3>Minimal Scarring</h3><p>Tiny incisions result in less visible scars, improving cosmetic outcomes.</p></li><li><h3>Preservation of Spinal Stability</h3><p>Less damage to surrounding muscles and ligaments helps maintain spinal integrity.</p></li><li><h3>High Success Rates</h3><p>Effective in treating a wide range of spinal conditions with excellent patient outcomes.</p></li></ul>
Recovery Information
<h2>Recovery After Minimally Invasive Spine Surgery</h2><p>Recovery from Minimally Invasive Spine Surgery (MISS) is generally faster and less painful than traditional open surgery. Patients typically spend 1-3 days in the hospital. The initial recovery phase, involving pain management and basic mobility, usually lasts 1-6 weeks. During this time, gentle walking is encouraged, and strenuous activities are avoided.</p><p>Physical therapy is a crucial component of long-term recovery, often starting a few weeks post-surgery. Therapists guide patients through exercises to strengthen core muscles, improve flexibility, and restore proper body mechanics. Full recovery and return to all pre-surgery activities can take anywhere from 3 to 6 months, depending on the individual's condition, the type of surgery performed, and adherence to rehabilitation protocols. DivinHeal provides continuous support and guidance throughout your recovery journey, connecting you with rehabilitation specialists and ensuring access to necessary resources for optimal healing.</p>

Robotic Knee Replacement Surgery
Treatment Price
$7500.00 USDRobotic Knee Replacement Surgery aims to alleviate chronic knee pain, restore mobility, and improve quality of life for individuals with debilitating knee conditions like osteoarthritis. By integrating sophisticated robotic technology, surgeons create a personalized 3D plan pre-operatively and execute the surgery with remarkable accuracy, ensuring optimal bone preparation and implant alignment.
Robotic Knee Replacement Surgery aims to alleviate chronic knee pain, restore mobility, and improve quality of life for individuals with debilitating knee conditions like osteoarthritis. By integrating sophisticated robotic technology, surgeons create a personalized 3D plan pre-operatively and execute the surgery with remarkable accuracy, ensuring optimal bone preparation and implant alignment.
Treatment Overview
Robotic Knee Replacement Surgery aims to alleviate chronic knee pain, restore mobility, and improve quality of life for individuals with debilitating knee conditions like osteoarthritis. By integrating sophisticated robotic technology, surgeons create a personalized 3D plan pre-operatively and execute the surgery with remarkable accuracy, ensuring optimal bone preparation and implant alignment.
Procedures
Robotic Knee Replacement Surgery involves several key steps: 1. **Pre-operative Planning:** A CT scan of the knee creates a 3D virtual model. The surgeon uses this model to meticulously plan the optimal implant size and position, tailoring it to the patient's unique anatomy. 2. **Anesthesia:** The patient receives general or spinal anesthesia. 3. **Incision:** A small incision is made over the knee. 4. **Robotic Guidance:** The robotic arm, guided by the surgeon, assists in preparing the bone for the implant. The system provides real-time feedback, ensuring bone cuts are made with extreme precision according to the pre-operative plan. 5. **Implant Placement:** The custom-selected artificial knee components are precisely cemented into place. 6. **Range of Motion Check:** The surgeon tests the knee's range of motion and stability. 7. **Closure:** The incision is closed with sutures or staples.
Benefits
<ul><li><strong>Exceptional Precision:</strong> Robot-assisted surgery allows for highly accurate bone preparation and implant placement, optimized for your unique anatomy.</li><li><strong>Customized Outcomes:</strong> Personalized surgical planning leads to a knee replacement tailored specifically for your body, enhancing functionality and feel.</li><li><strong>Reduced Pain & Faster Recovery:</strong> Many patients experience less post-operative pain and a quicker return to mobility compared to traditional methods.</li><li><strong>Minimally Invasive:</strong> Often involves smaller incisions, leading to less scarring and potentially reduced blood loss.</li><li><strong>Improved Implant Longevity:</strong> Accurate alignment can prolong the life of your knee implant, reducing the need for revision surgery.</li><li><strong>Enhanced Mobility:</strong> Designed to restore natural knee motion and significantly improve your quality of life.</li></ul>
Recovery Information
Recovery from Robotic Knee Replacement Surgery typically involves a hospital stay of 3-5 days. Patients usually begin physical therapy within 24 hours of surgery, focusing on gentle exercises to restore range of motion and strength. Full recovery, including return to most daily activities, usually takes 3-6 months. Adherence to a prescribed physical therapy regimen is crucial for optimal outcomes. Long-term wellness includes maintaining a healthy weight and engaging in low-impact activities.
Meet Our Doctors
Meet our team of highly qualified and experienced medical professionals dedicated to providing the best healthcare services.

Dinesh Kansal
Director & Head
Orthopaedics
New Delhi
23+ Years
Experience
Apolo Delhi
Hospital
1500
Fees

Dr. Ajit Singh Baghela
Sr. Consultant - Paediatric Neurology
Paediatric Neurology
New Delhi
9+ Years
Experience
Artemis Hospital
Hospital
1500
Fees

Dr. Ambrish Mithal
Chairman and Head of Endocrinology and Diabetes at Max Healthcare, Saket, New Delhi
Endocrinology & Diabetes
New Delhi
36+ Years
Experience
Max Hospital,Gurgaon
Hospital
1500
Fees

Dr. Amit Kalsotra
Sr. Consultant - Anaesthesia, Critical Care & Pain Management
Anaesthesia, Critical Care, Pain Management
New Delhi
15+ Years
Experience
Artemis Hospital
Hospital
1500
Fees

Dr. Anjali Vaish
Consultant - Physiotherapy and Rehabilitation Centre
Physiotherapy and Rehabilitation Centre
New Delhi
10+ Years
Experience
Artemis Hospital
Hospital
1500
Fees

Dr. Anju Singh
Consultant - Pediatric Rheumatology
Pediatric Rheumatology
New Delhi
13+ Years
Experience
Artemis Hospital
Hospital
1500
Fees

Dr. Anurag Krishna
Director & Head of Pediatric Services, Max Healthcare
Pediatric Surgery
New Delhi
30+ Years
Experience
Max Hospital,Gurgaon
Hospital
1500
Fees

Dr. Arvind M Das
Senior Consultant
Orthopaedics
New Delhi
25+ Years
Experience
Apolo Delhi
Hospital
1500
Fees

Dr. Ashish Gautam
Consultant
Orthopaedics
New Delhi
12+ Years
Experience
Apolo Delhi
Hospital
1500
Fees

Dr. Ashish Rai
Director
Orthopaedics
New Delhi
18+ Years
Experience
Apolo Delhi
Hospital
1500
Fees

Dr. B L Agarwal
Senior Consultant - Endocrinology
Endocrinology
New Delhi
40+ Years
Experience
Apolo Delhi
Hospital
1500
Fees
Dr. (Brig.) Anil Khetarpal
Deputy Chief - Medical Services & Chairperson -Department of Blood Centre and Transfusion medicine
Blood Centre & Transfusion Medicine
New Delhi
33+ Years
Experience
Artemis Hospital
Hospital
1500
Fees

Dr. Col Manjit Singh Paul
Director & Chief of Spine Surgery
Orthopaedics
New Delhi
33+ Years
Experience
Apolo Delhi
Hospital
1500
Fees

Dr Deepak Lahoti
Director
Orthopaedics
New Delhi
20+ Years
Experience
Apolo Delhi
Hospital
1500
Fees

Dr. Devavrat Arya
Principal Director - Medical Oncology
Medical Oncology
New Delhi
20+ Years
Experience
Max Hospital,Gurgaon
Hospital
1500
Fees

Dr. Devendra Chaukar
Director - Orthopaedics and Joint Replacement
Orthopaedics and Joint Replacement
New Delhi
29+ Years
Experience
Apolo Delhi
Hospital
1500
Fees

Dr. Dinesh Khullar
Chairman, Department of Nephrology, and Renal Transplant Medicine at Max Super Speciality Hospital, Saket, New Delhi
Nephrology and Renal Transplant Medicine
New Delhi
25+ Years
Experience
Max Hospital,Gurgaon
Hospital
1500
Fees

Dr. Gajanand Yadav
Consultant - Orthopaedics and Hip and Knee Arthroplasty
Orthopaedics, Hip and Knee Arthroplasty, Joint Replacement, Sports Medicine
New Delhi
12+ Years
Experience
Artemis Hospital
Hospital
1500
Fees

Dr. Gaurav Minocha
Director
Orthopaedics & Joint Replacement
New Delhi
17+ Years
Experience
Apolo Delhi
Hospital
1500
Fees

Dr. Harshavardhan Karunakara Hegde
Chairman - Orthopaedics
Orthopaedics and Joint Replacement
New Delhi
40+ Years
Experience
Apolo Delhi
Hospital
1500
Fees